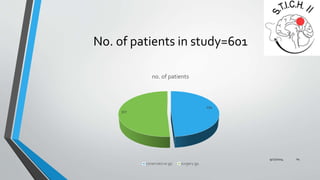
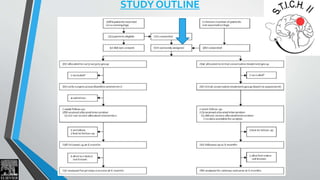
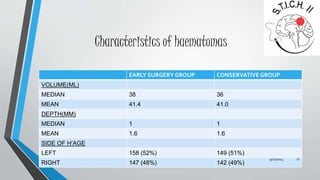
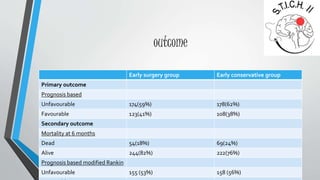
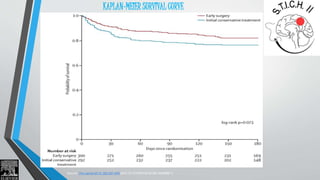
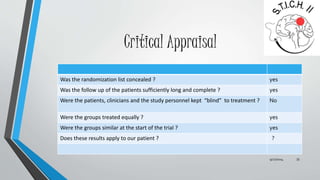
This document summarizes the STICH II trial which compared early surgery versus initial conservative treatment for spontaneous supratentorial lobar intracerebral haemorrhages between 10-100mL. The trial involved 601 patients randomized to either early surgery within 12 hours or initial conservative treatment with delayed surgery if needed. The primary outcome of death or severe disability at 6 months showed no significant difference between the groups. Secondary outcomes of mortality, functional scales also showed no significant differences, indicating that early surgery did not improve outcomes over initial conservative treatment for these types of hemorrhages.

![INCLUSION CRITERIA
All of the following :
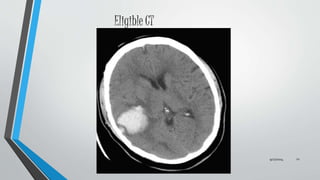
Evidence of a spontaneous lobar ICH on CT scan (1 cm or less from
the cortex surface of the brain)
Patient within 48 hours of ictus.
Best MOTOR score on the Glasgow Coma Scale (GCS) of 5 or 6 and
best EYE score on the GCS of 2 or more
Volume of haematoma between 10 and 100 ml [Calculated using
(a × b × c)/2 method].
9/27/2014 11](https://image.slidesharecdn.com/stichiitrial-140927112006-phpapp01/85/Stich-ii-trial-for-supratentorial-intra-cerebral-bleed-11-320.jpg)