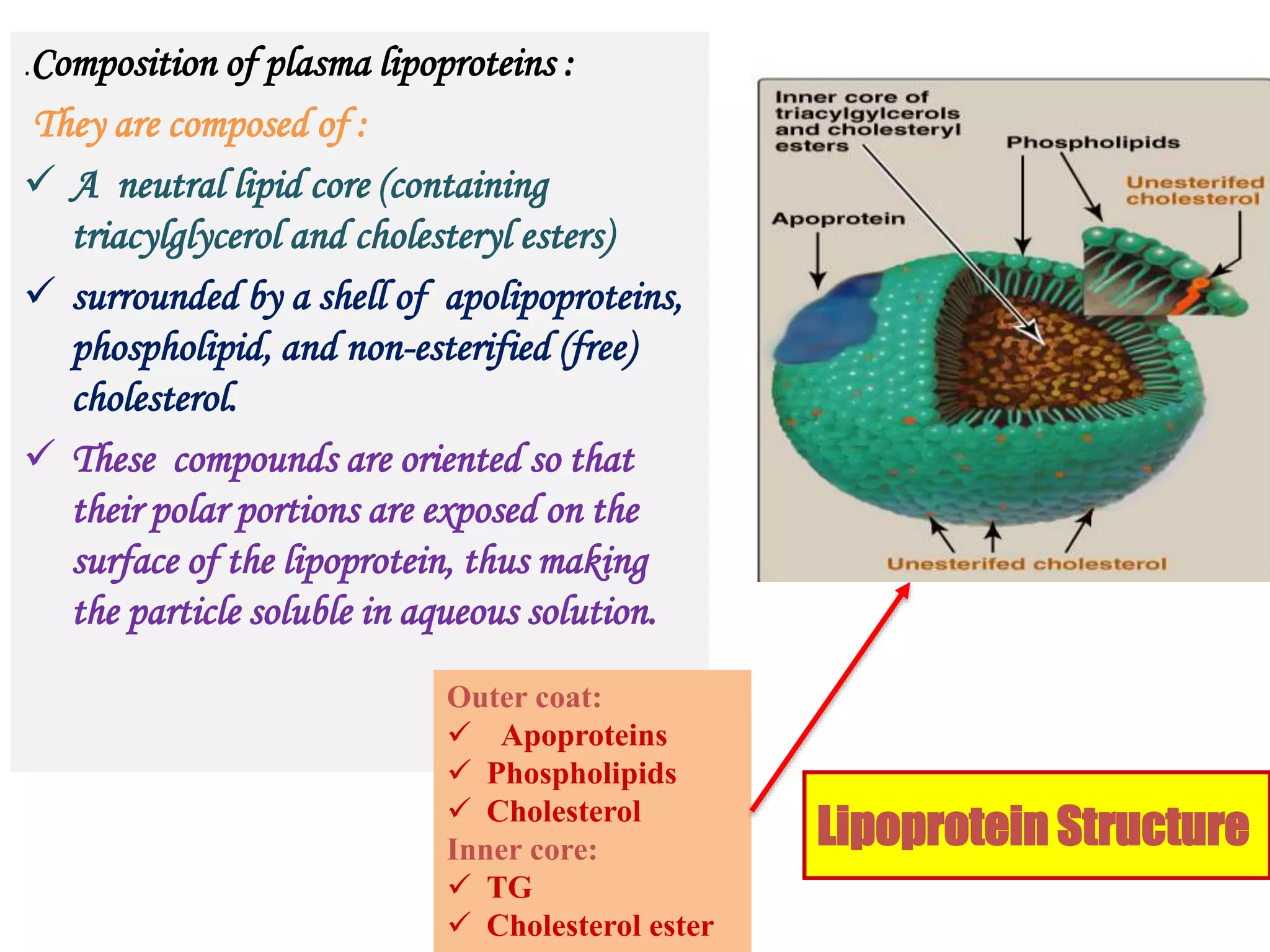
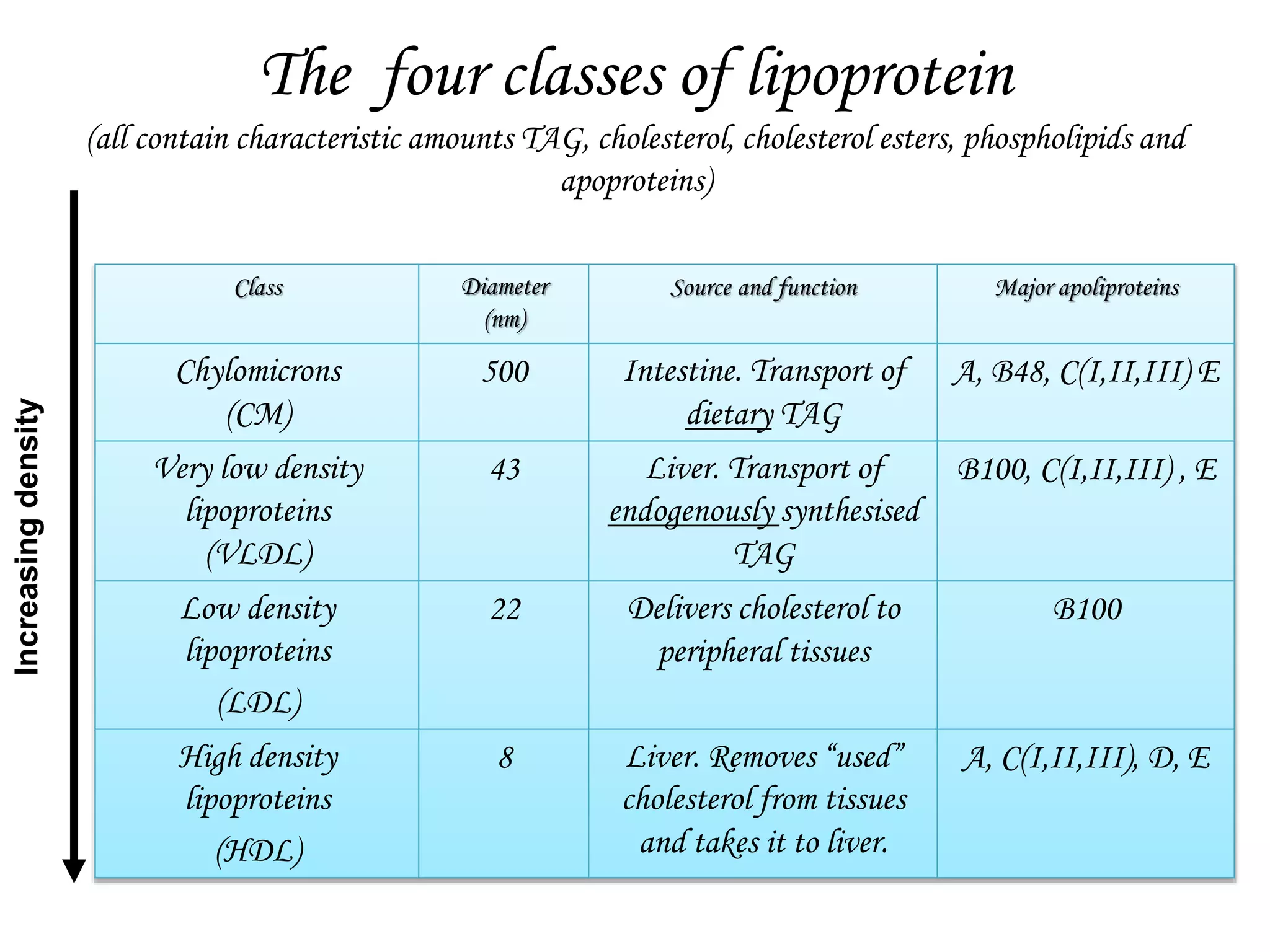
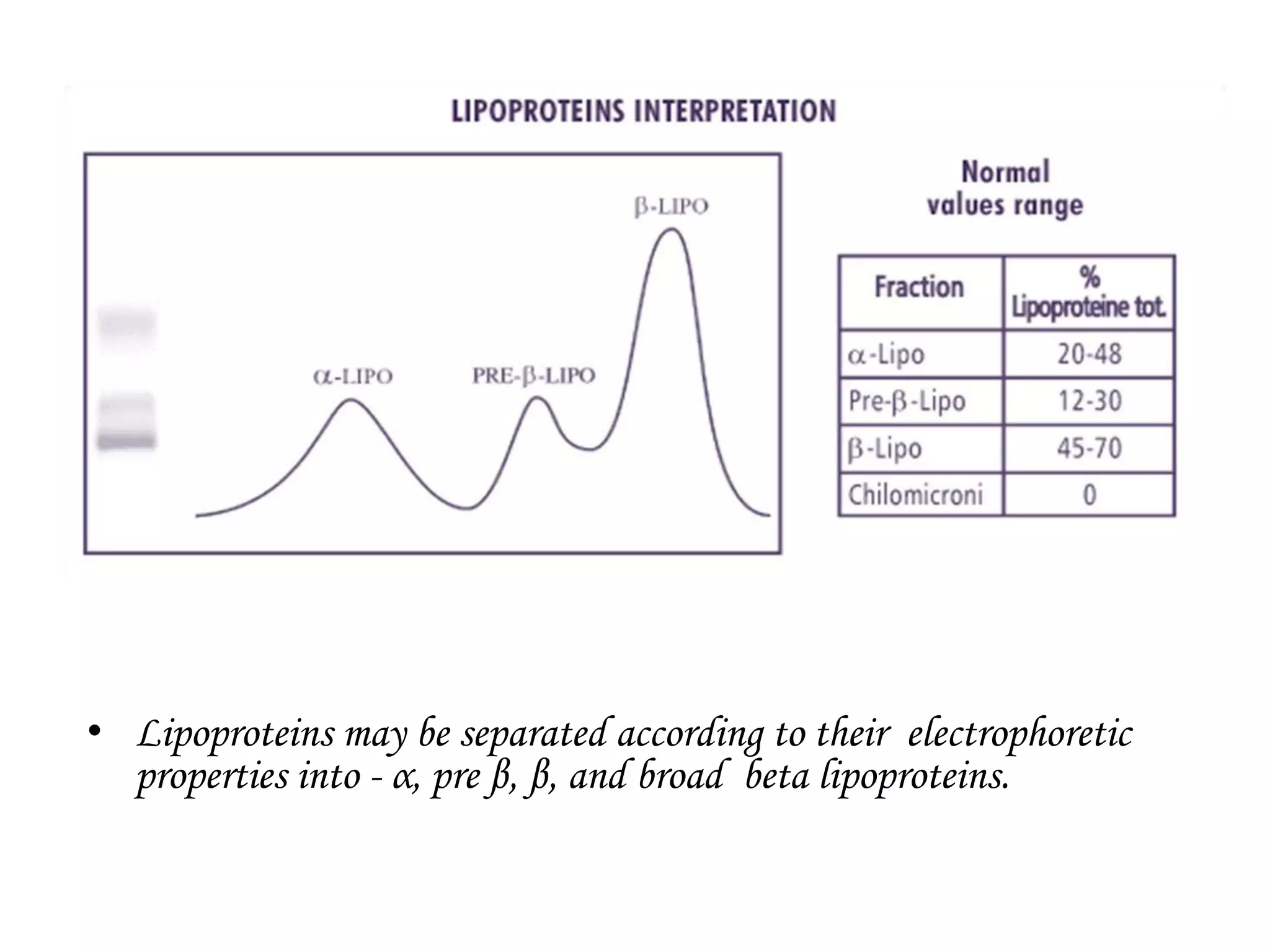
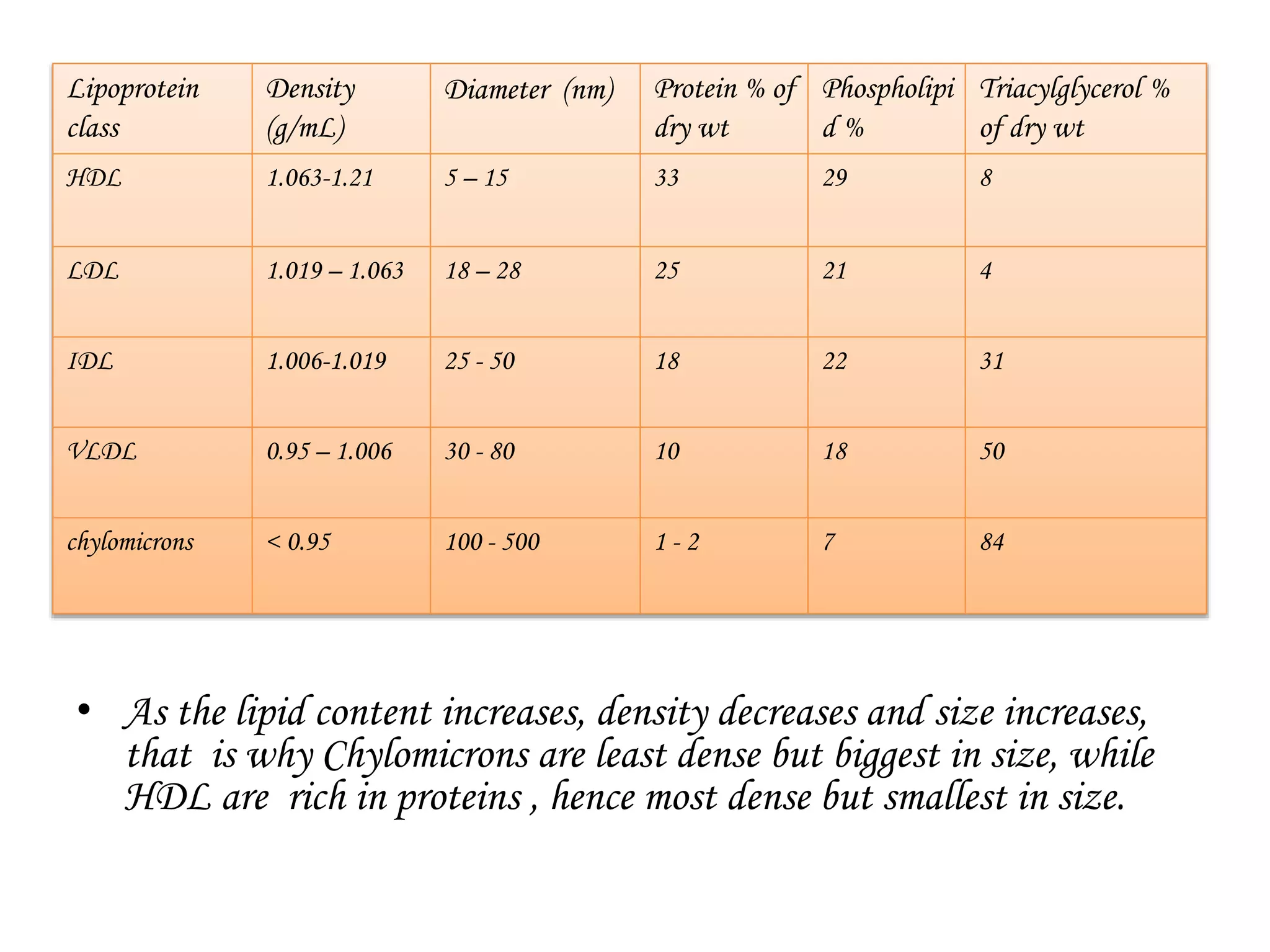
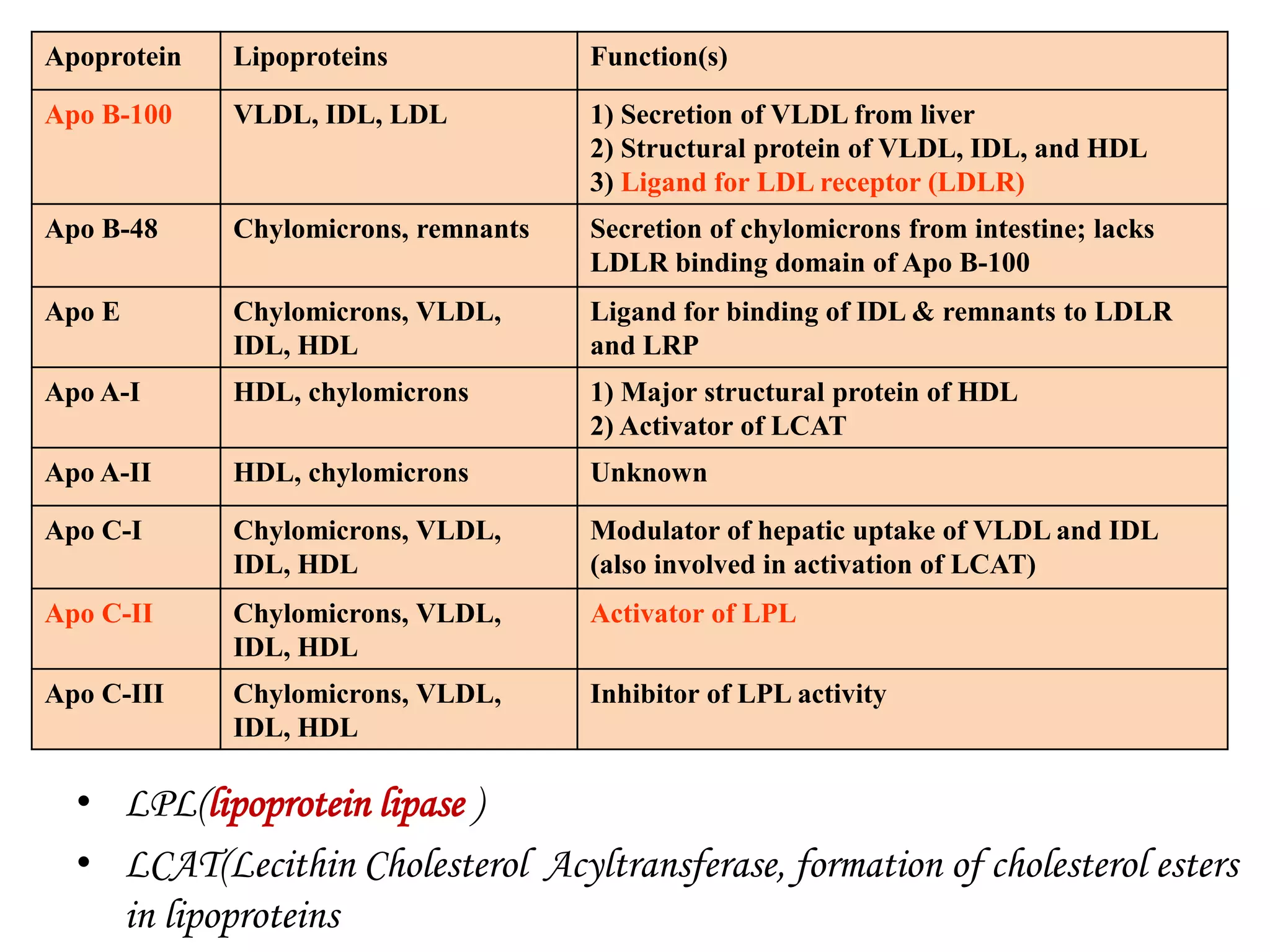
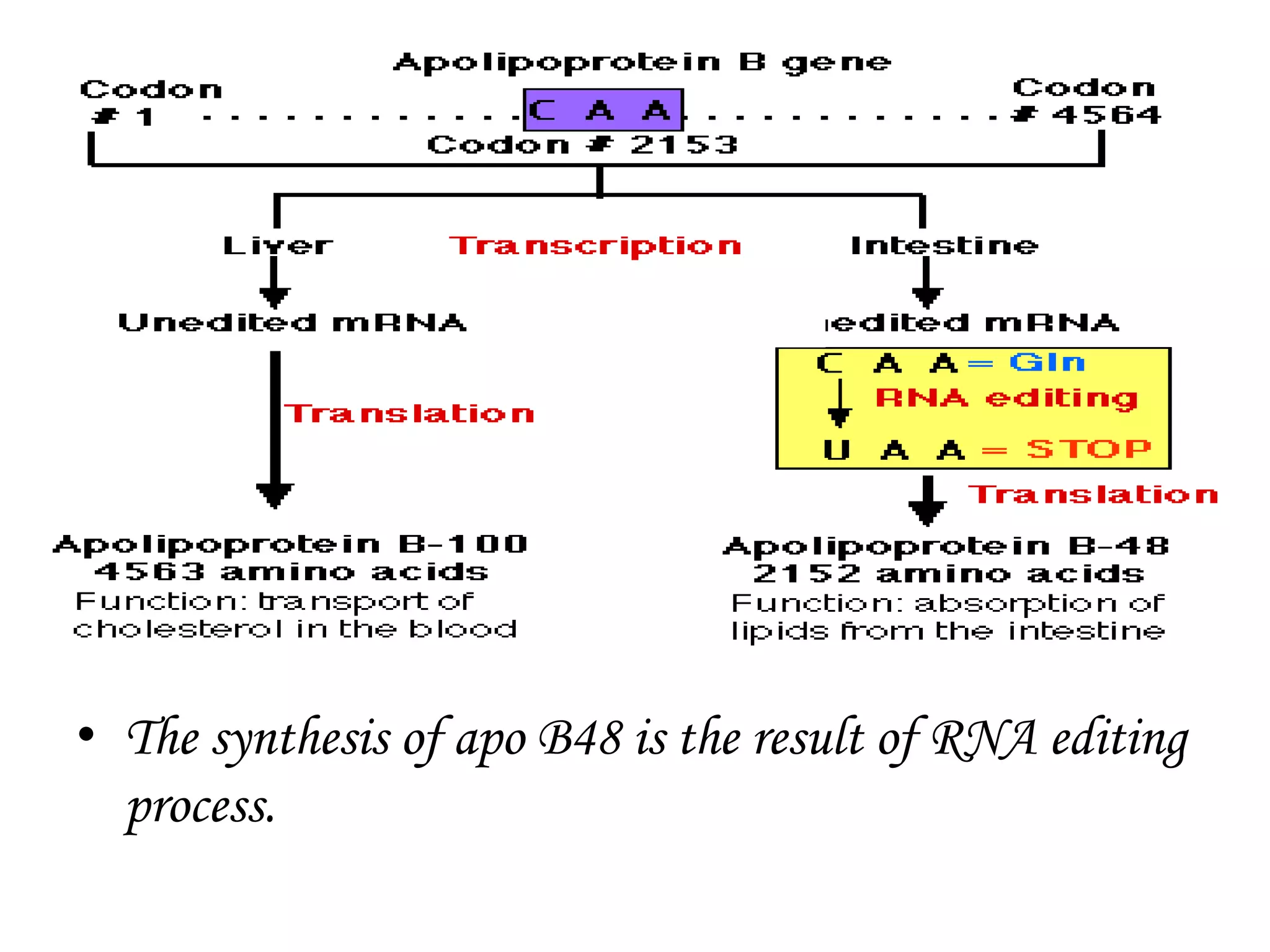
Lipoproteins are complexes of lipids and proteins that transport hydrophobic lipid molecules in blood plasma. They play key roles in lipid absorption, transport, and reverse cholesterol transport. Lipoproteins are classified based on their density and include chylomicrons, VLDL, LDL, IDL, and HDL. They contain characteristic amounts of triglycerides, cholesterol, phospholipids, and apolipoproteins such as Apo B, Apo E, and differ in size, density, and function. Abnormal lipoprotein metabolism can lead to dyslipidemias and diseases like atherosclerosis.