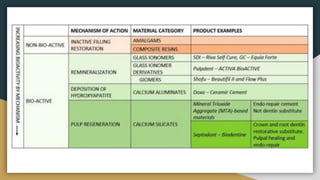
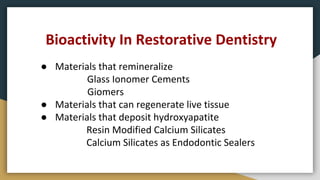
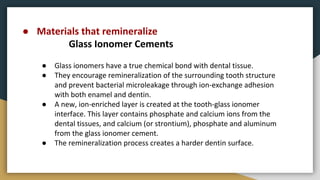
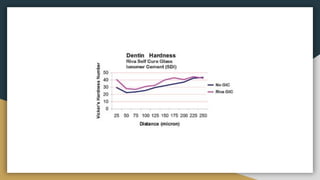
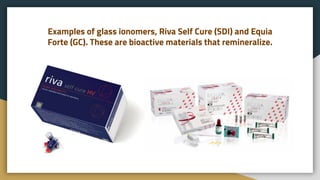
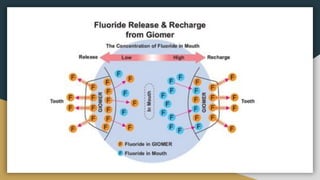
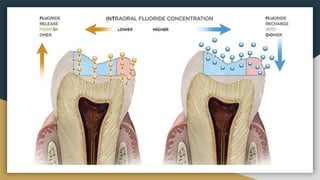
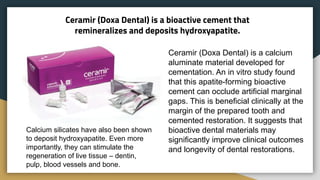
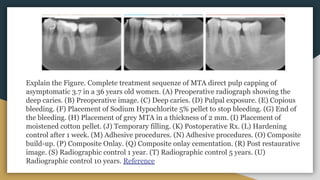
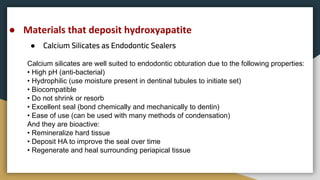
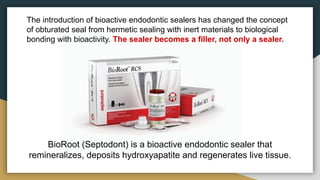
The document discusses the use of bioactive materials in dentistry, highlighting their capabilities to remineralize dental structures and regenerate live tissue. It emphasizes the importance of materials like glass ionomer cements, giomers, calcium silicates, and mineral trioxide aggregate (MTA) in improving clinical outcomes and the longevity of dental restorations. The use of bioactive endodontic sealers marks a shift in dental practice towards biologically active materials that bond with teeth and support tissue regeneration.