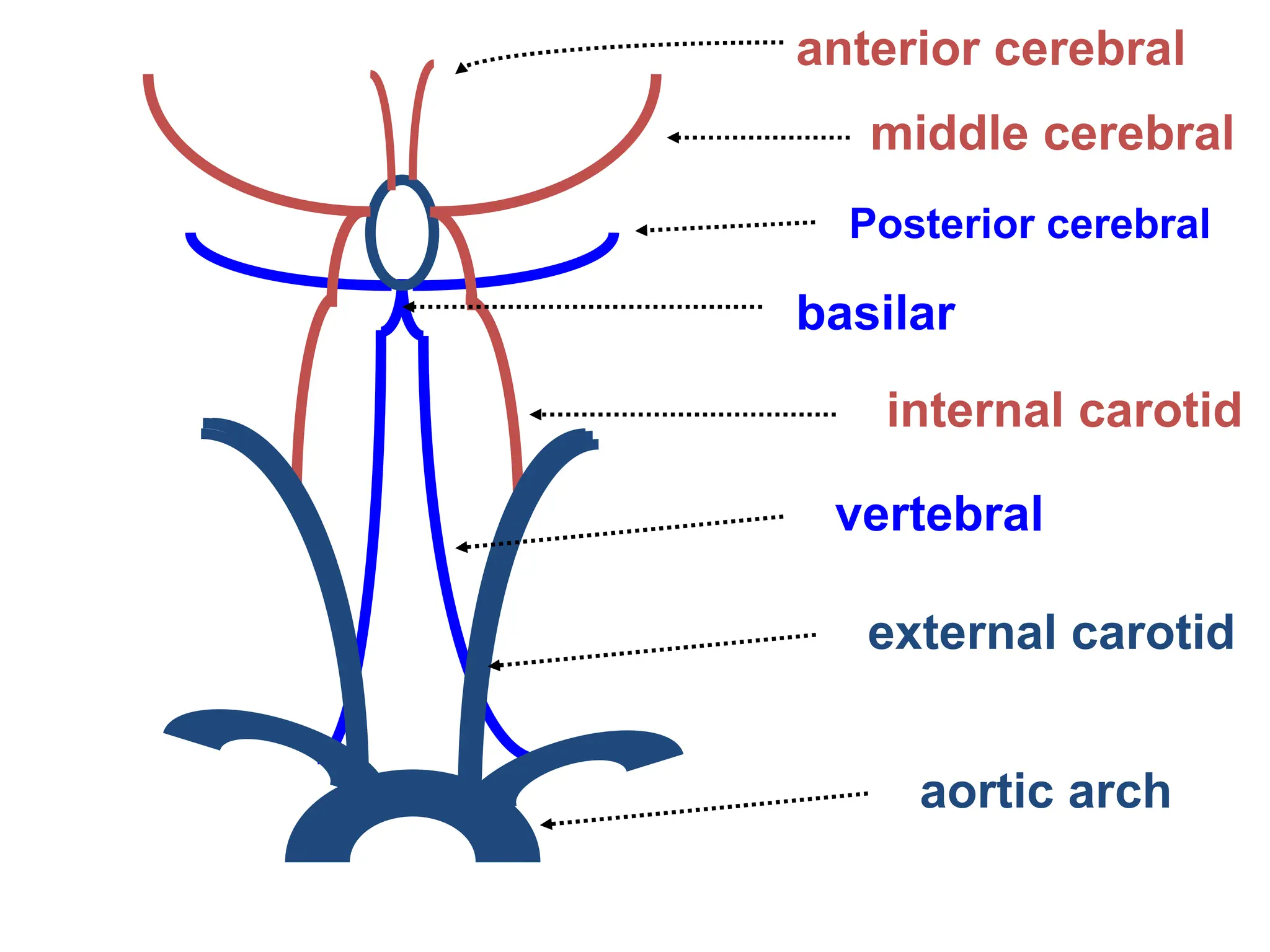
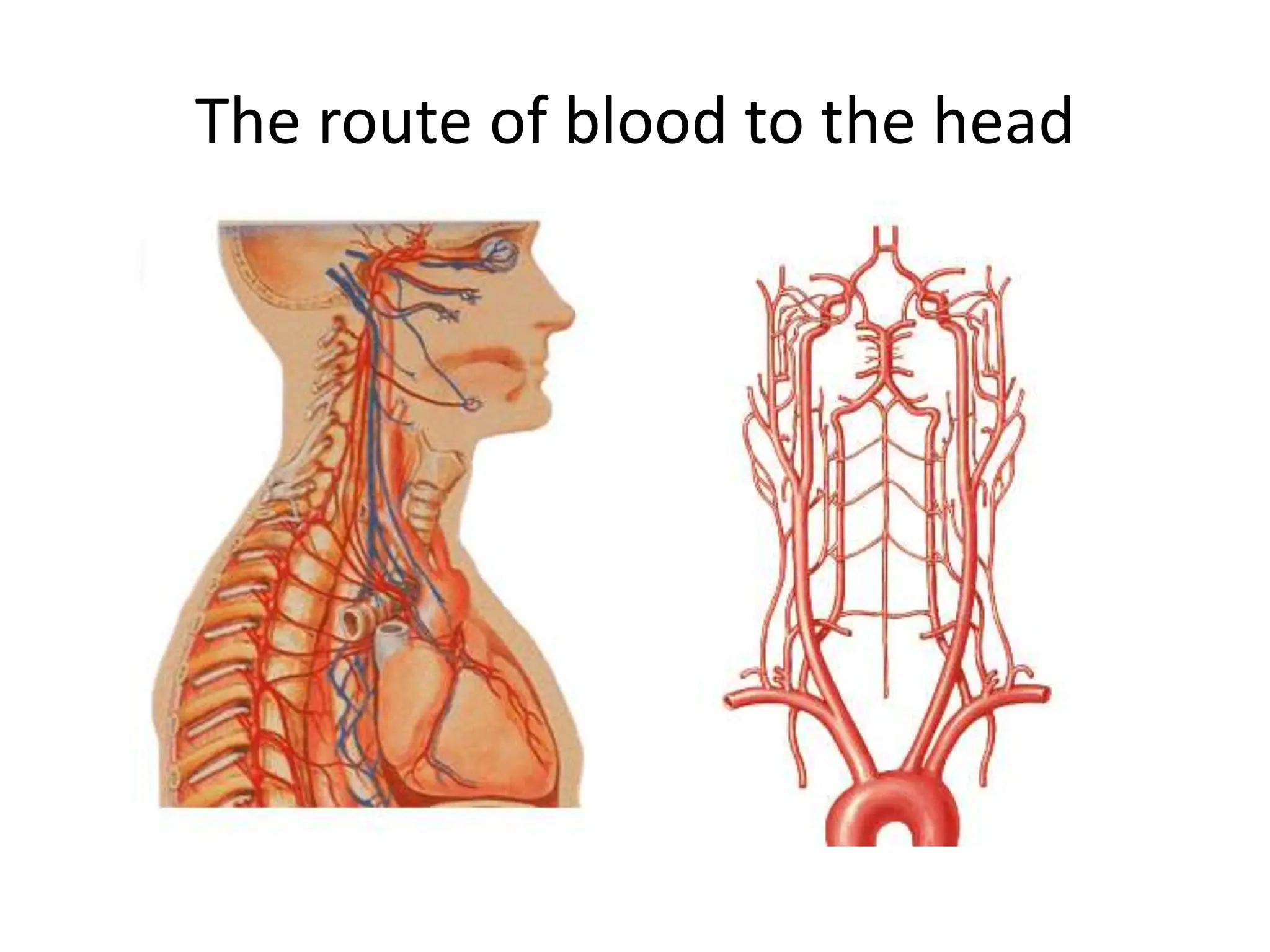
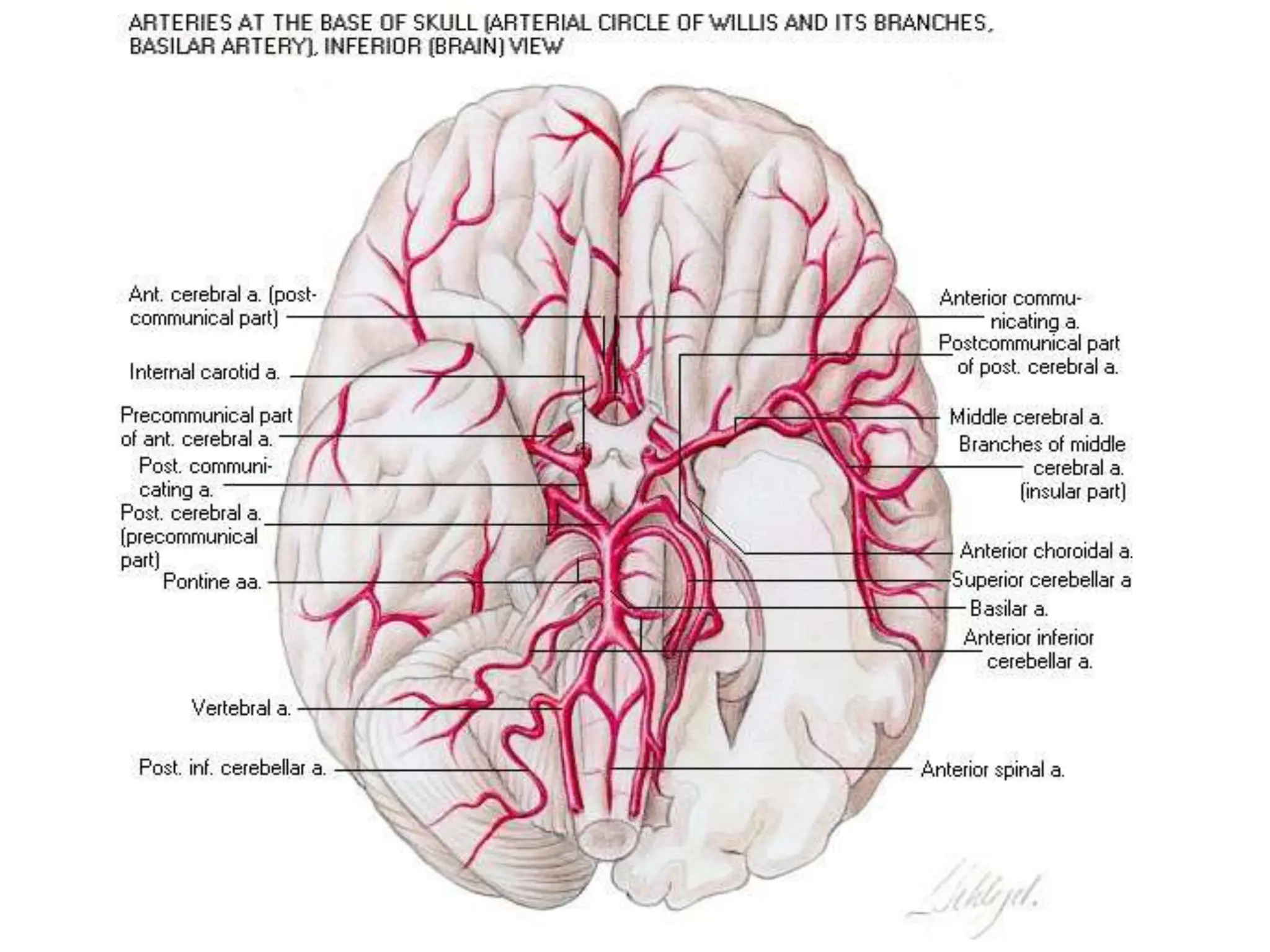
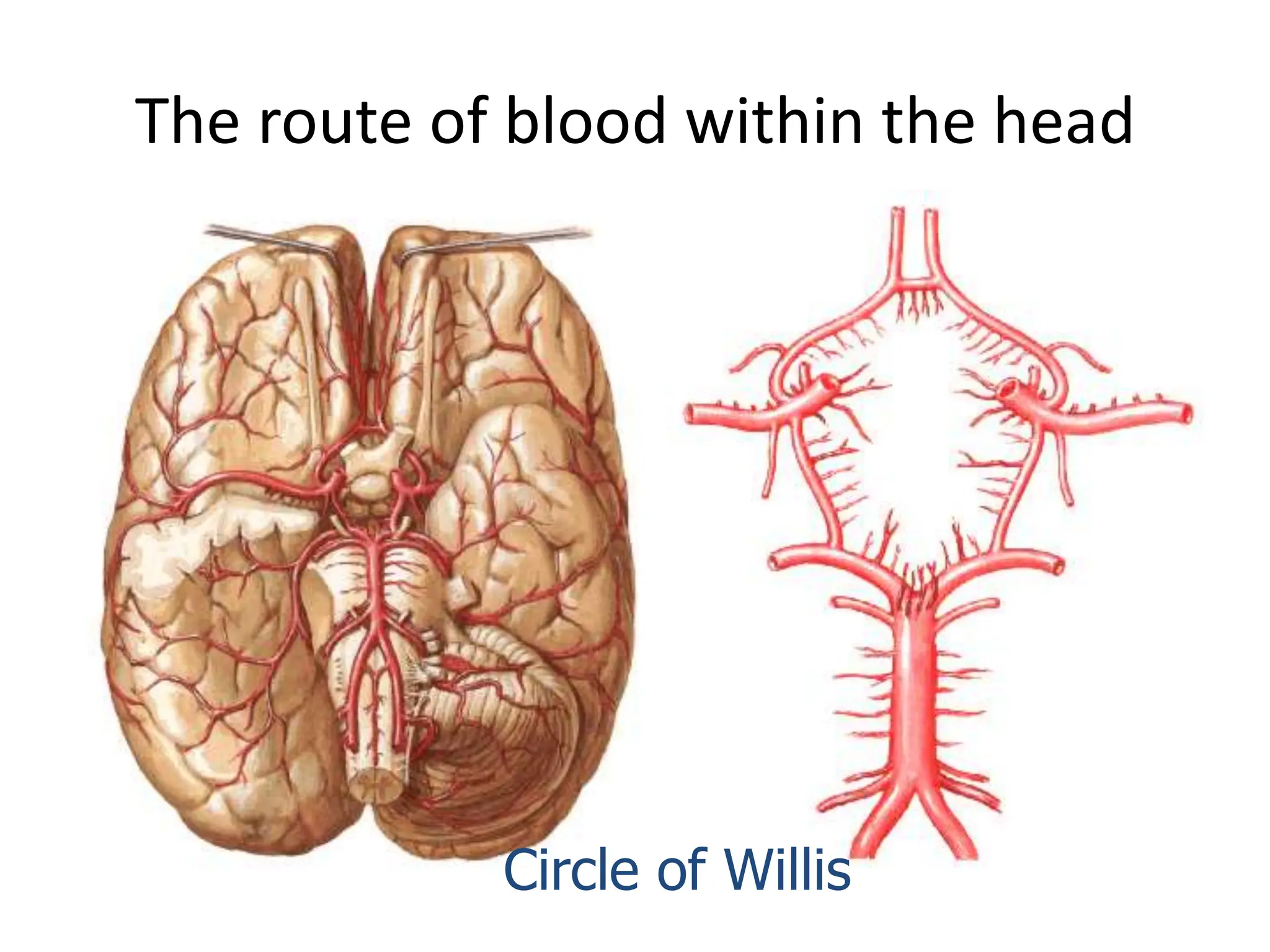
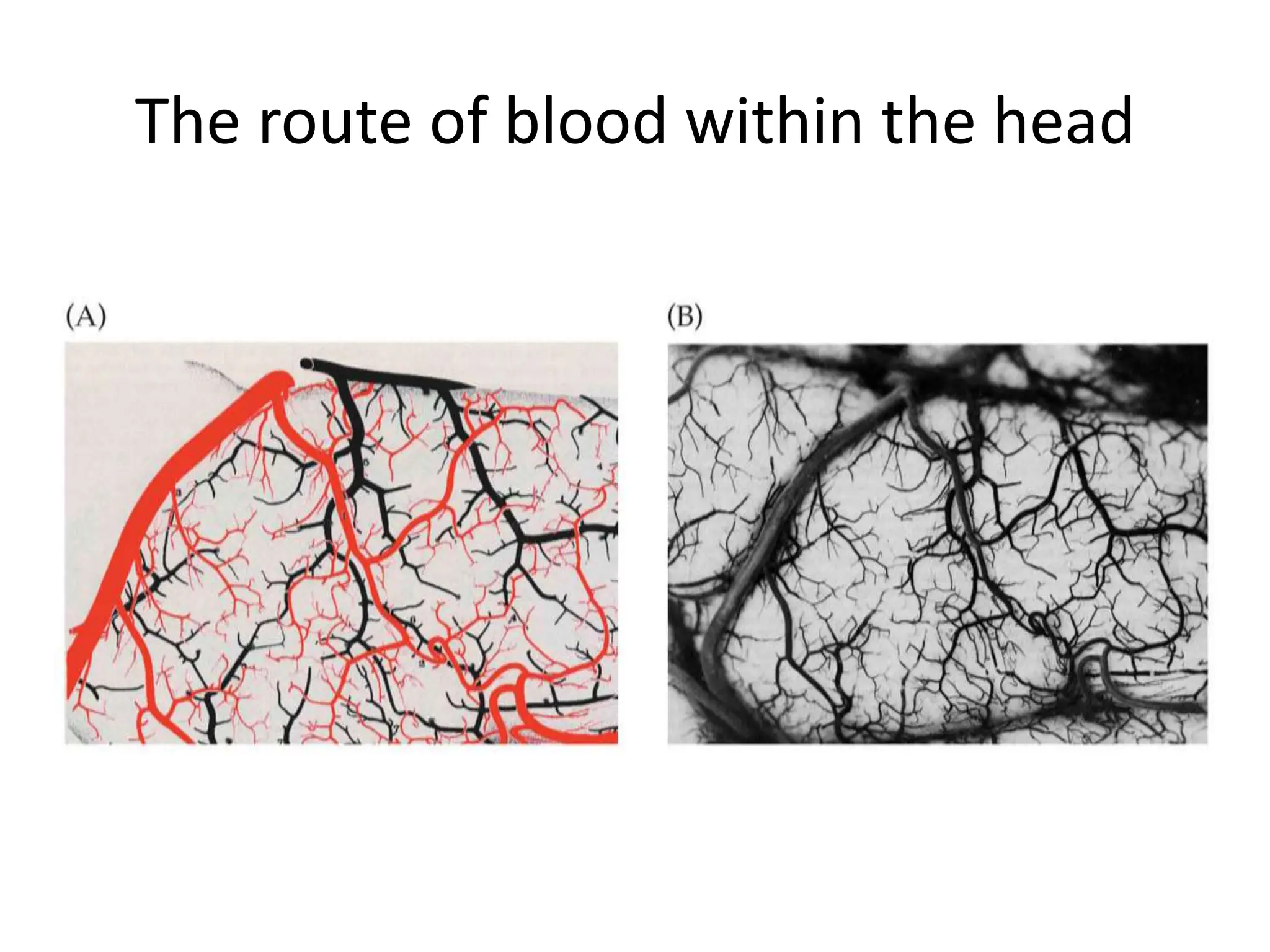
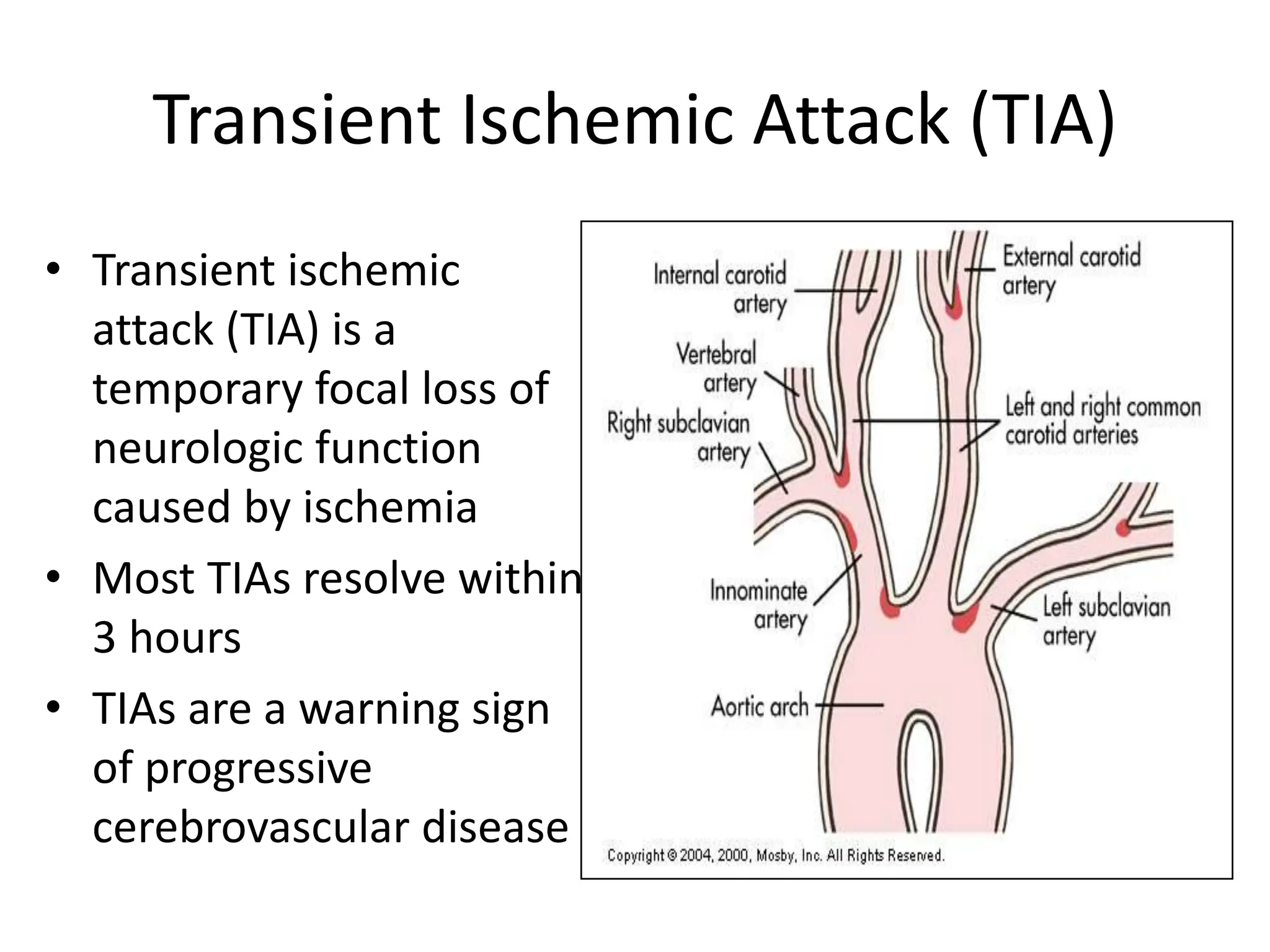
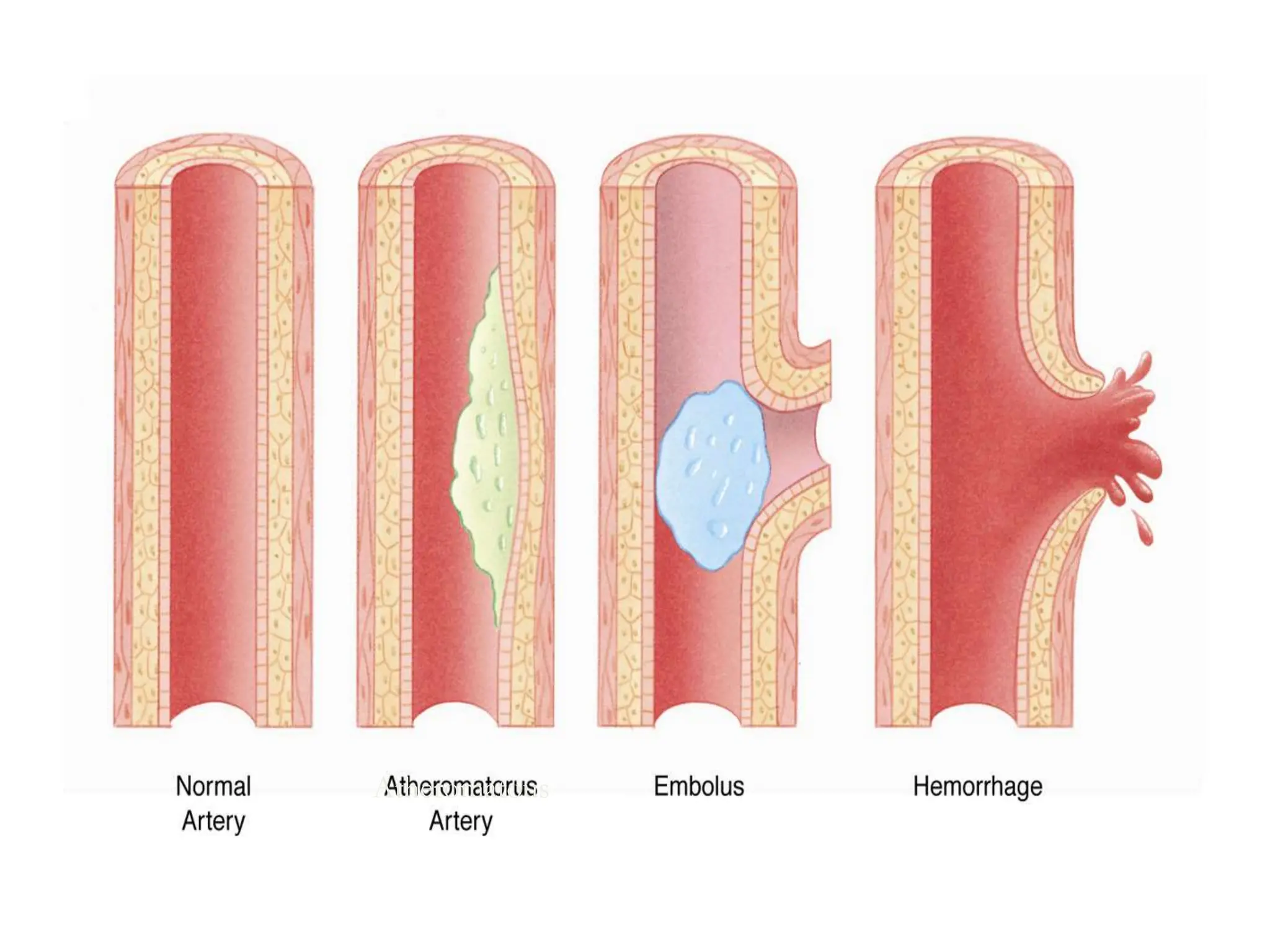
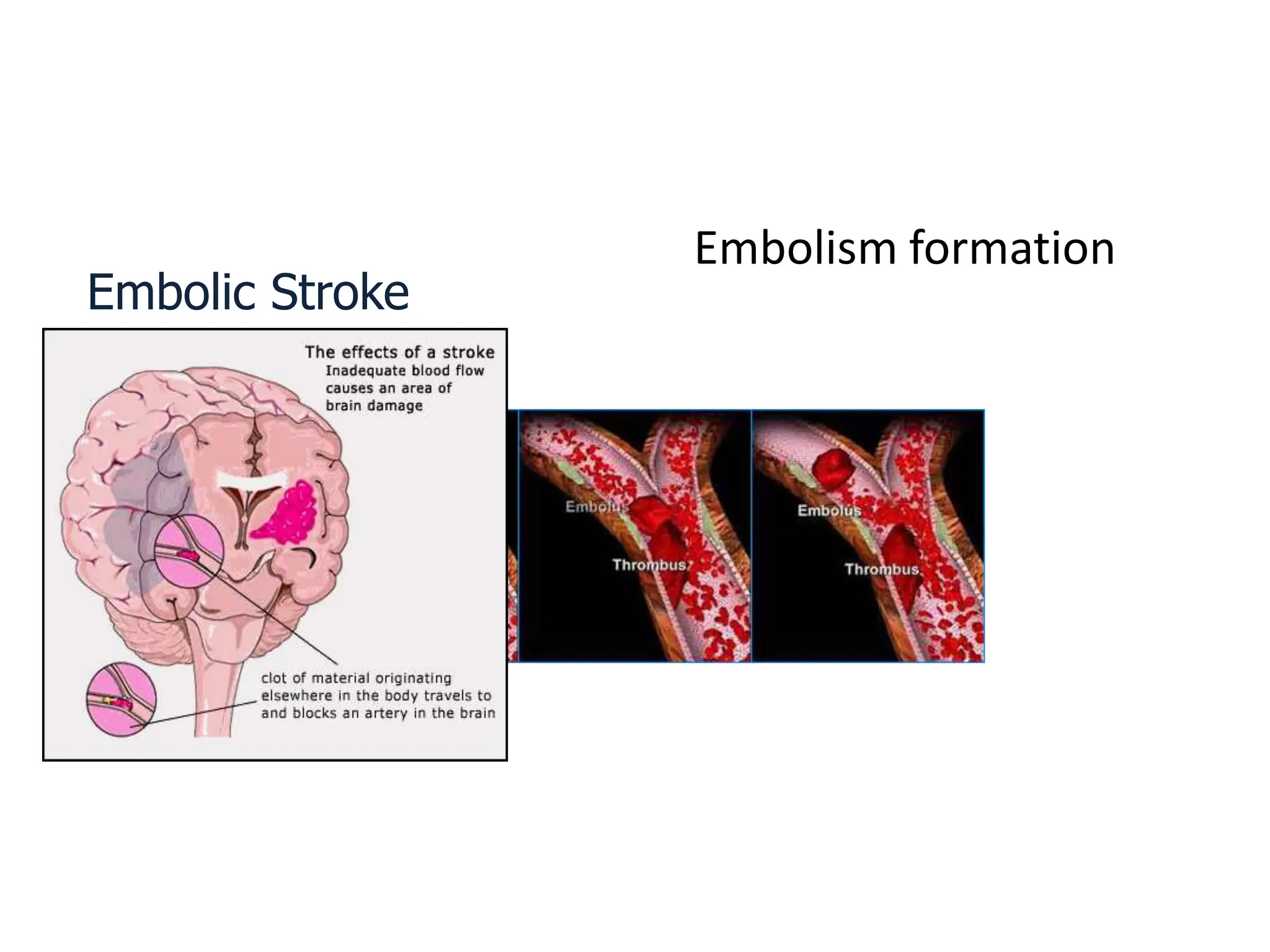
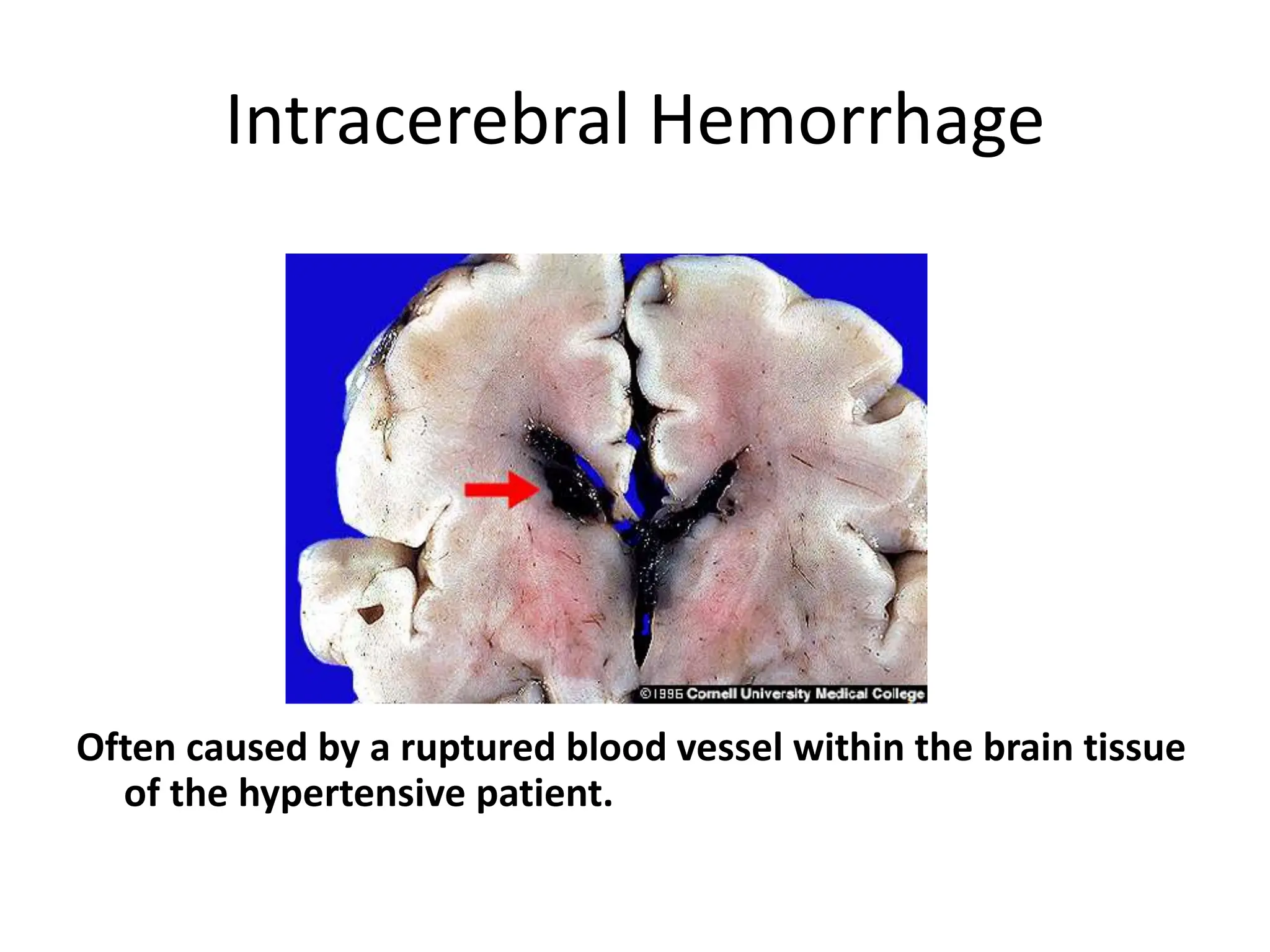
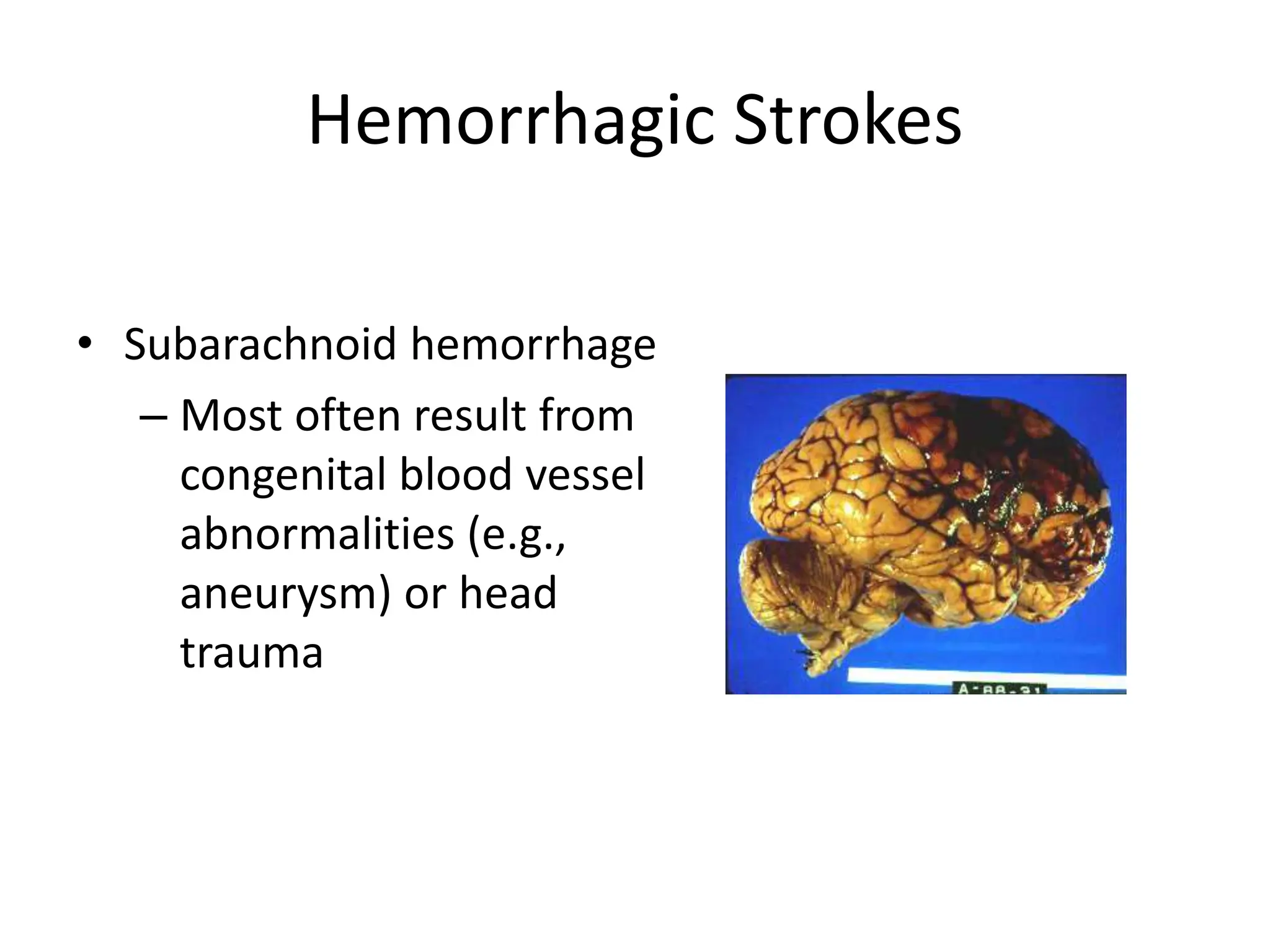
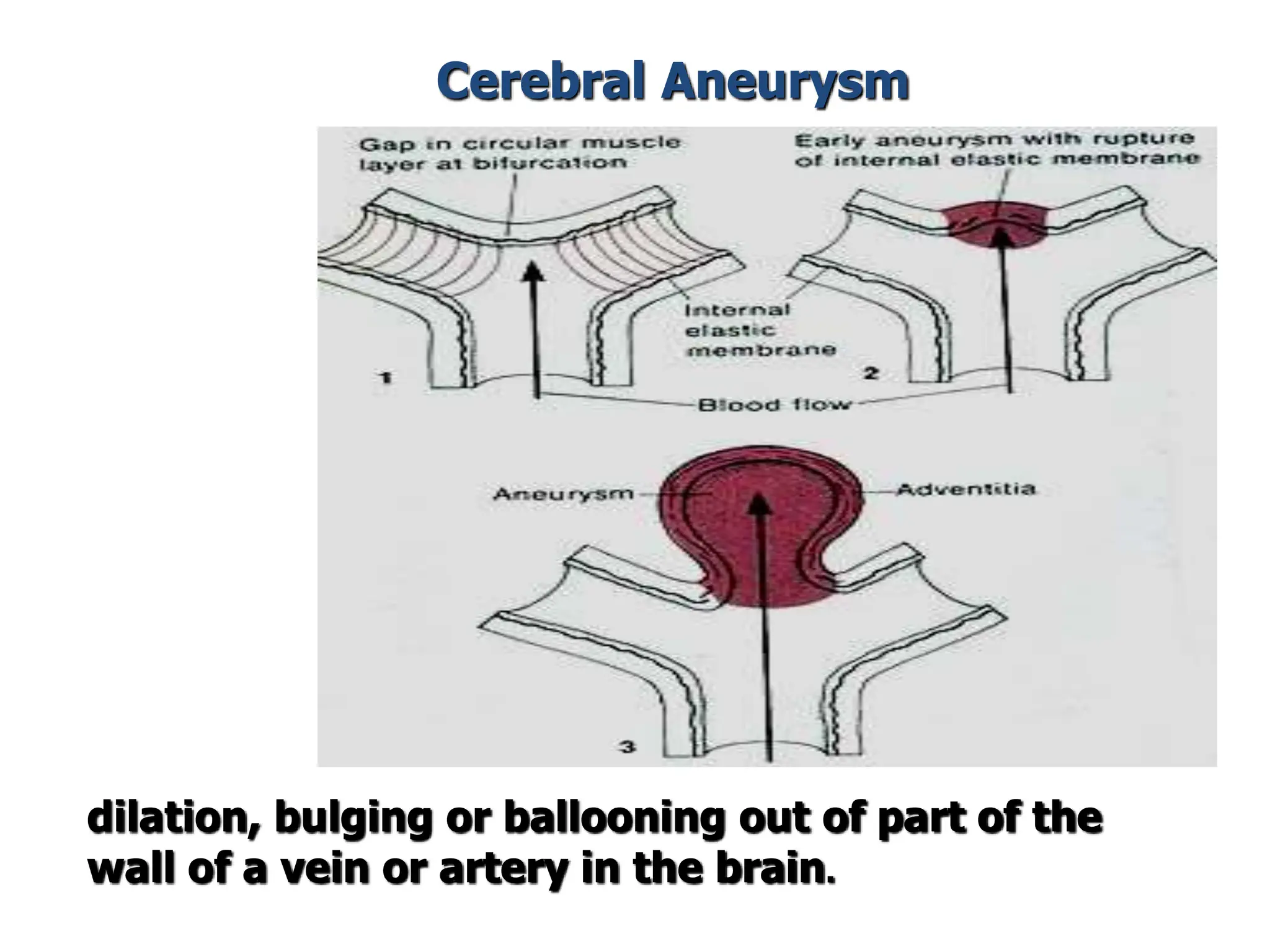
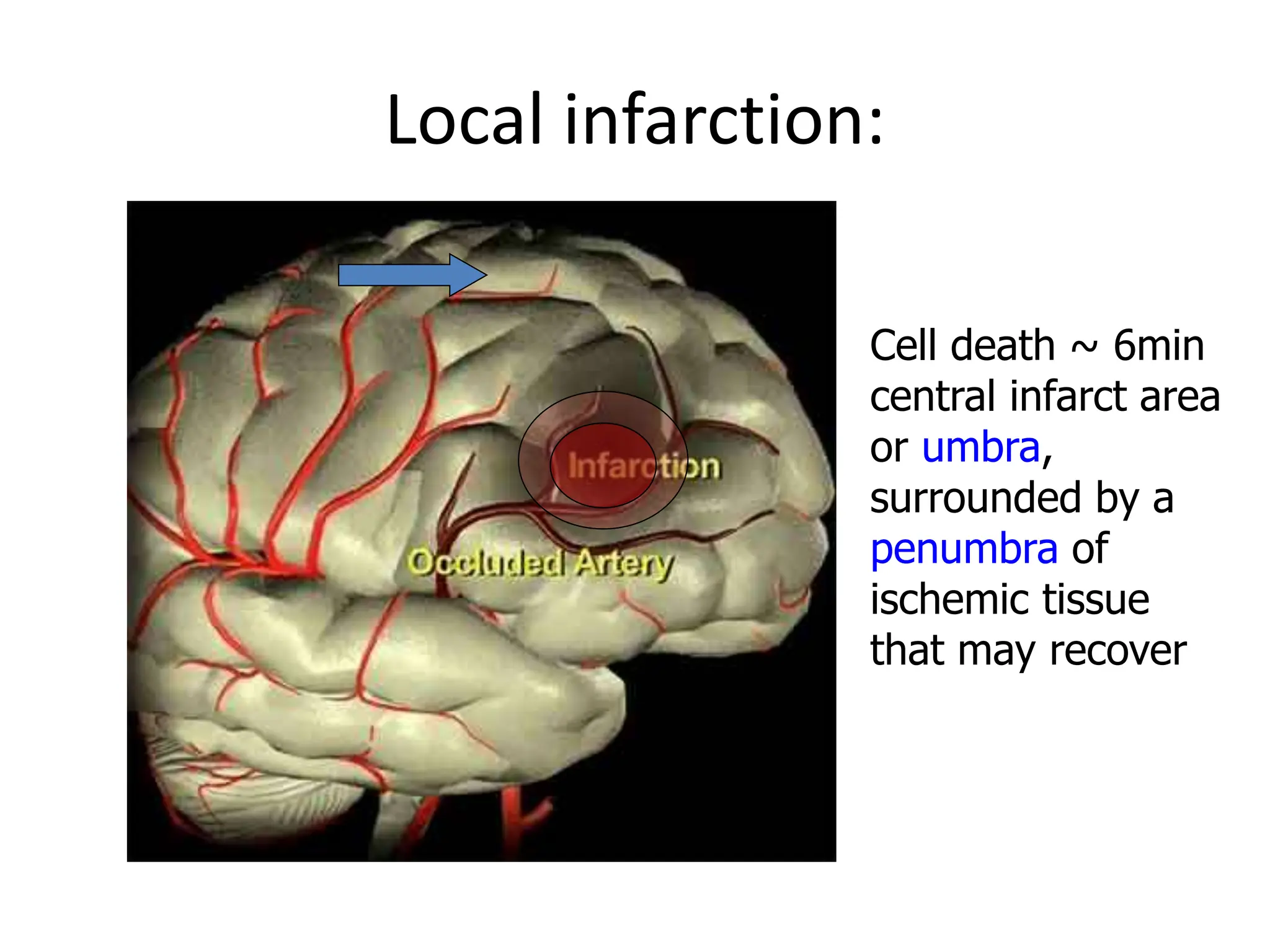
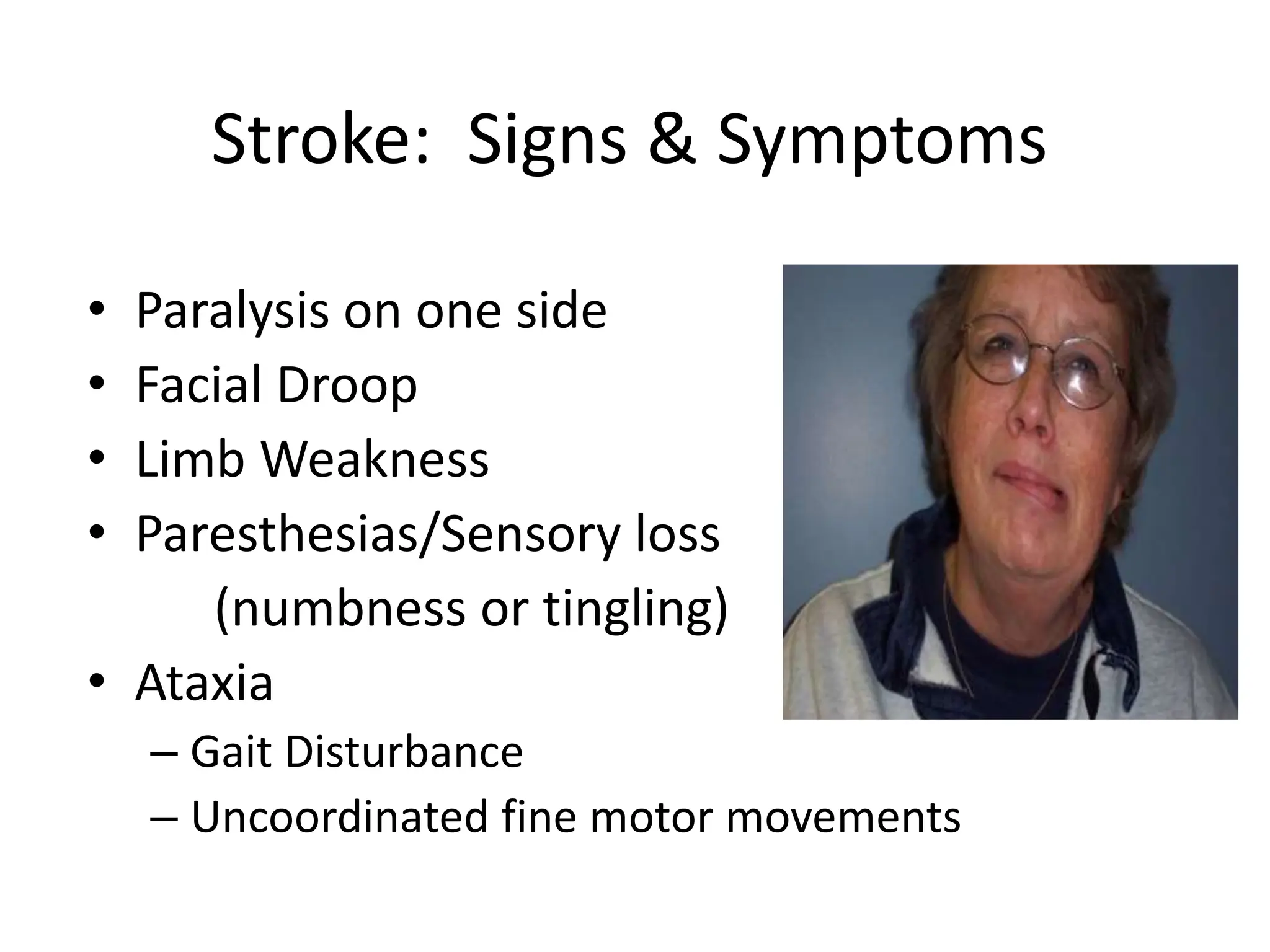
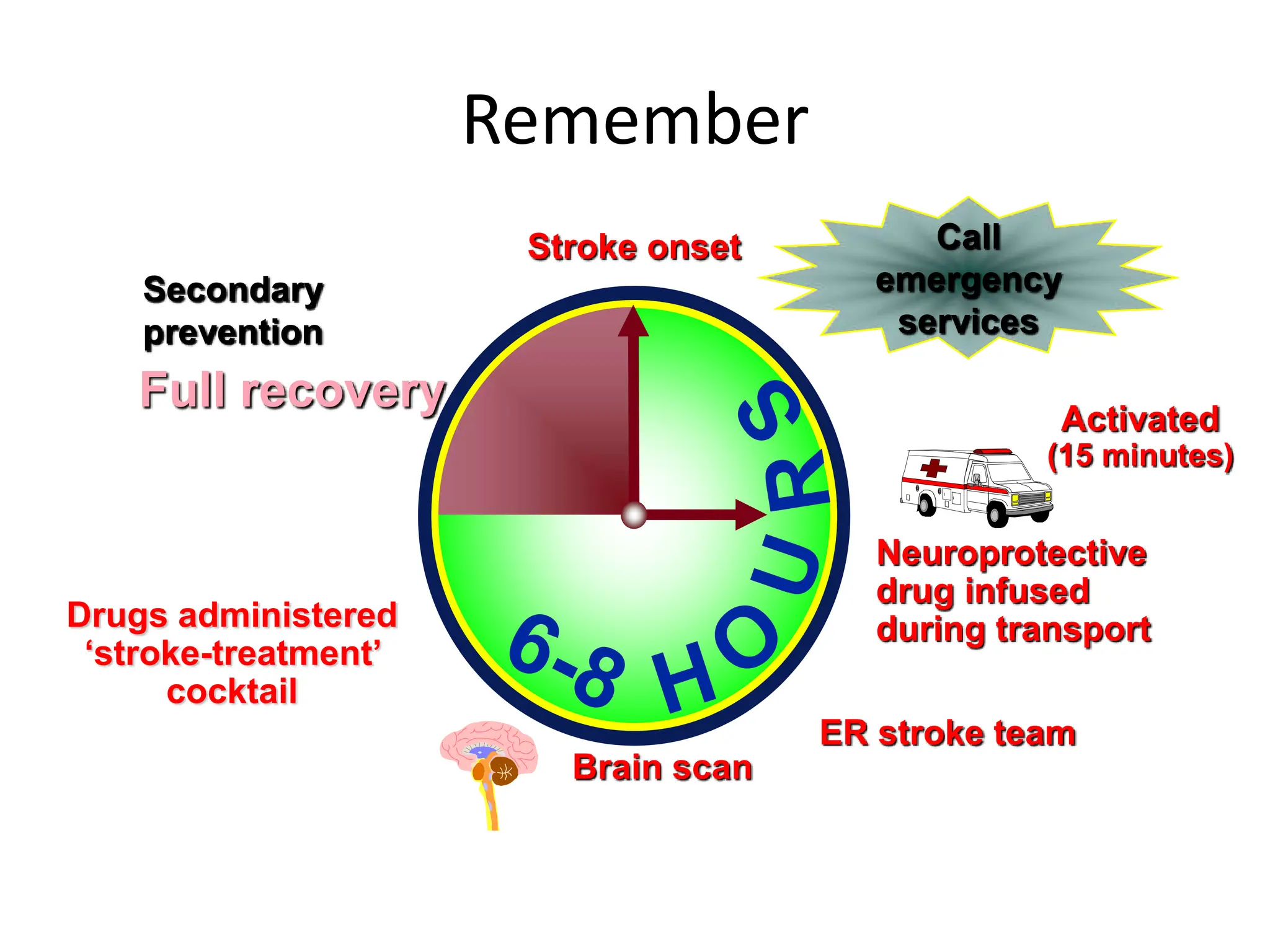
The document discusses strokes, defined as the injury or death of brain tissue due to oxygen deprivation from interrupted blood supply, and outlines types (ischemic and hemorrhagic), risk factors, and symptoms. It highlights the importance of rapid therapy and assessment, emphasizing a multidisciplinary approach to treatment and rehabilitation. Additionally, it presents the underlying pathophysiology, blood supply characteristics, and diagnostic measures to manage and prevent strokes effectively.