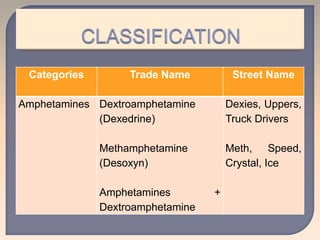
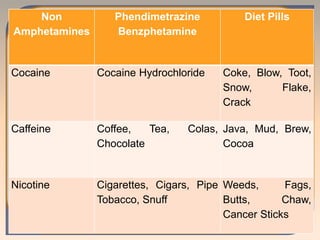
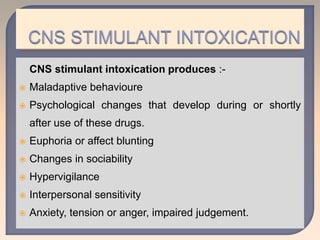
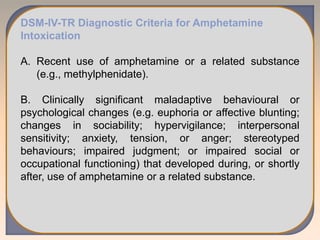
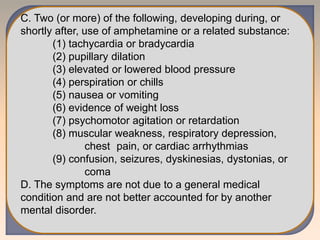
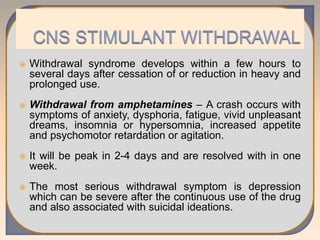
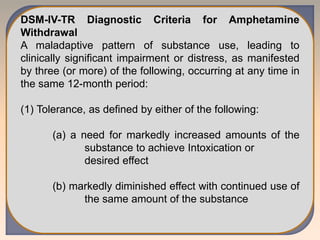
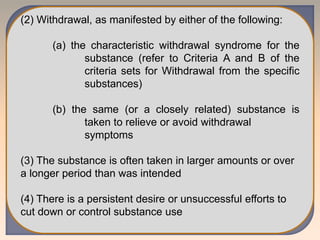
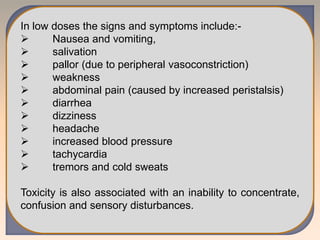
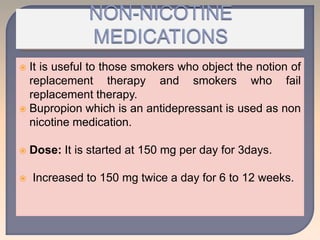
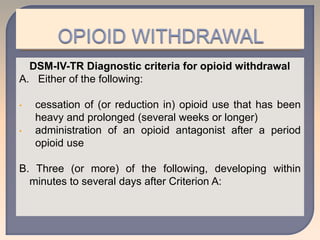
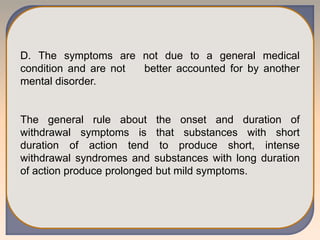
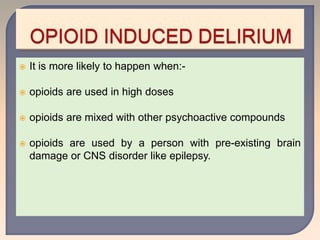
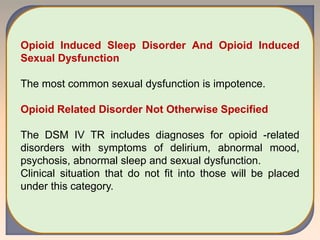
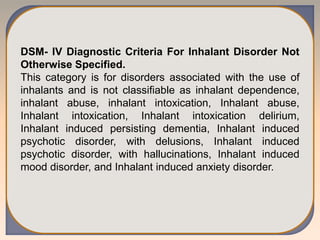
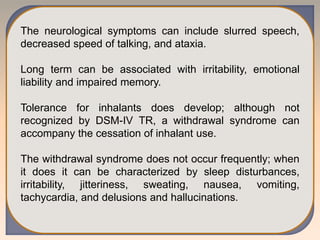
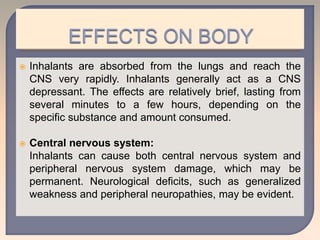
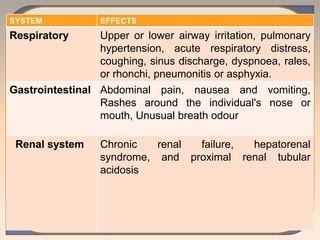
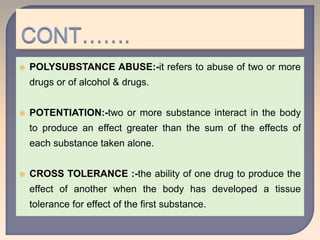
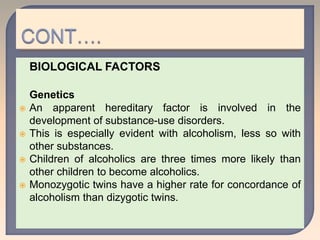
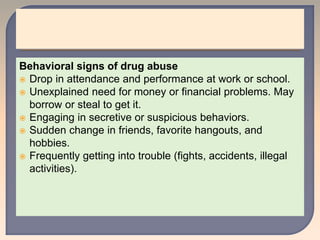
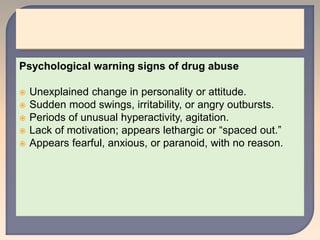
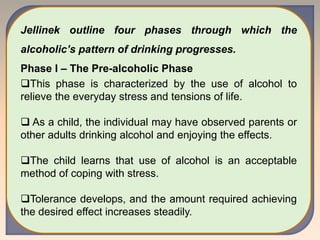
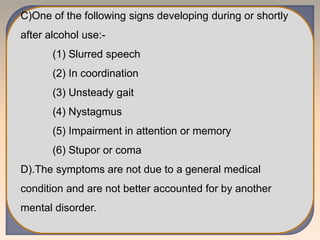
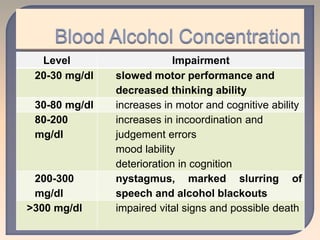
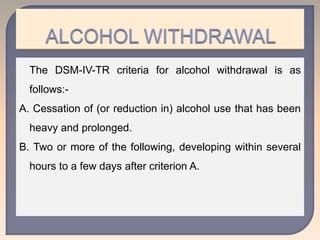
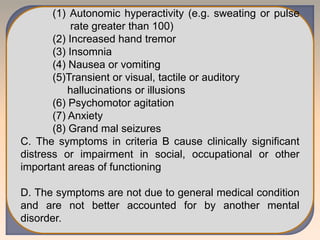
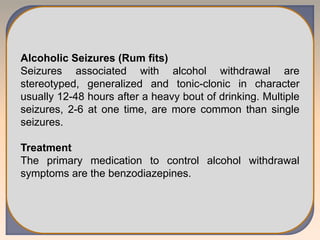
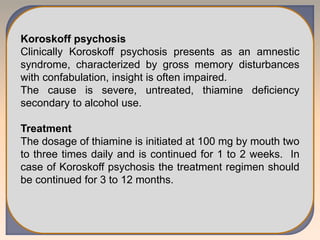
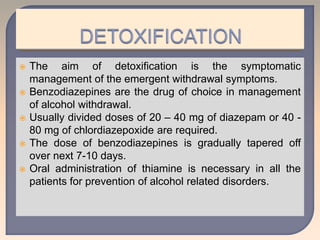
This document discusses substance use disorders and substance abuse. It notes that substance use disorders are composed of substance use disorders (dependence and abuse) and substance induced disorders. Substance abuse is defined as maladaptive substance use with adverse consequences. The document outlines the diagnostic criteria for substance dependence per the DSM and ICD-10, including tolerance, withdrawal symptoms, loss of control over use, and continuing use despite consequences. It also discusses physical and psychological dependence, intoxication, withdrawal, and the various classes of abused substances. Biological, psychological, and socio-cultural factors in substance abuse are examined.



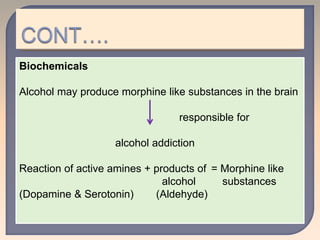









![ In contrast, alcohol intoxication caused a significant
increase in [1-(11)C]acetate brain uptake (measured as
standard uptake value, SUV), with the largest increases
occurring in the cerebellum and the smallest in the
thalamus.](https://image.slidesharecdn.com/substancerelateddisorder-240304025047-47007a6e/85/SUBSTANCE-RELbddddddddATED-DISORDER-pptx-71-320.jpg)