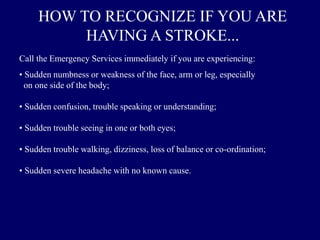
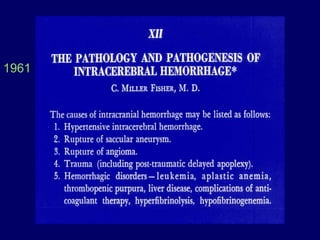
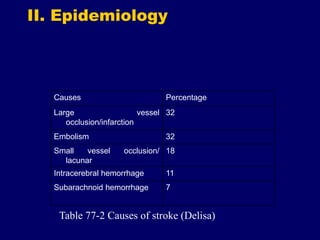
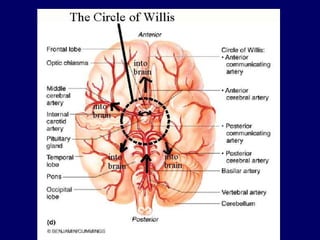
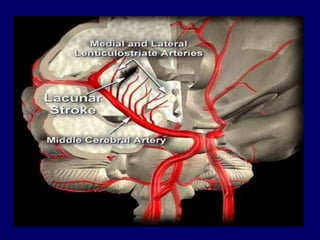
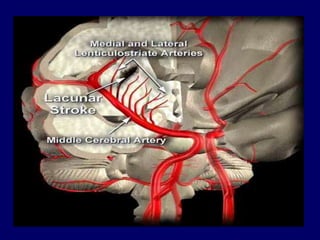
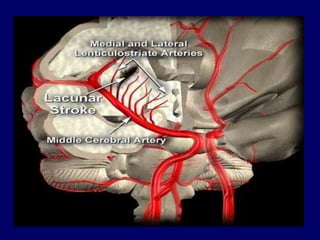
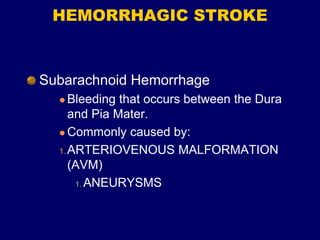
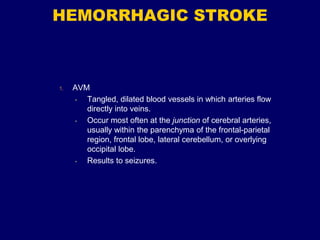
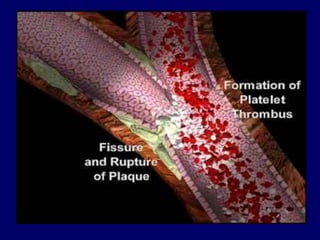
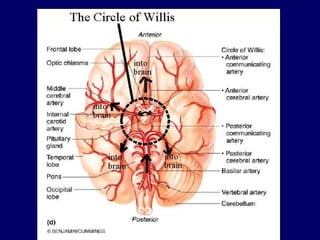
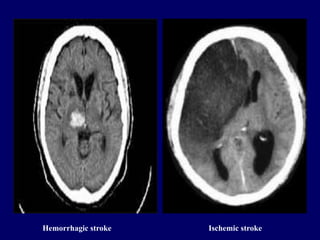
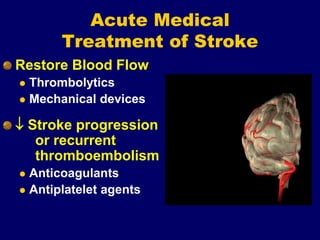
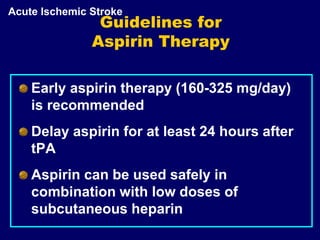
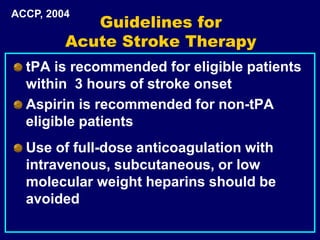
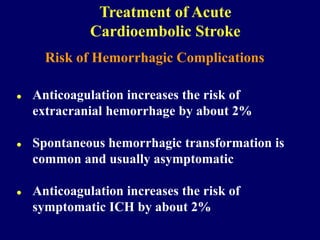
Stroke occurs when a blood vessel that supplies the brain is blocked or ruptures, depriving brain tissue of oxygen and nutrients. The most common type of stroke is ischemic stroke, which accounts for over 80% of cases and occurs when a blood clot blocks an artery. Less common is hemorrhagic stroke, which occurs when a blood vessel ruptures in or near the brain. Risk factors for stroke include high blood pressure, heart disease, diabetes, smoking, obesity, high cholesterol, physical inactivity, and excessive alcohol use. Prompt treatment is crucial for stroke victims.