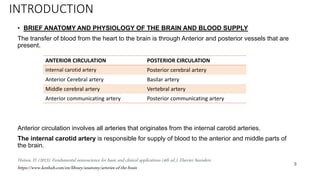
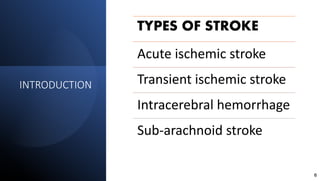
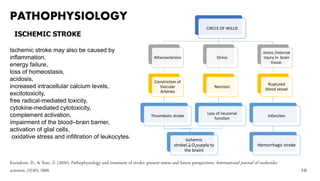
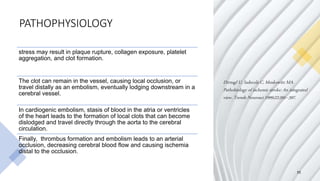
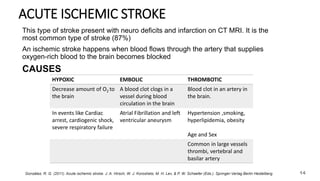
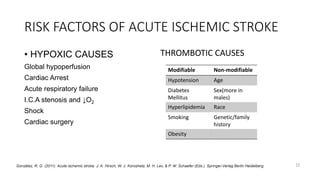
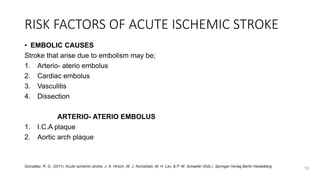
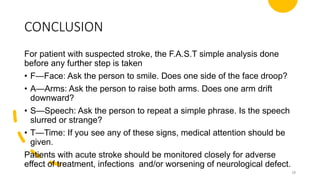
The document provides a comprehensive overview of stroke, including its definition, types, risk factors, epidemiology, pathophysiology, clinical manifestations, and treatment options. Stroke is characterized by the rapid loss of brain function due to disrupted blood supply, with significant mortality and disability worldwide. It outlines both non-modifiable and modifiable risk factors, recent research on causes, and detailed treatment guidelines for various stroke types.