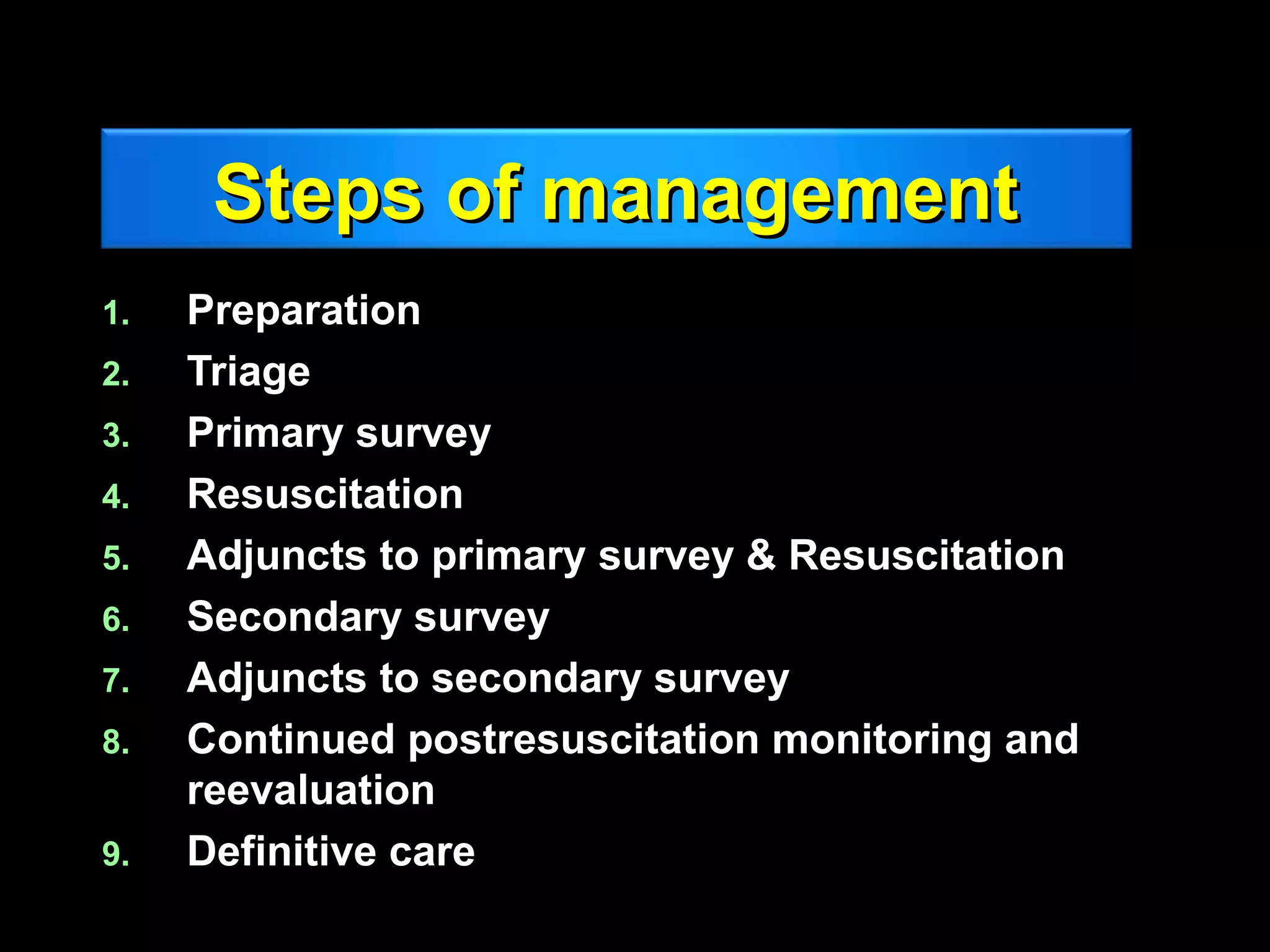
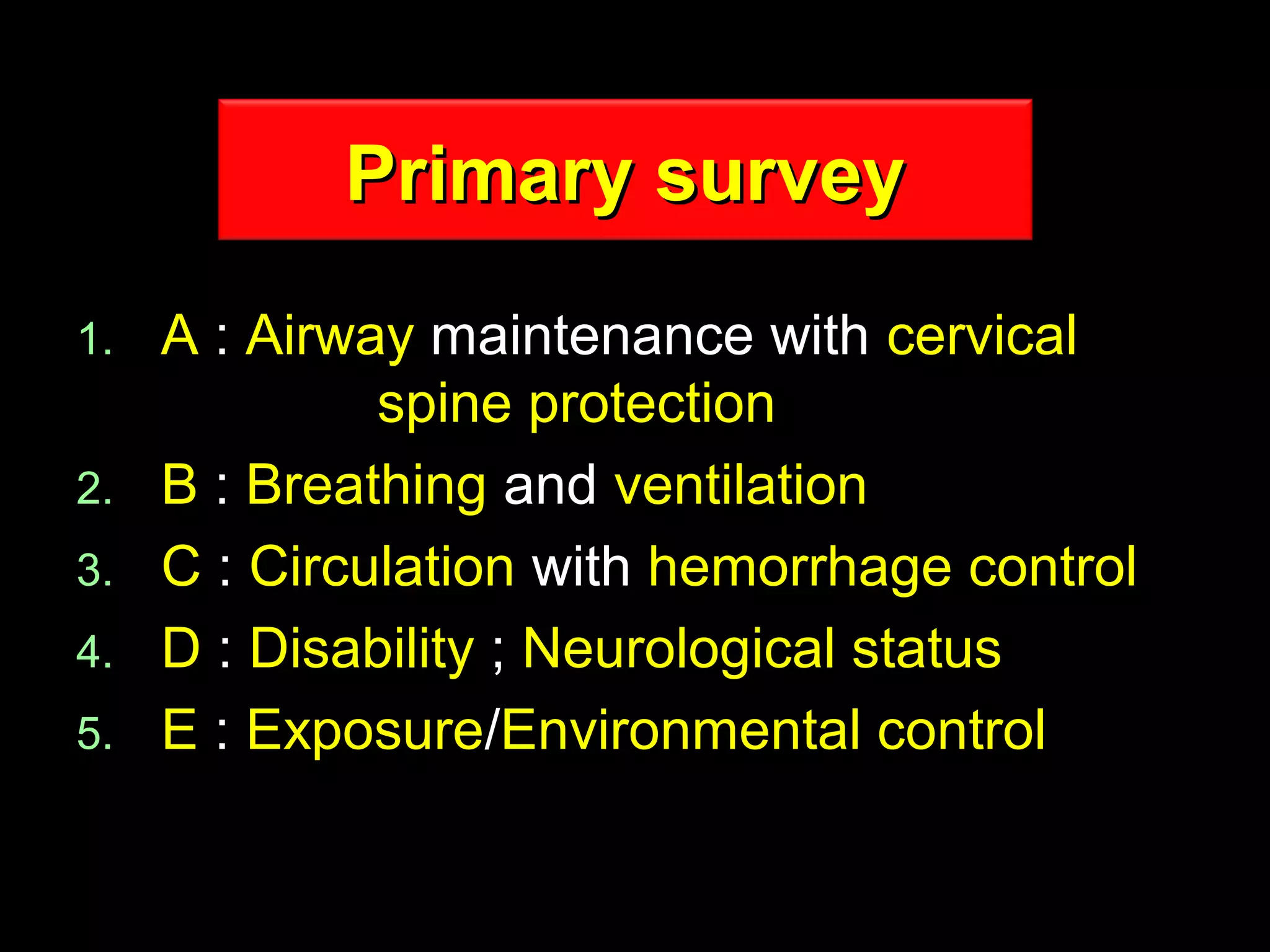
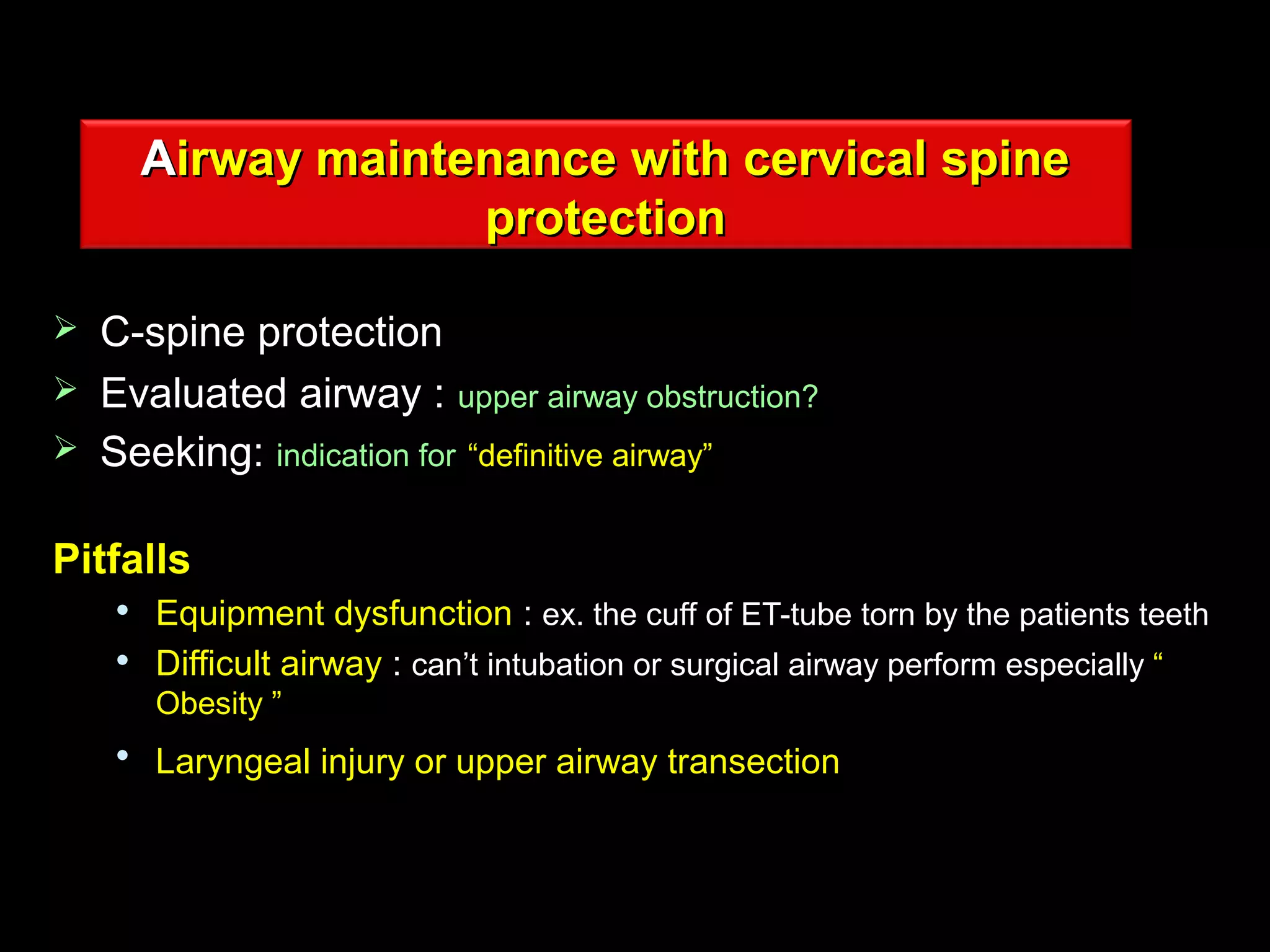
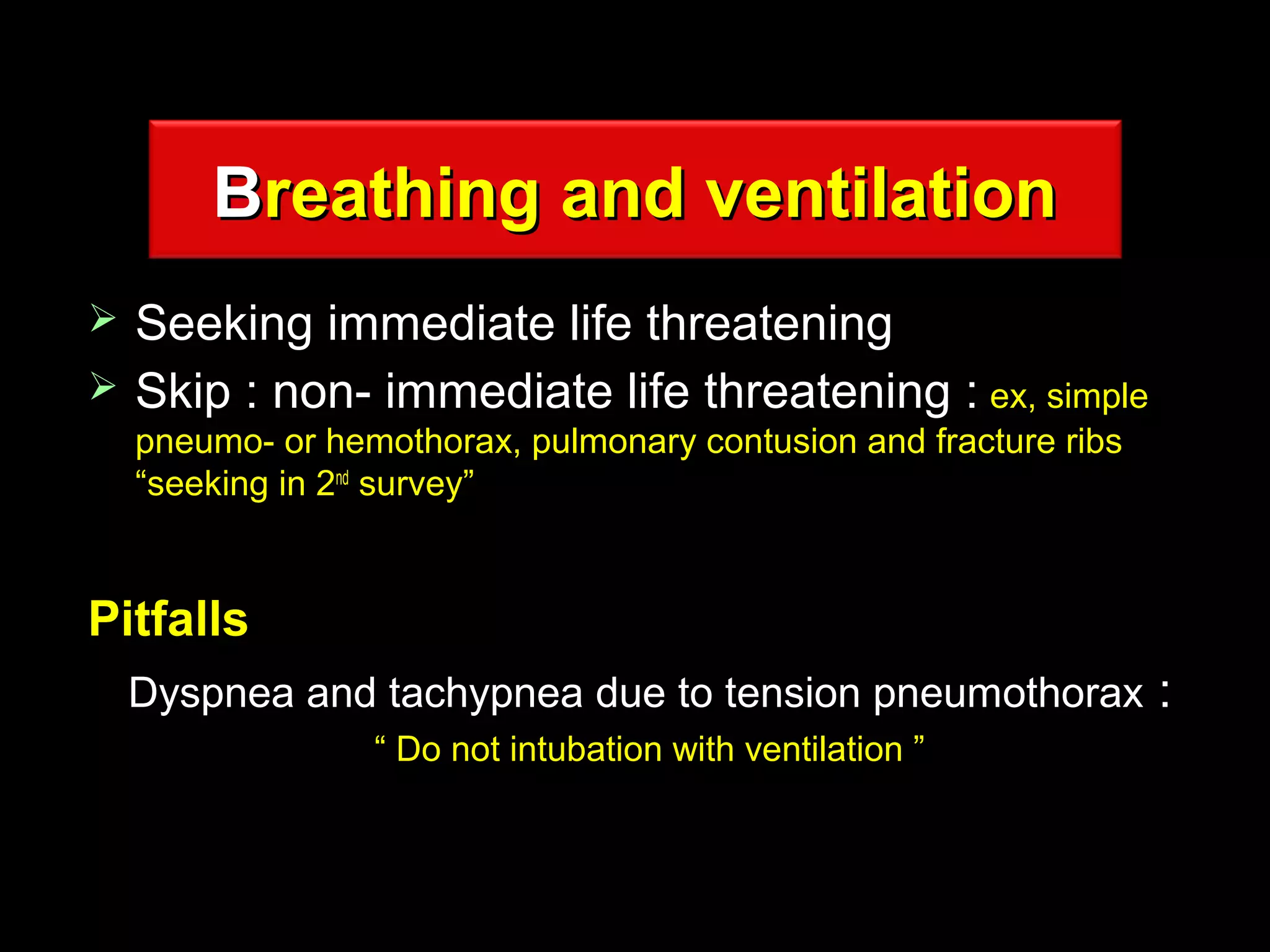
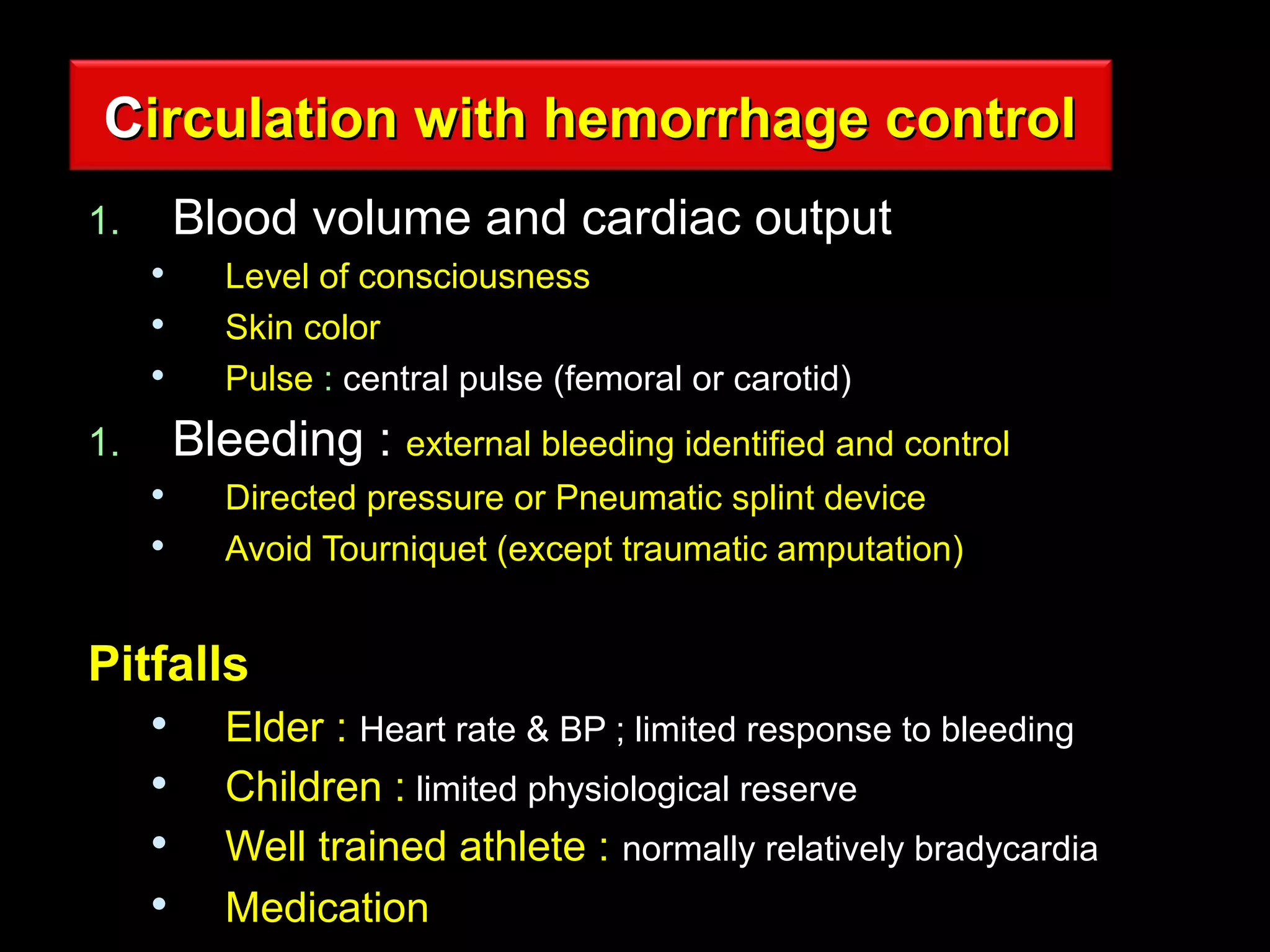
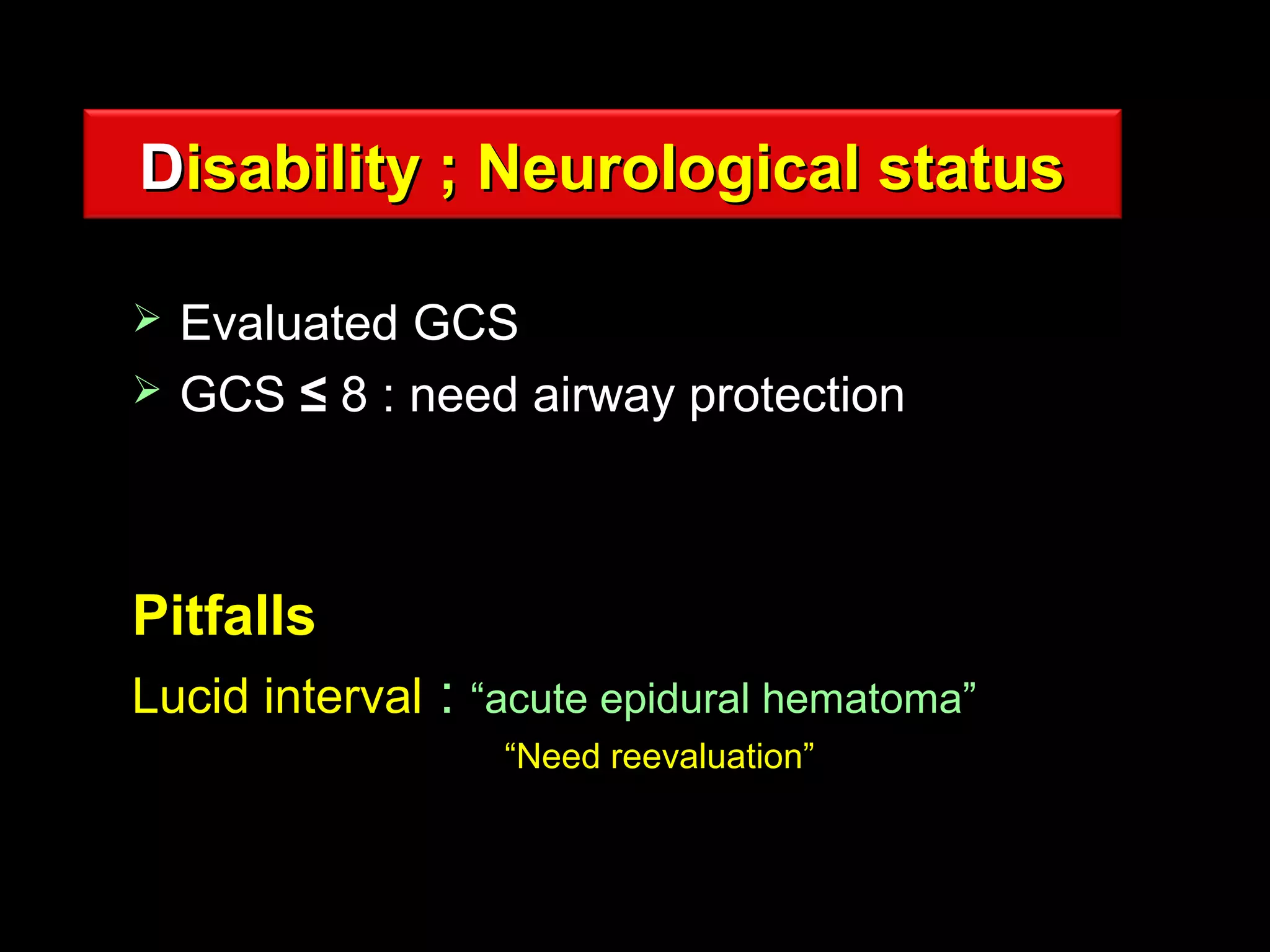
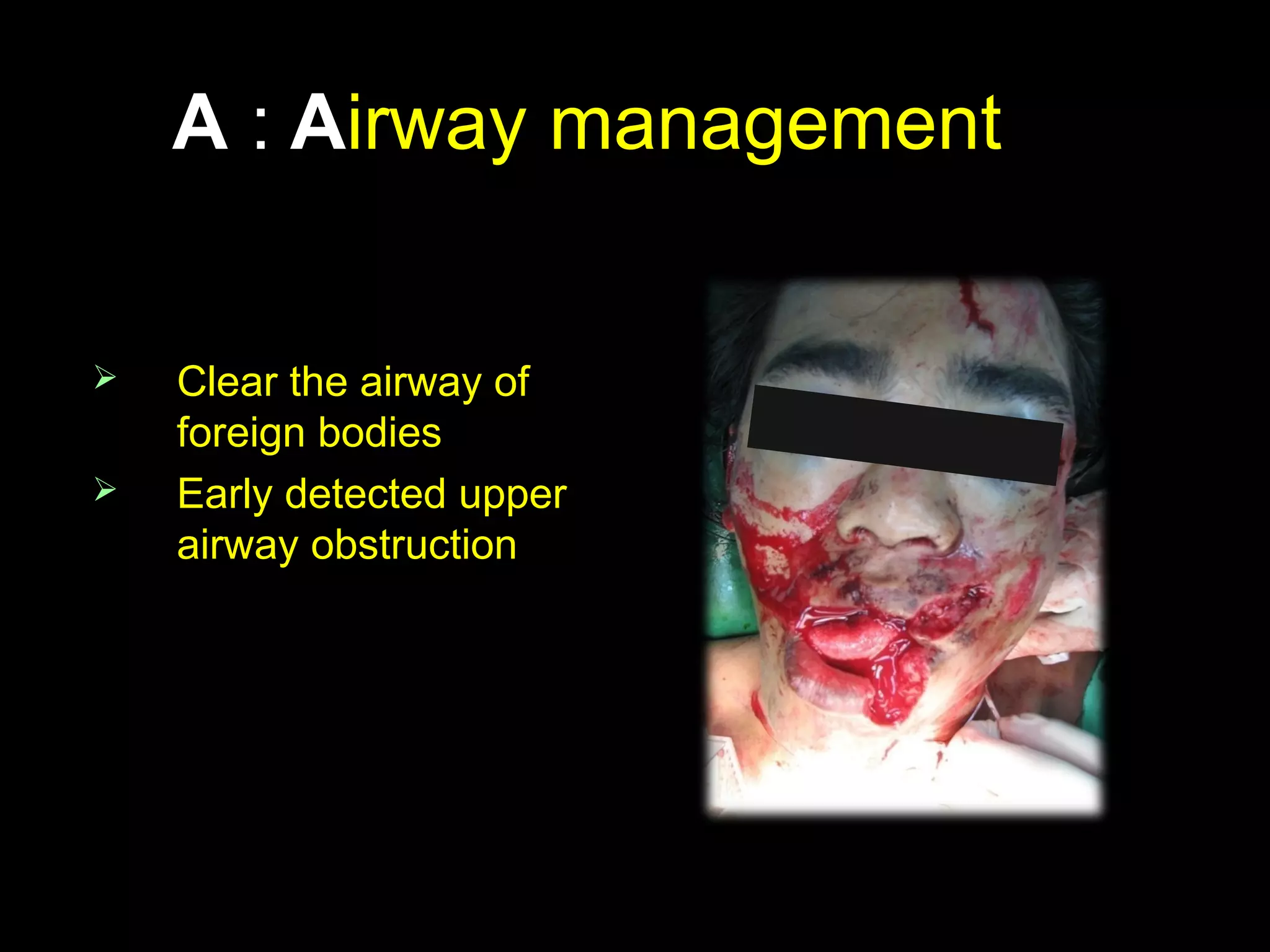
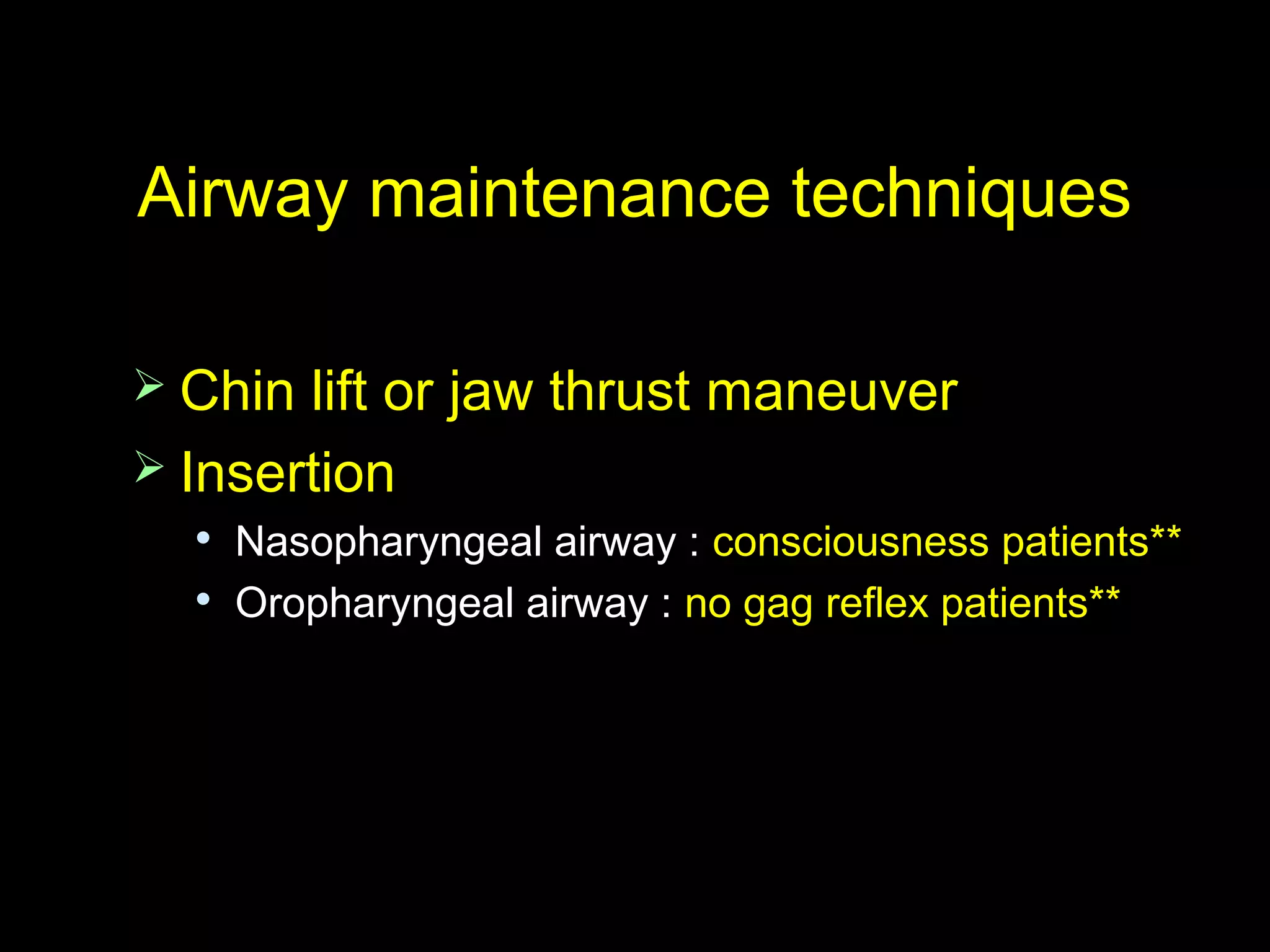
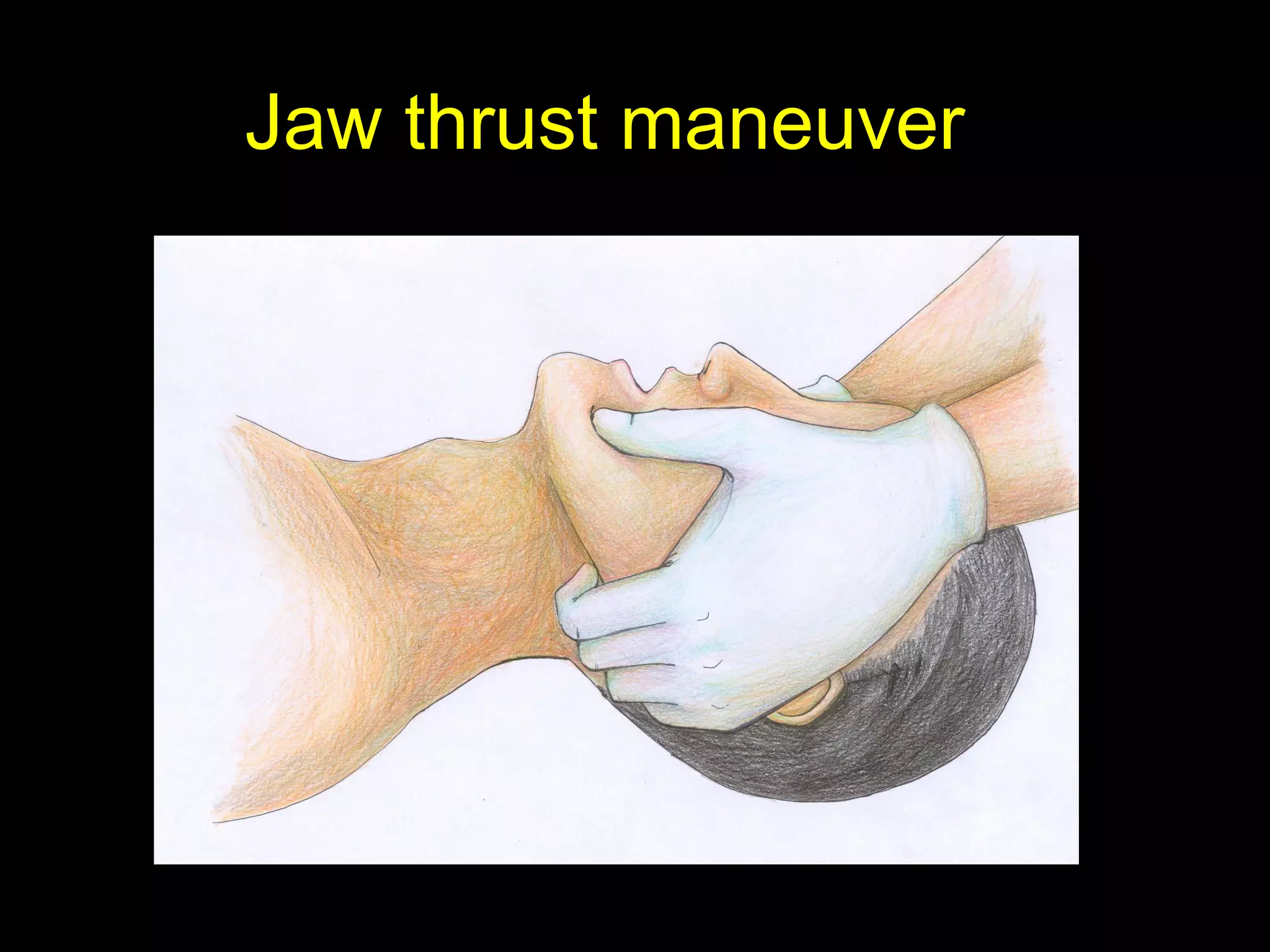
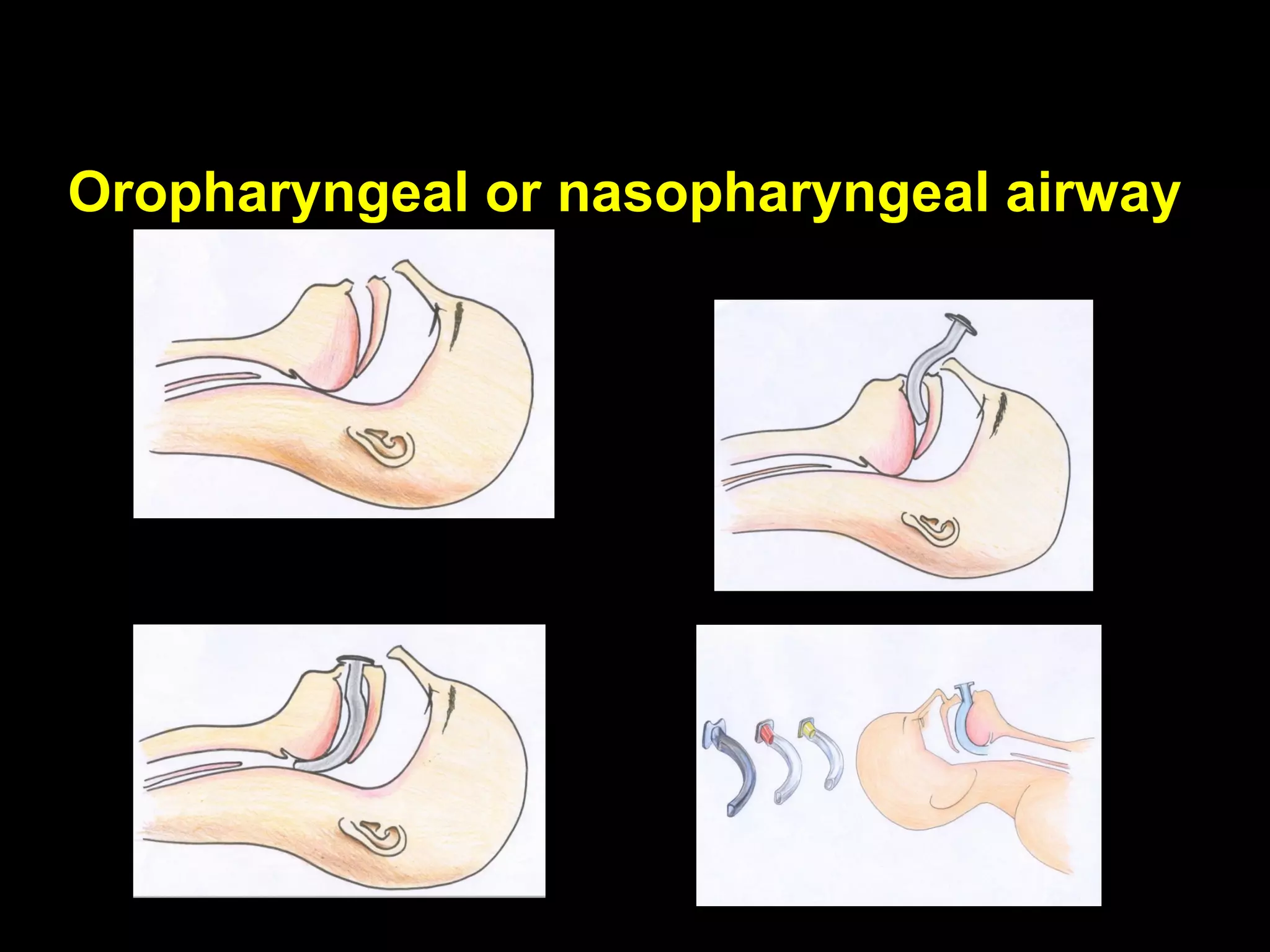
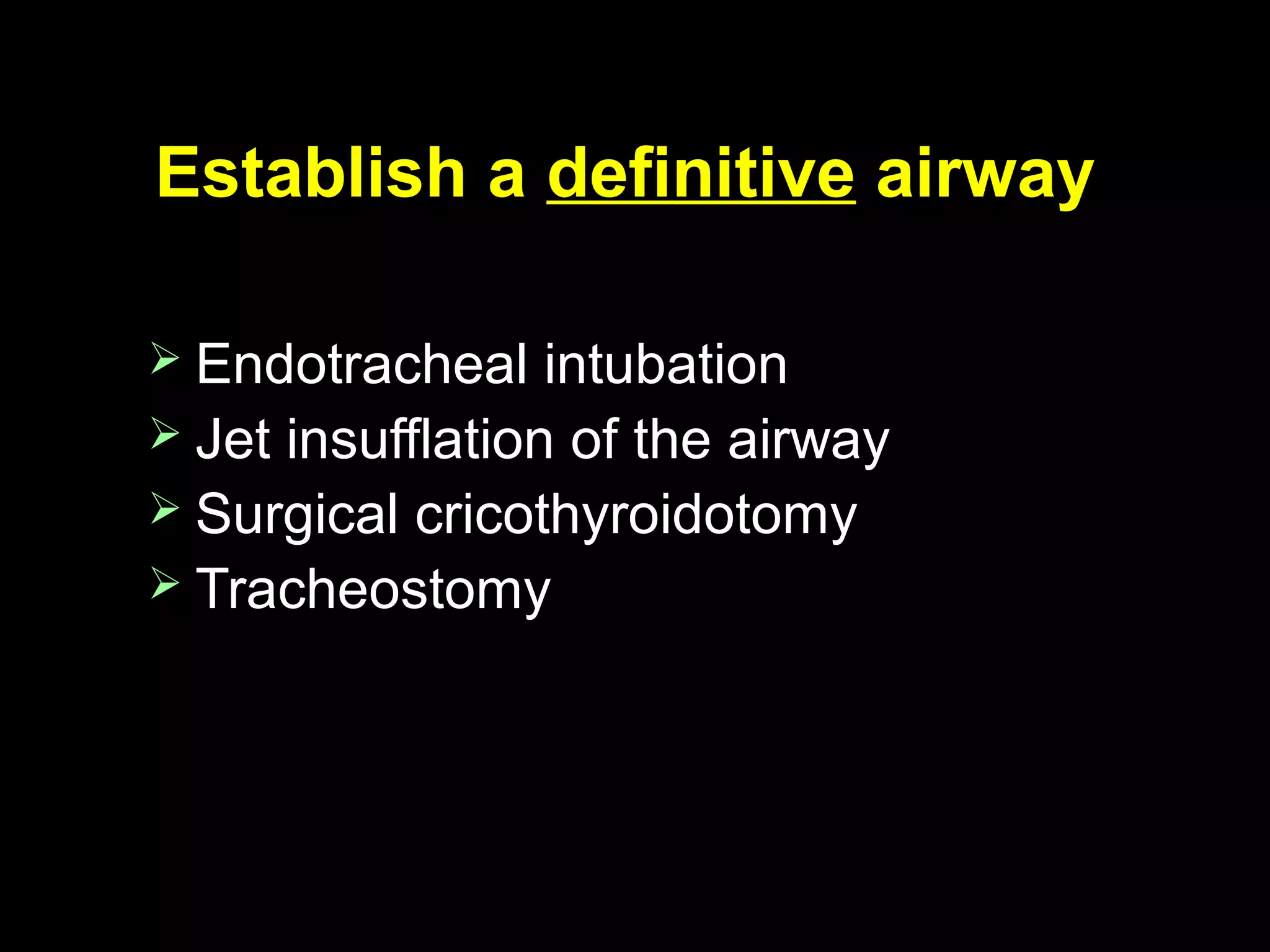
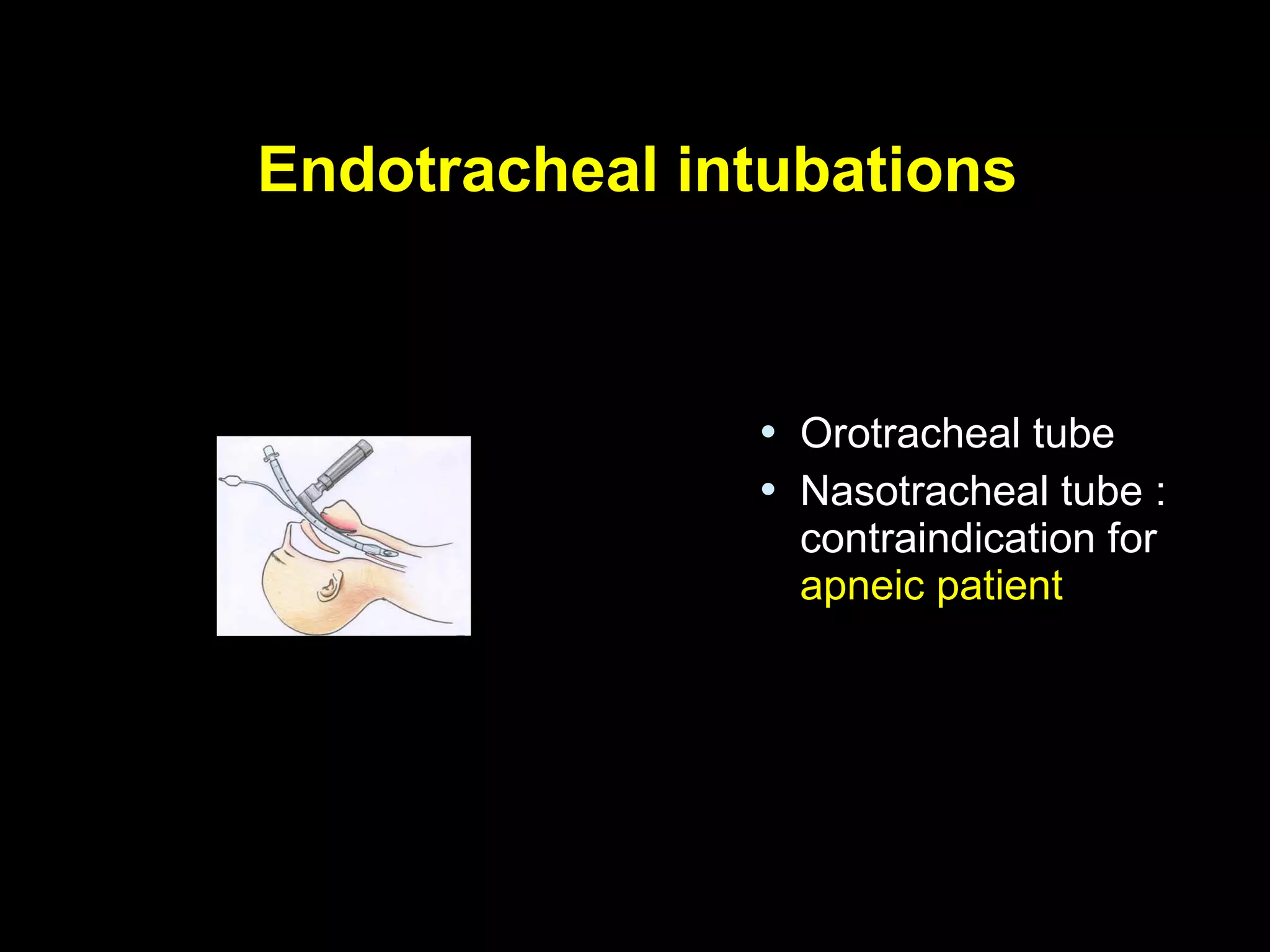
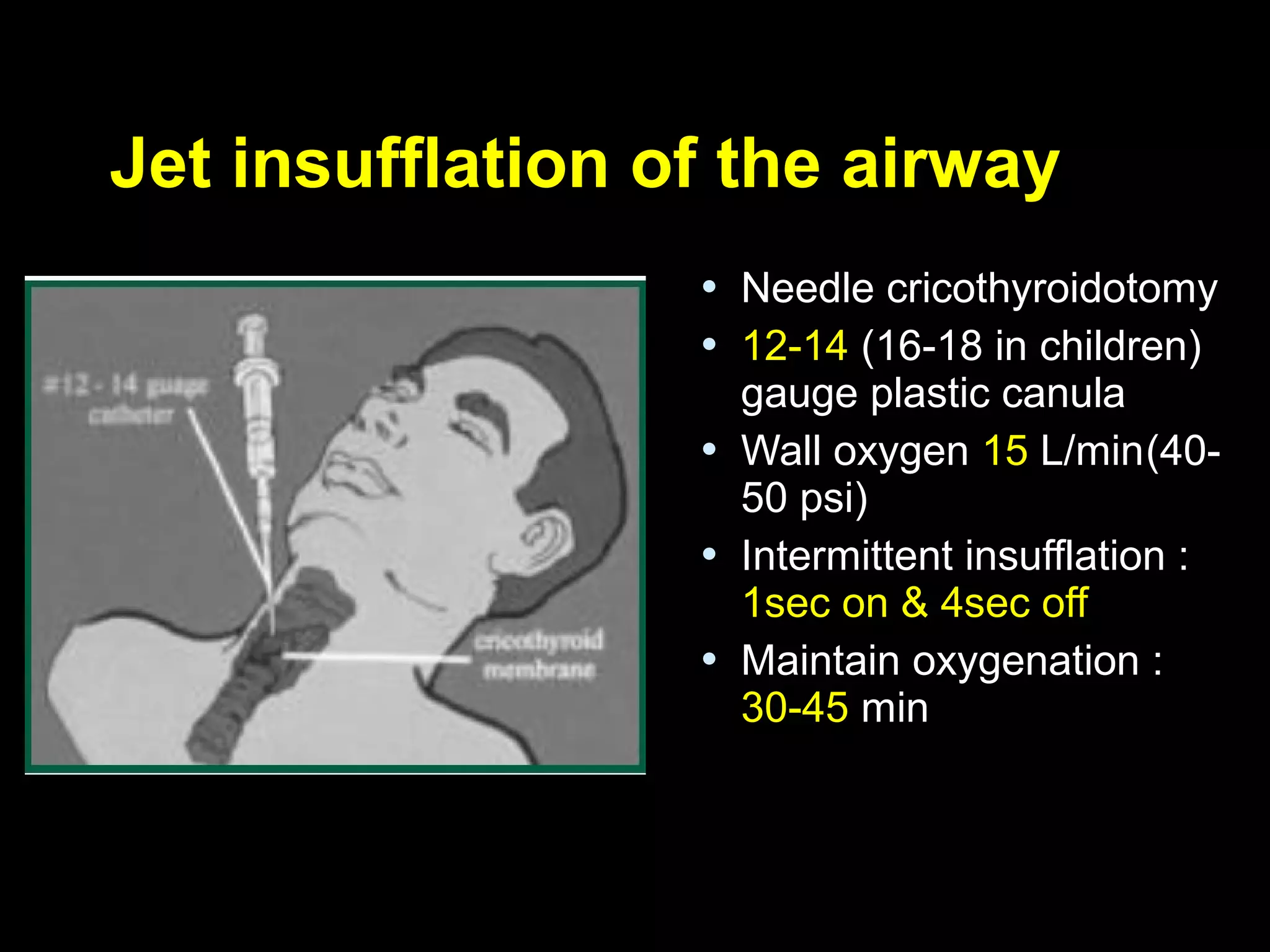
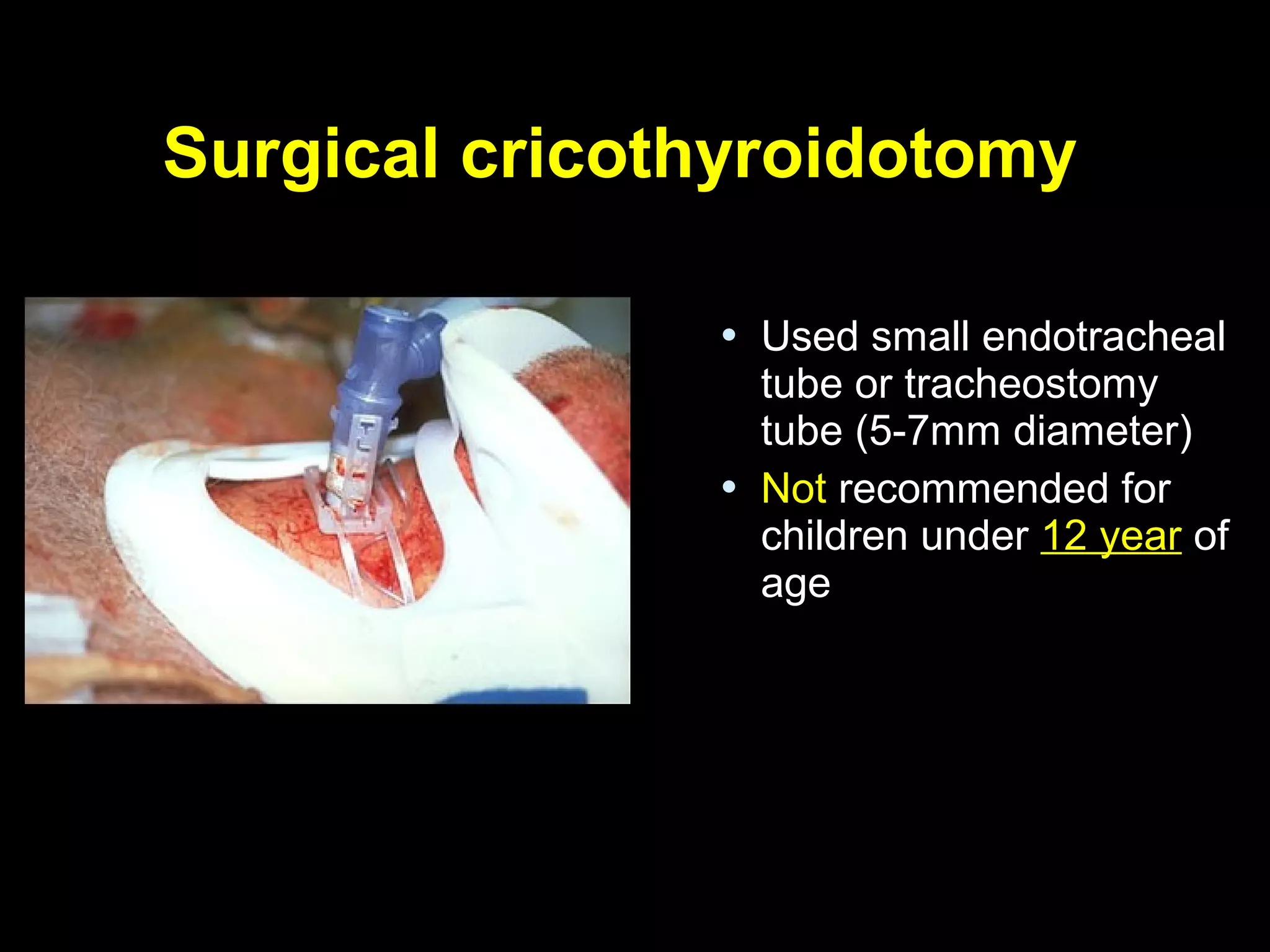
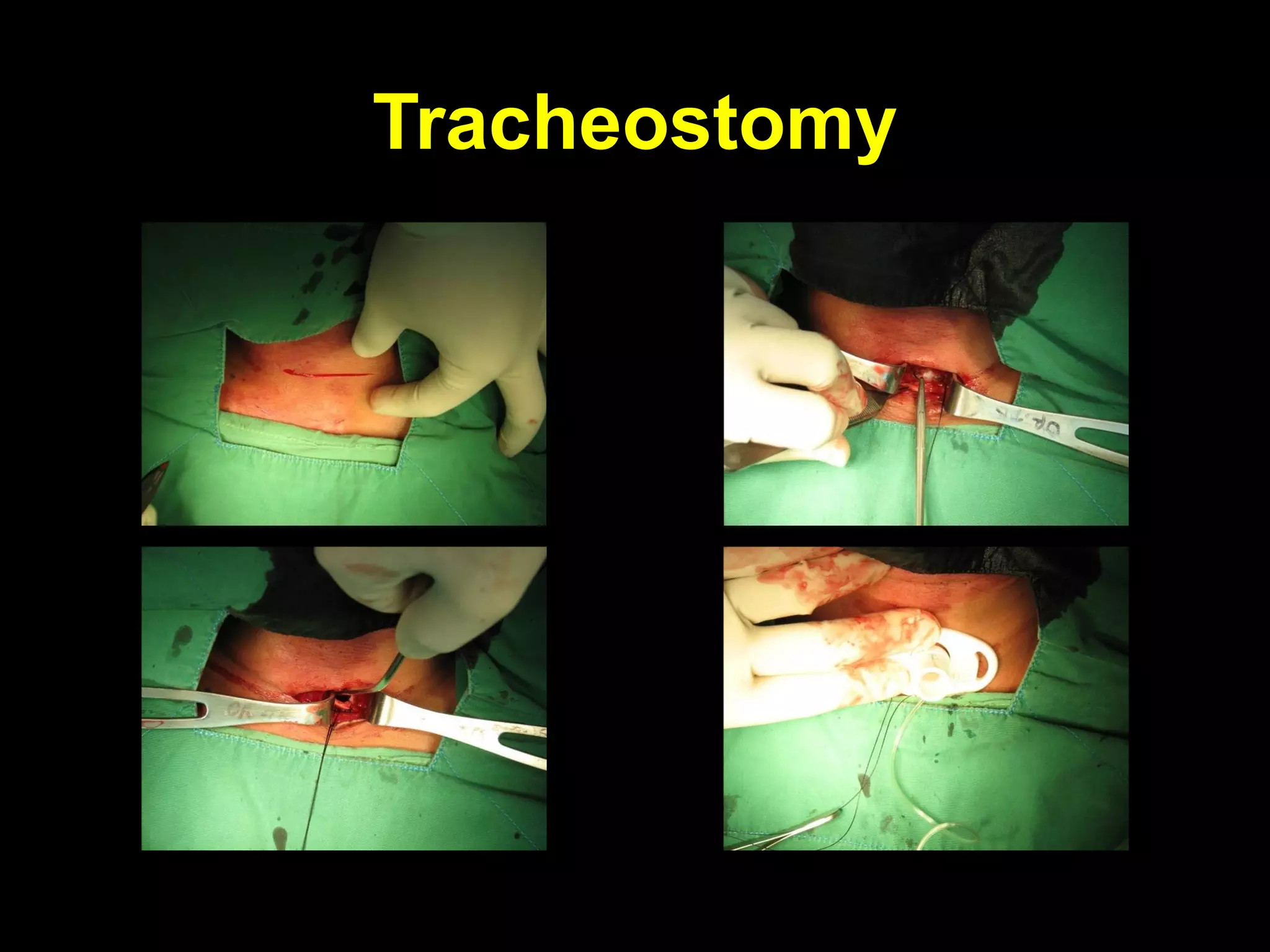
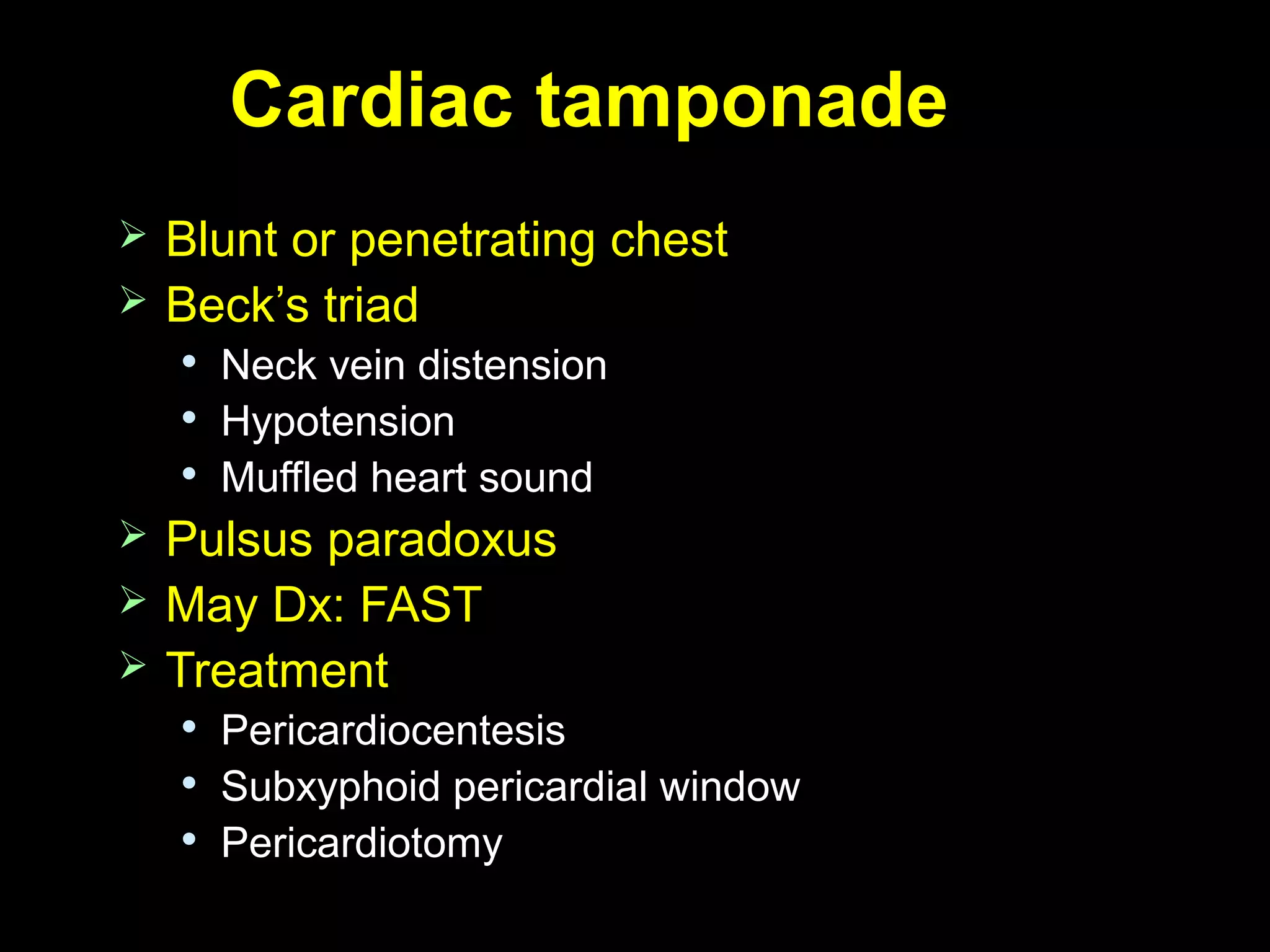
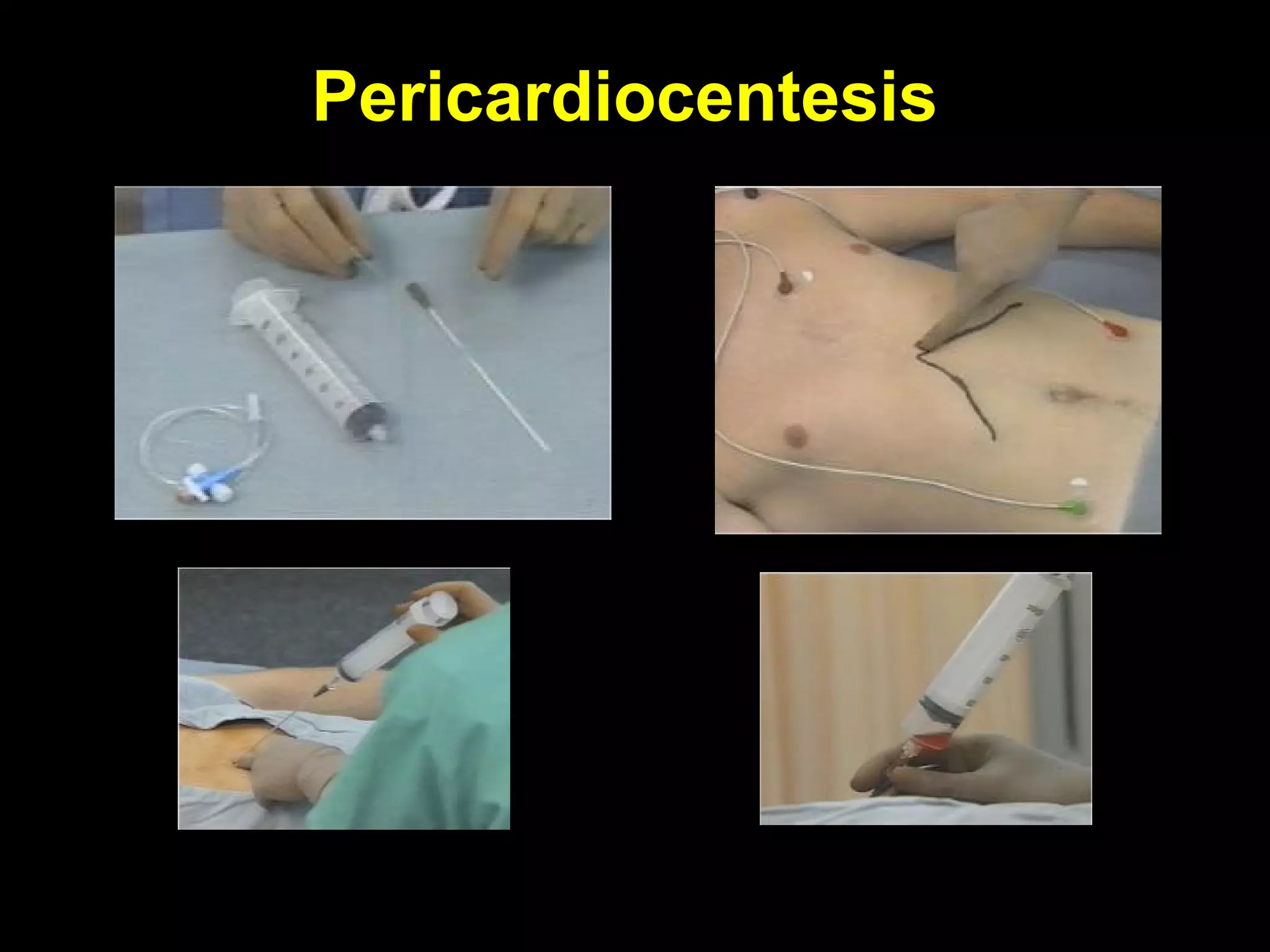
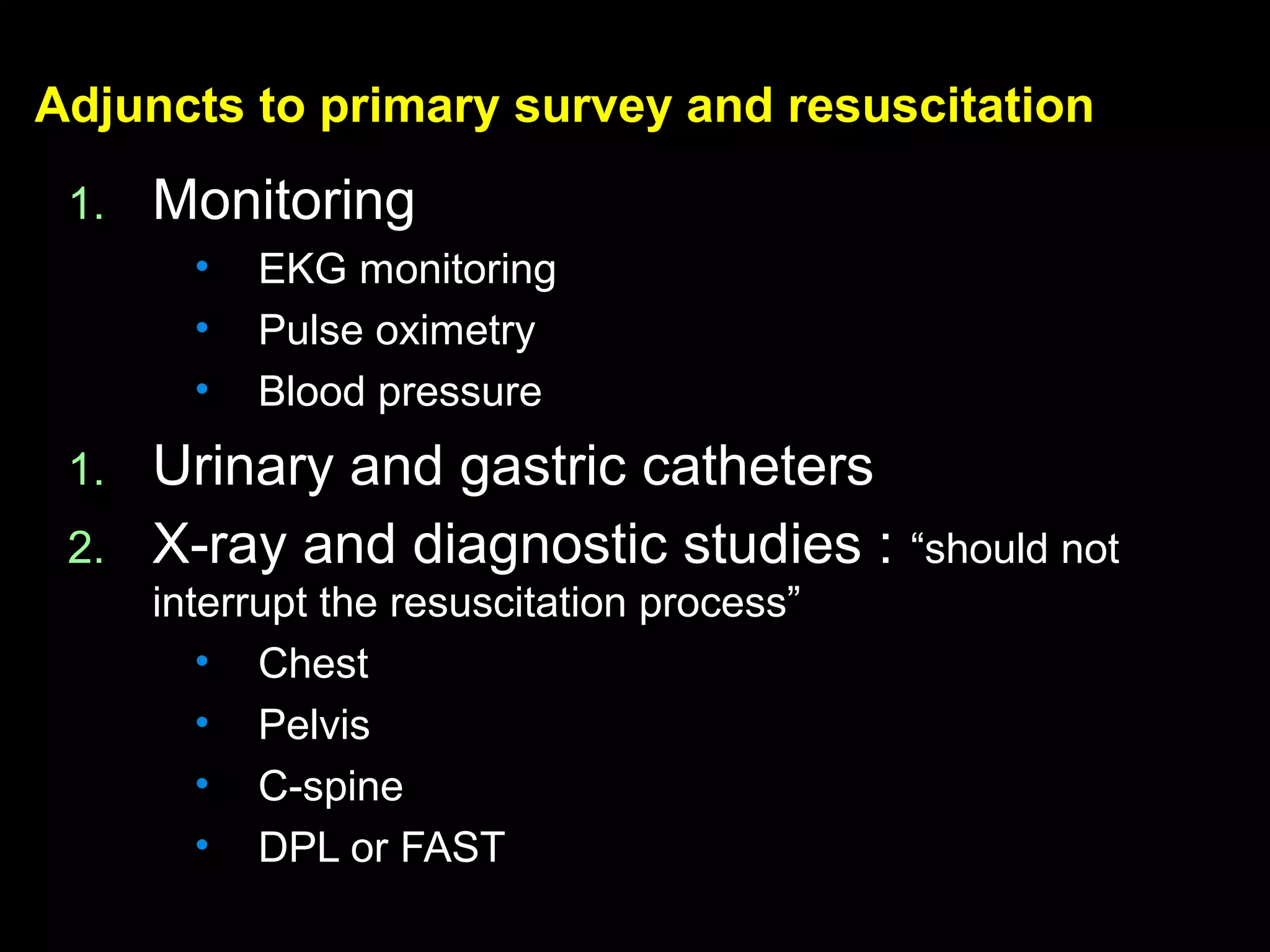
1. The document discusses the initial assessment and management of trauma patients, including the primary and secondary surveys. Key steps include airway management, breathing and ventilation, circulation control and hemorrhage management.
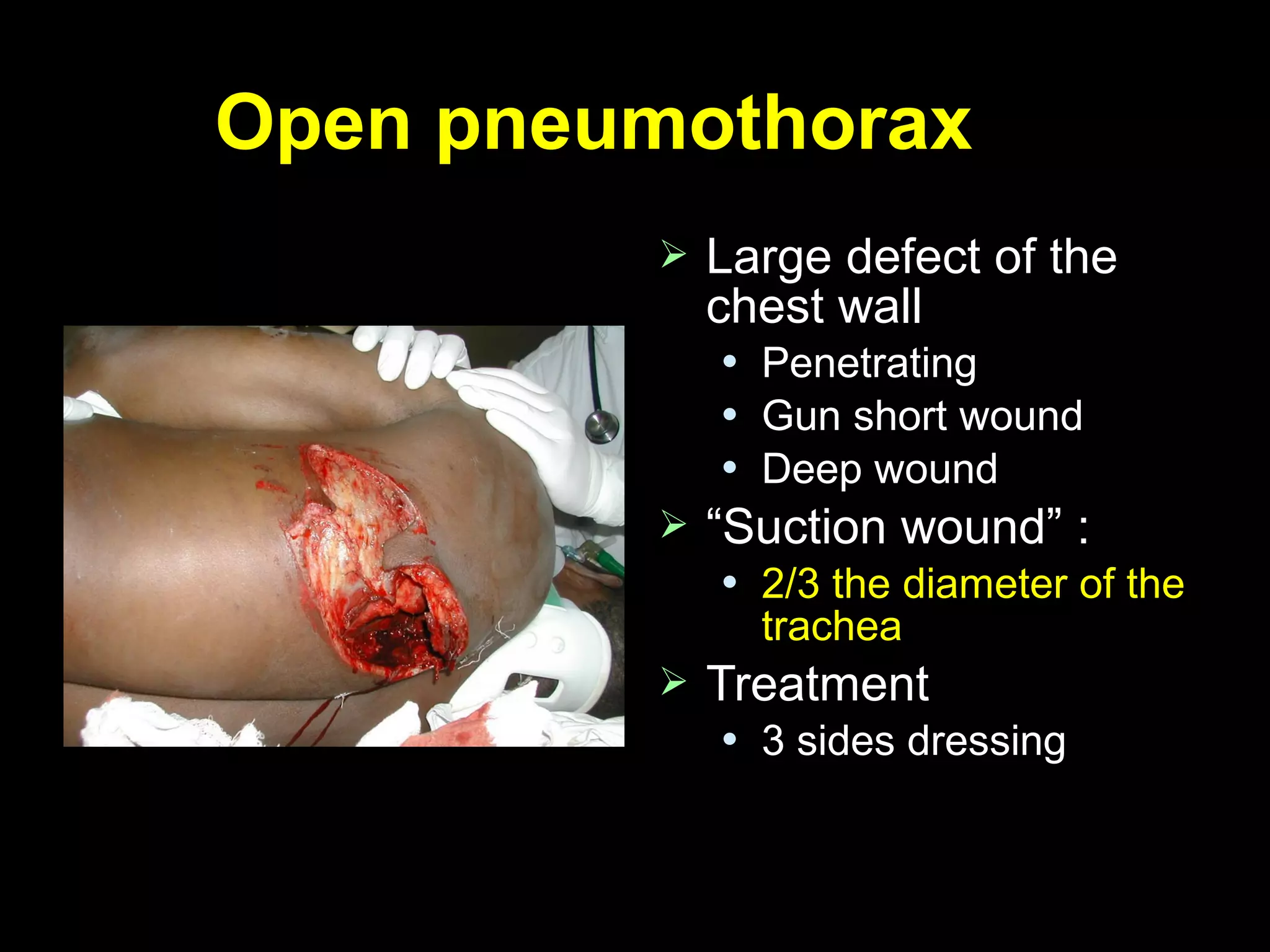
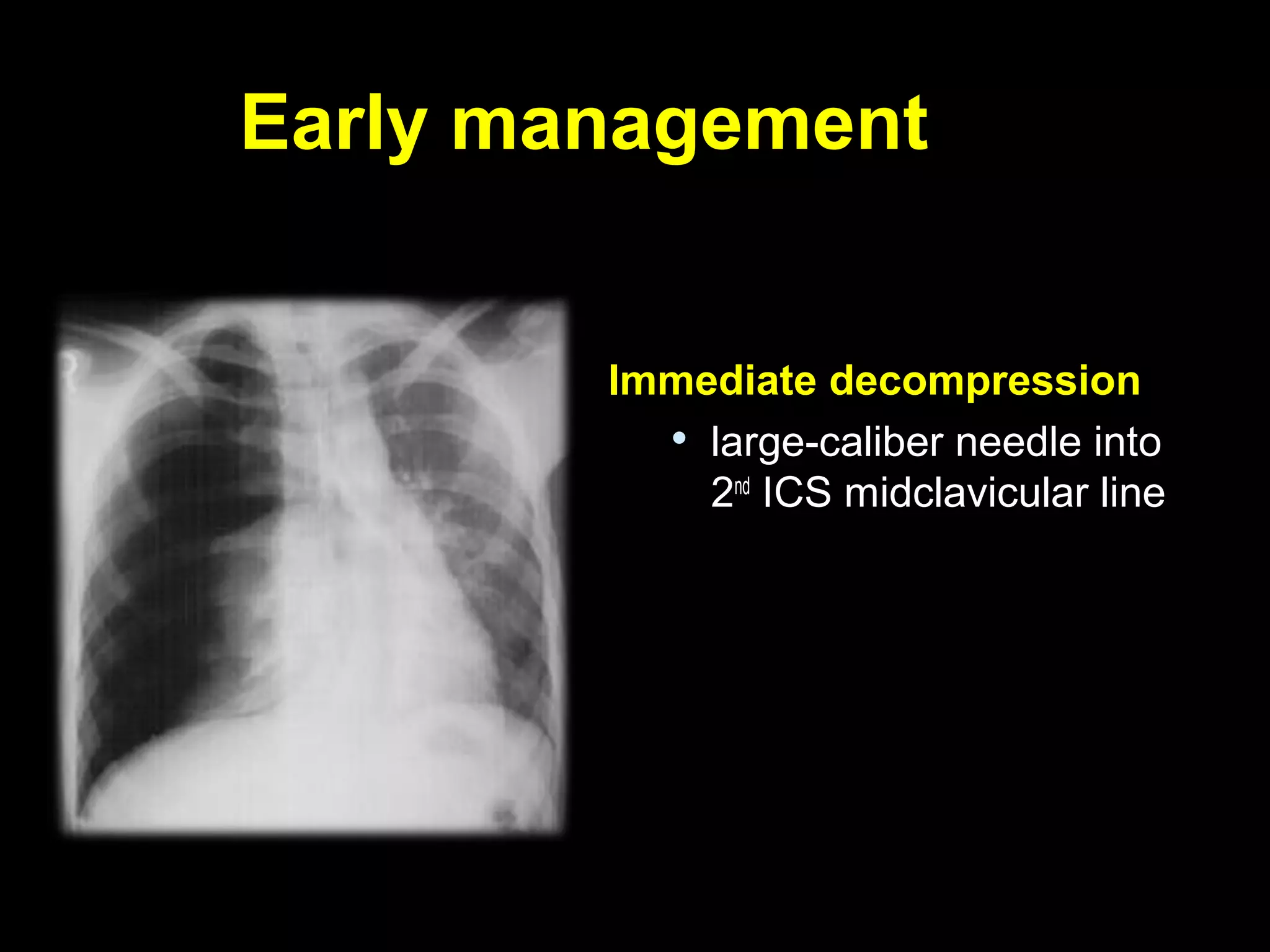
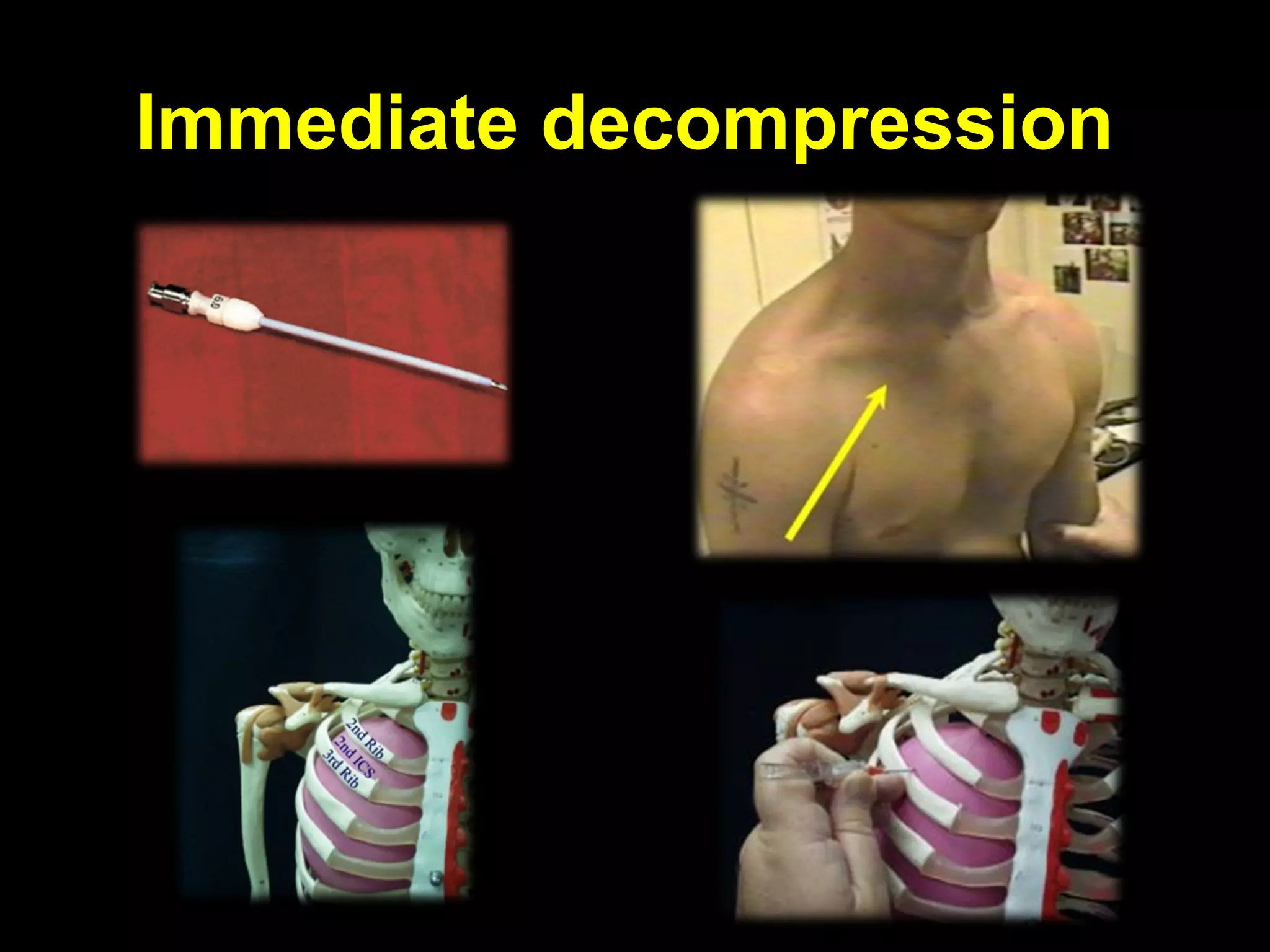
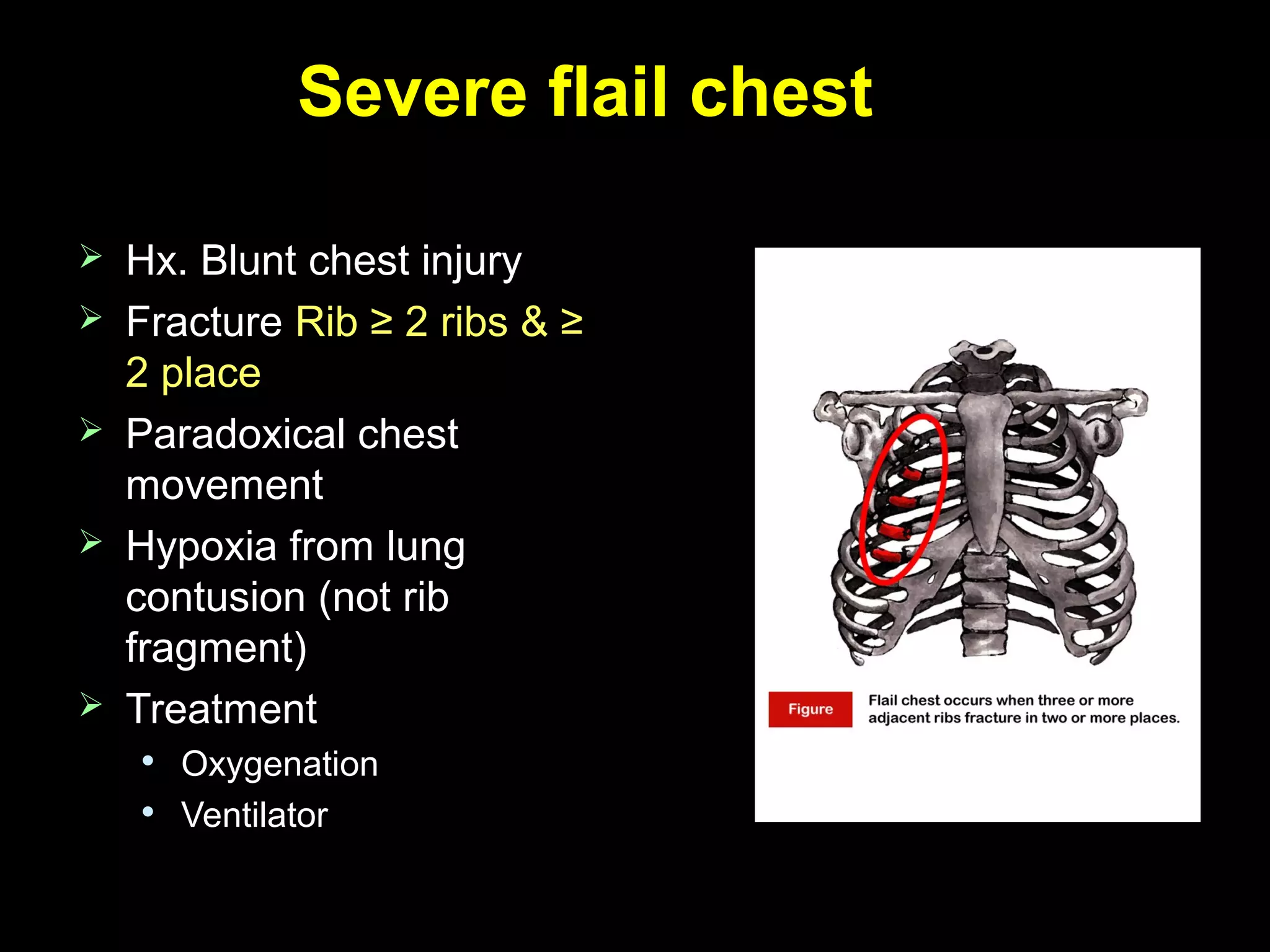
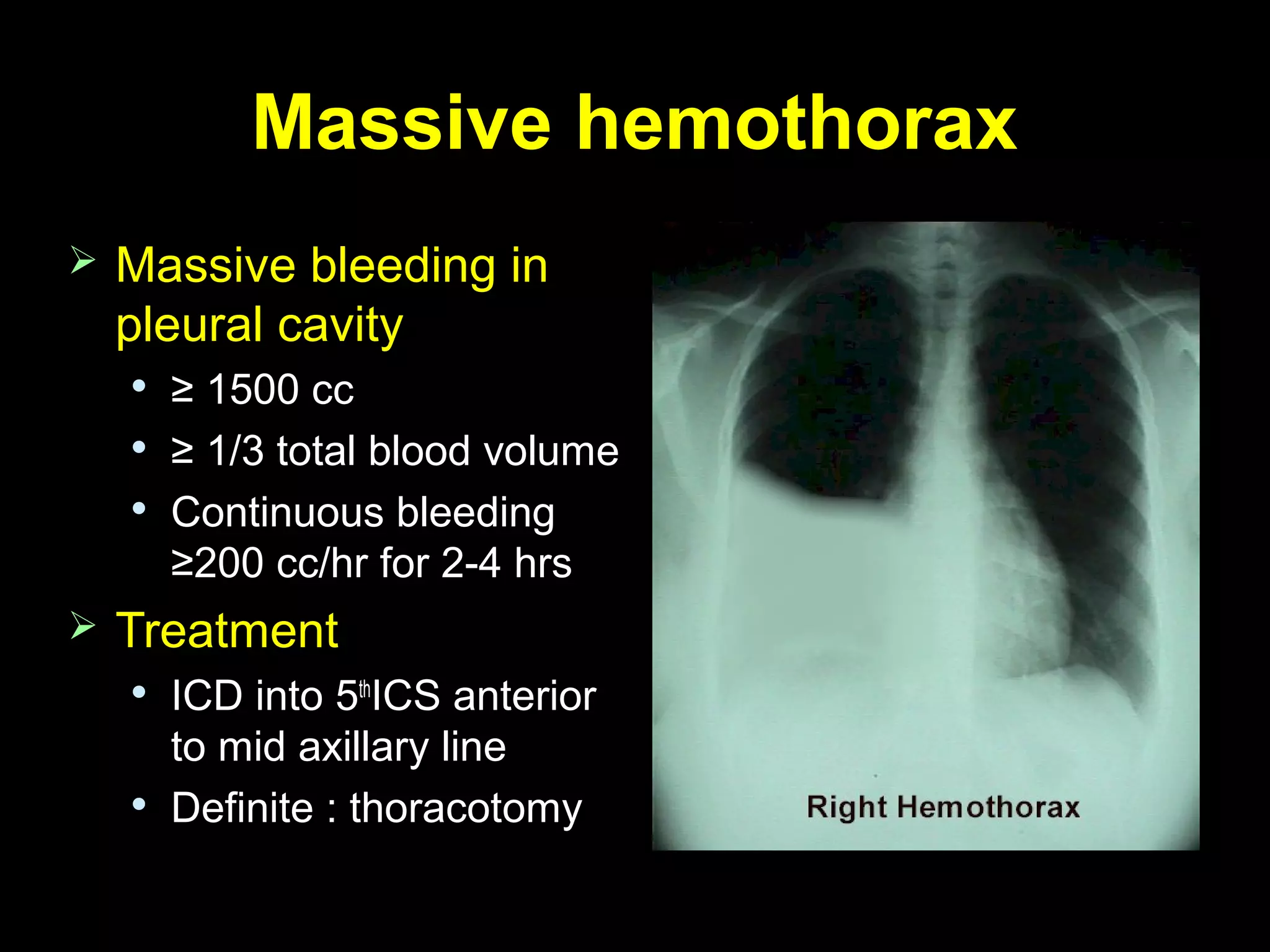
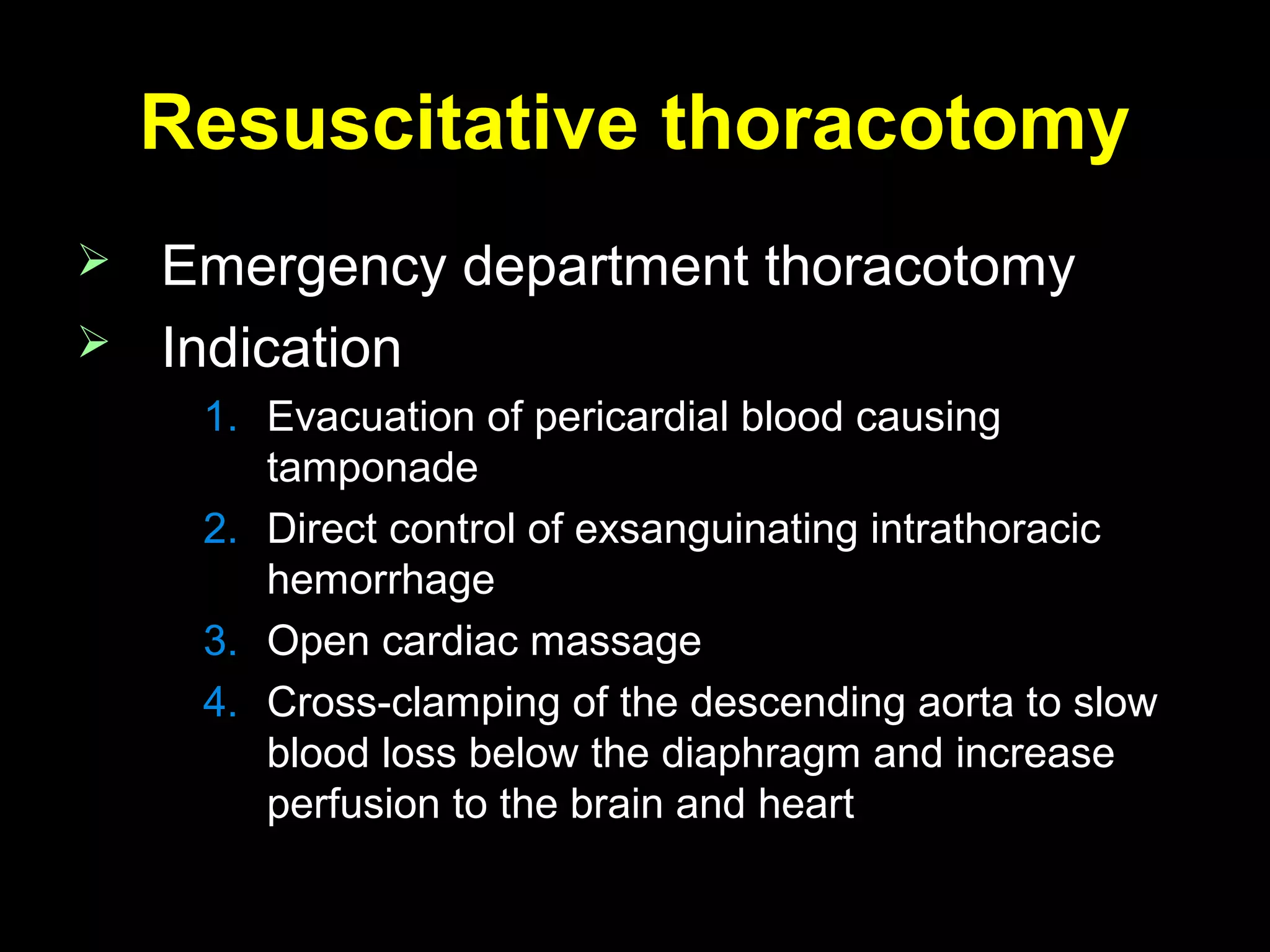
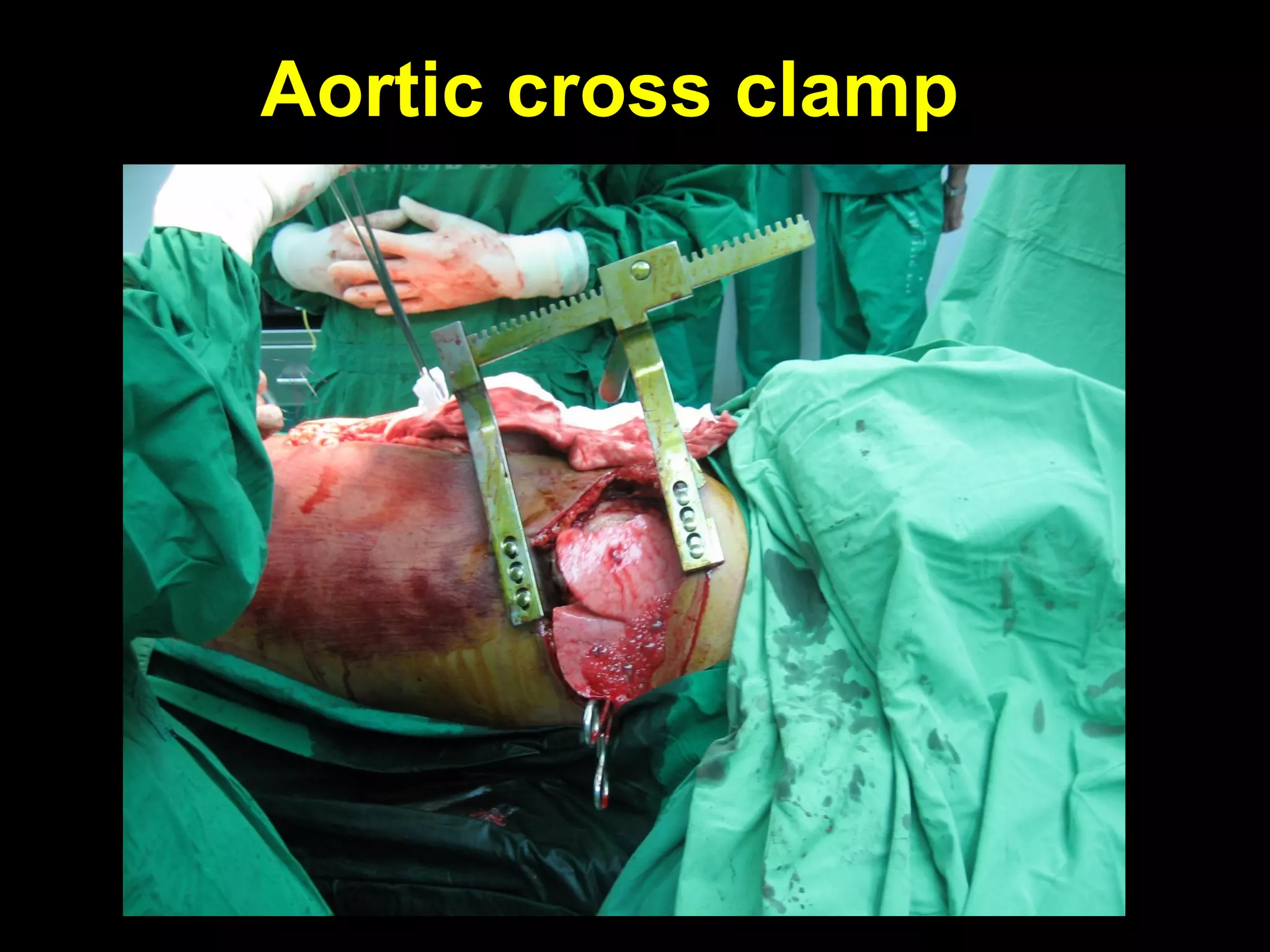
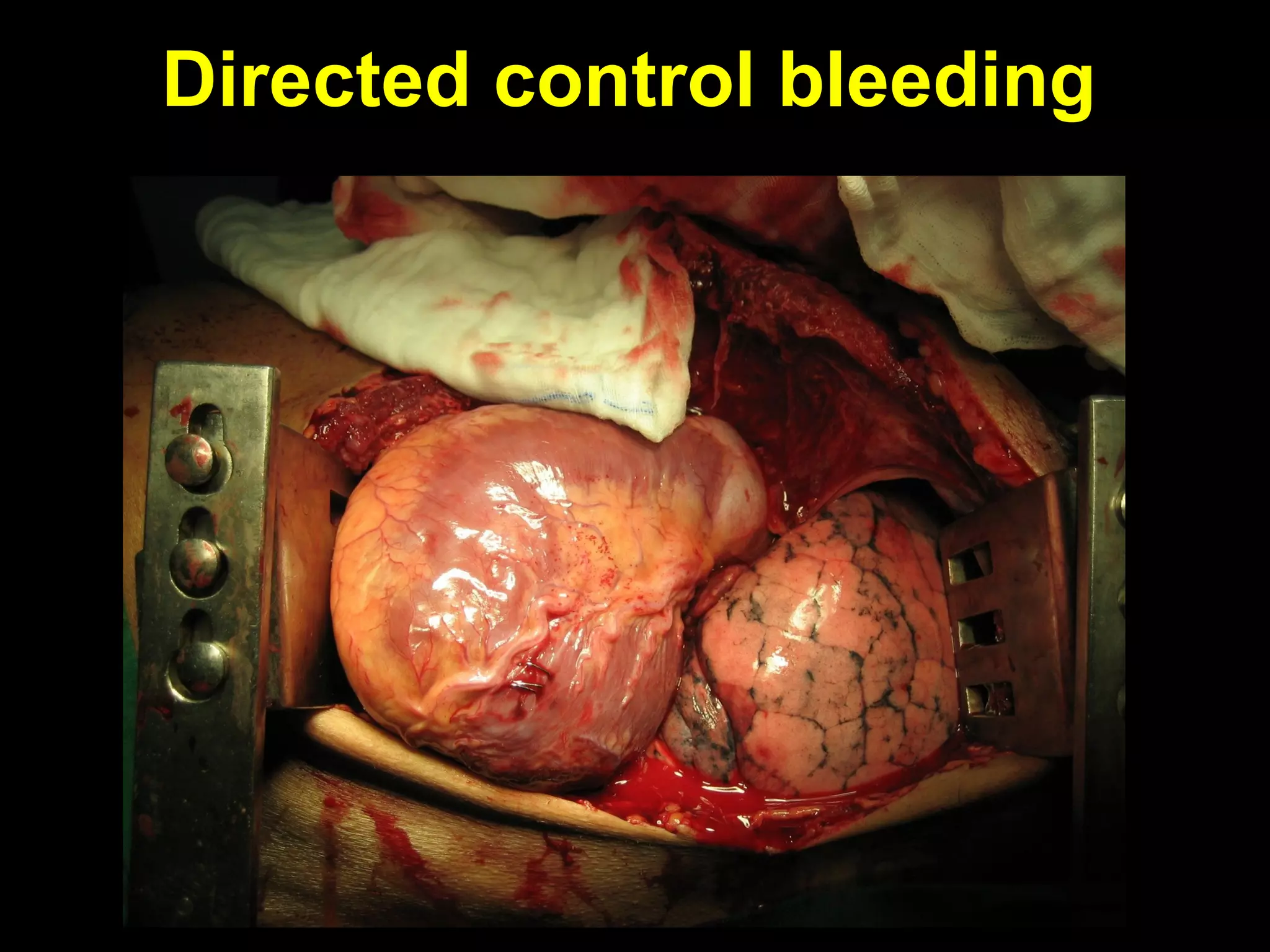
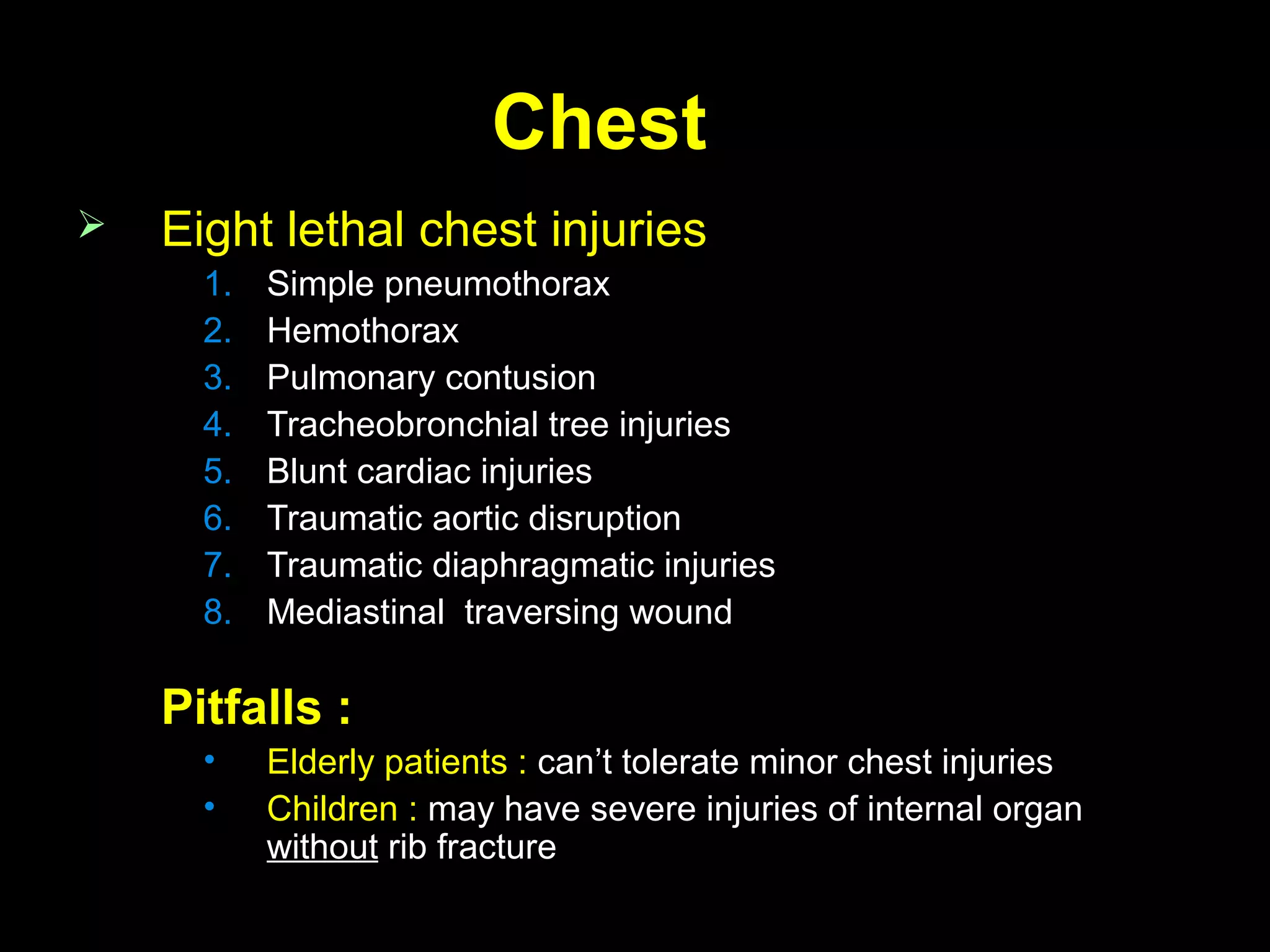
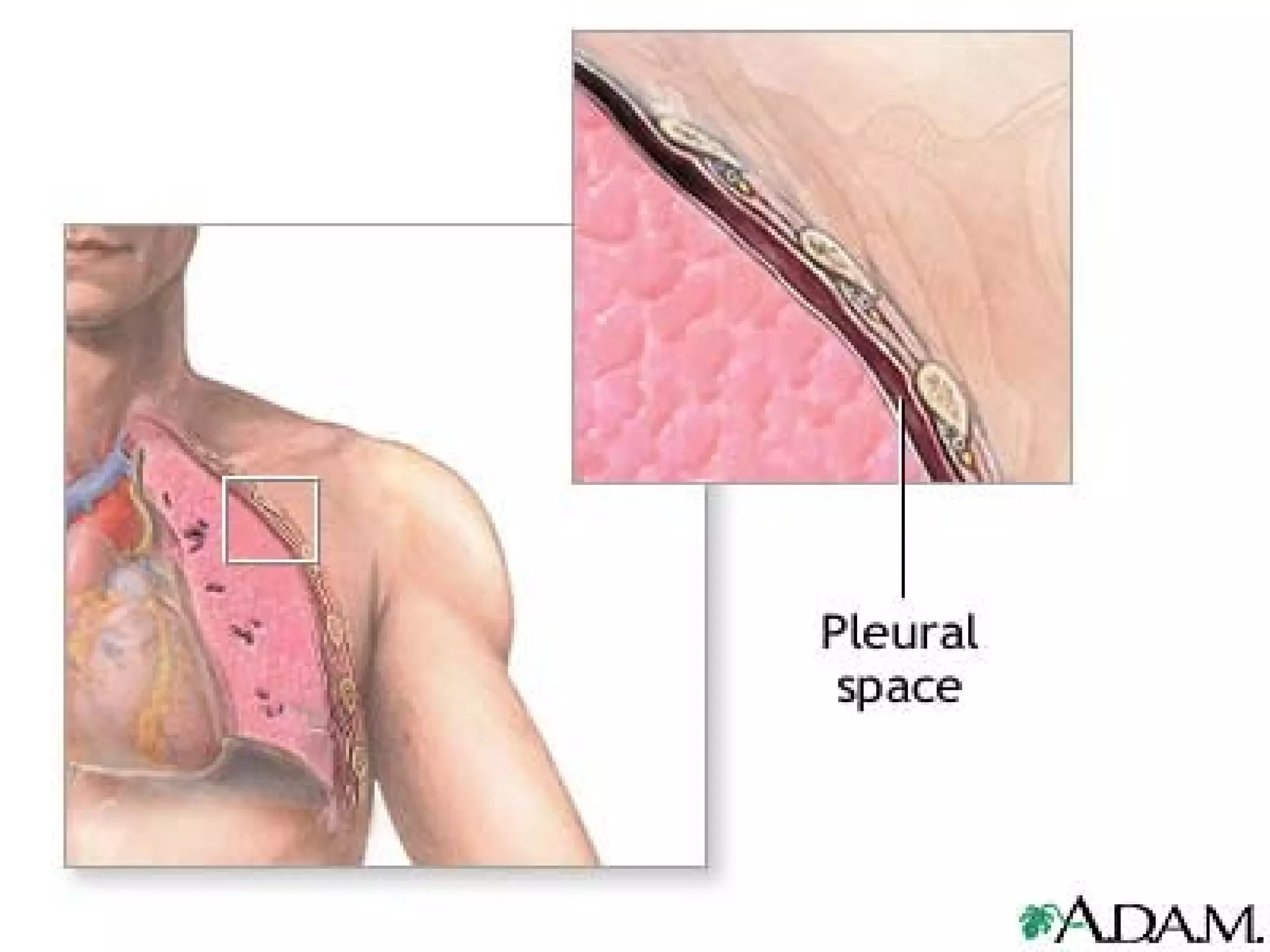
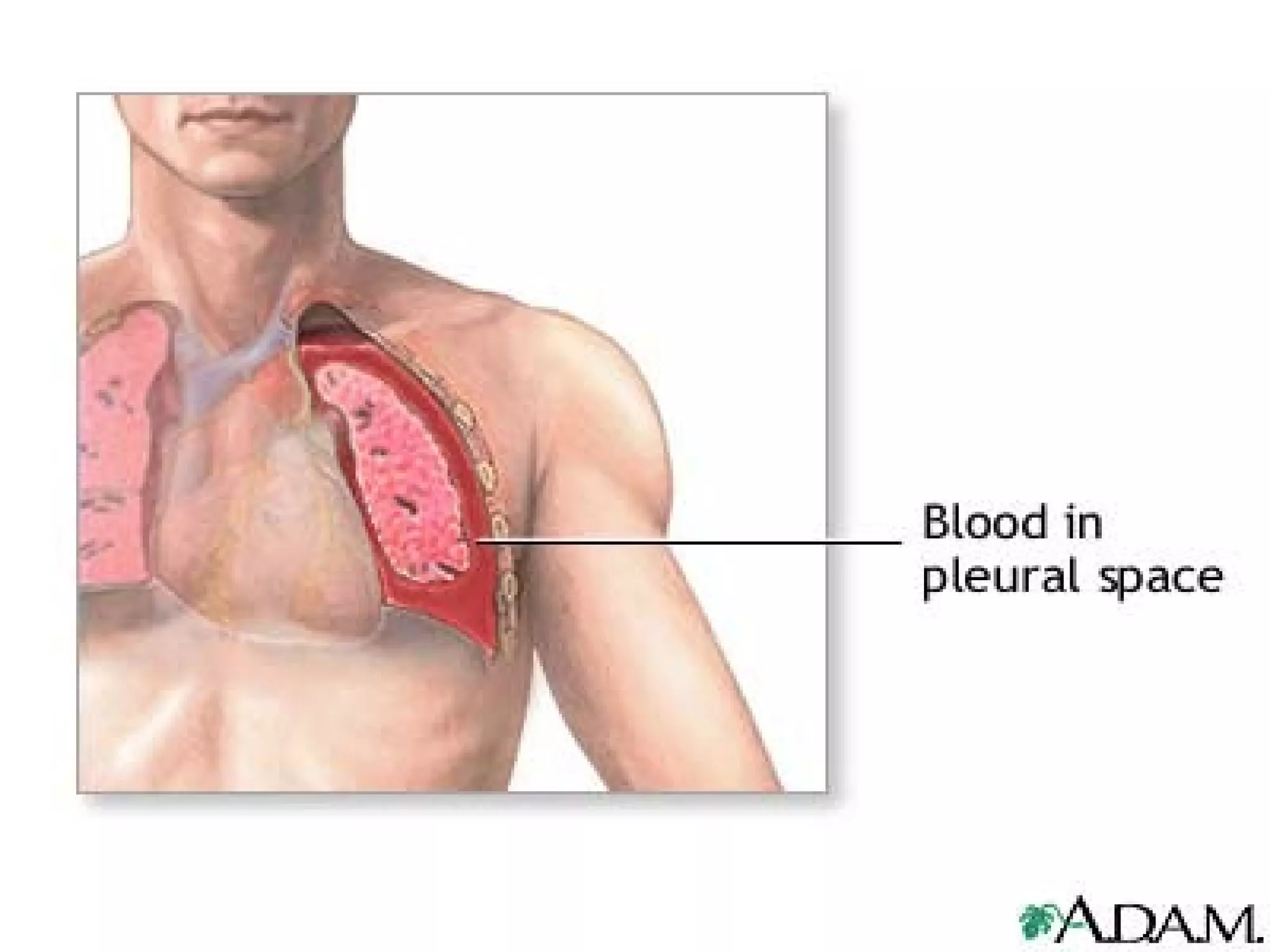
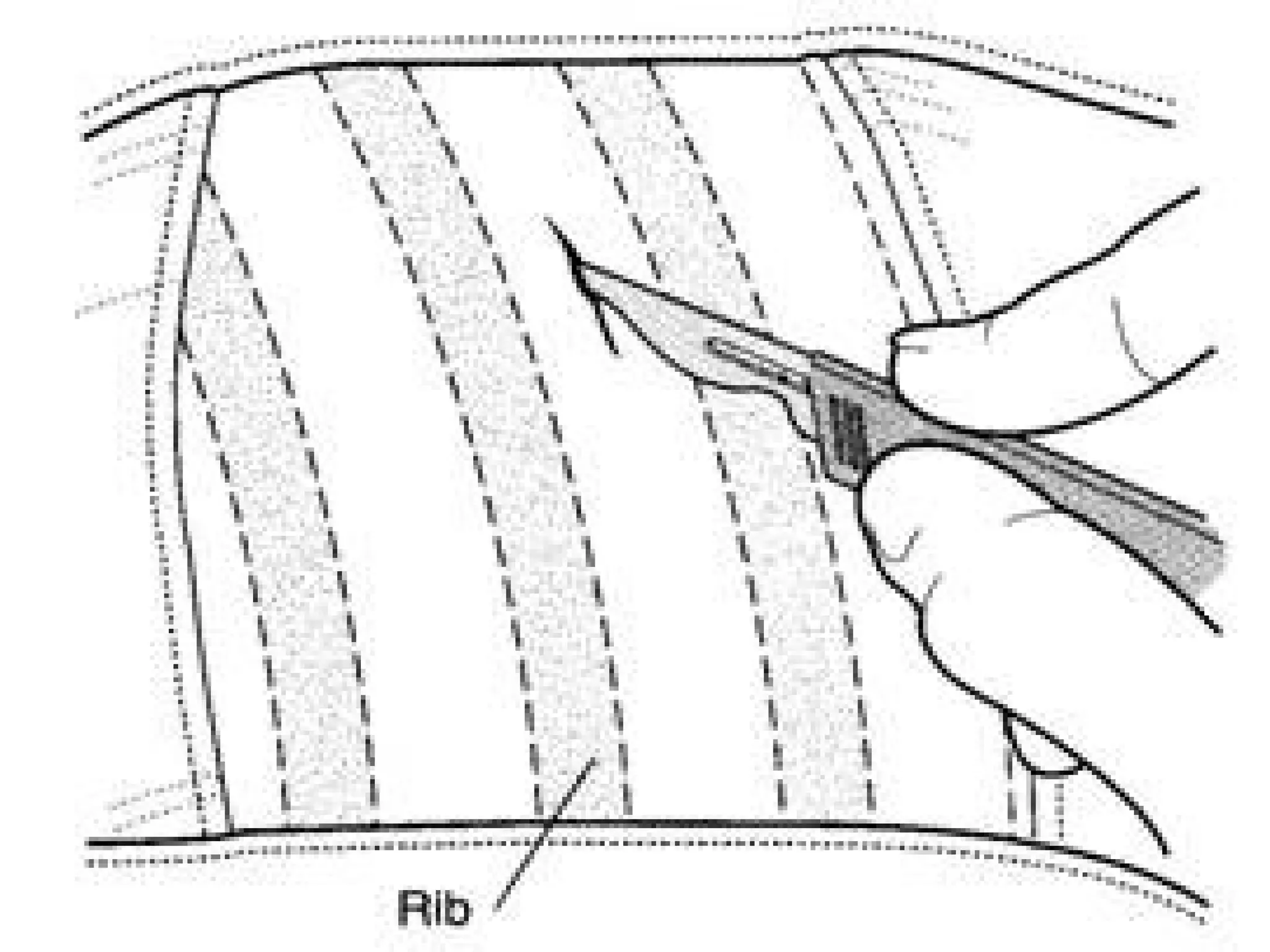
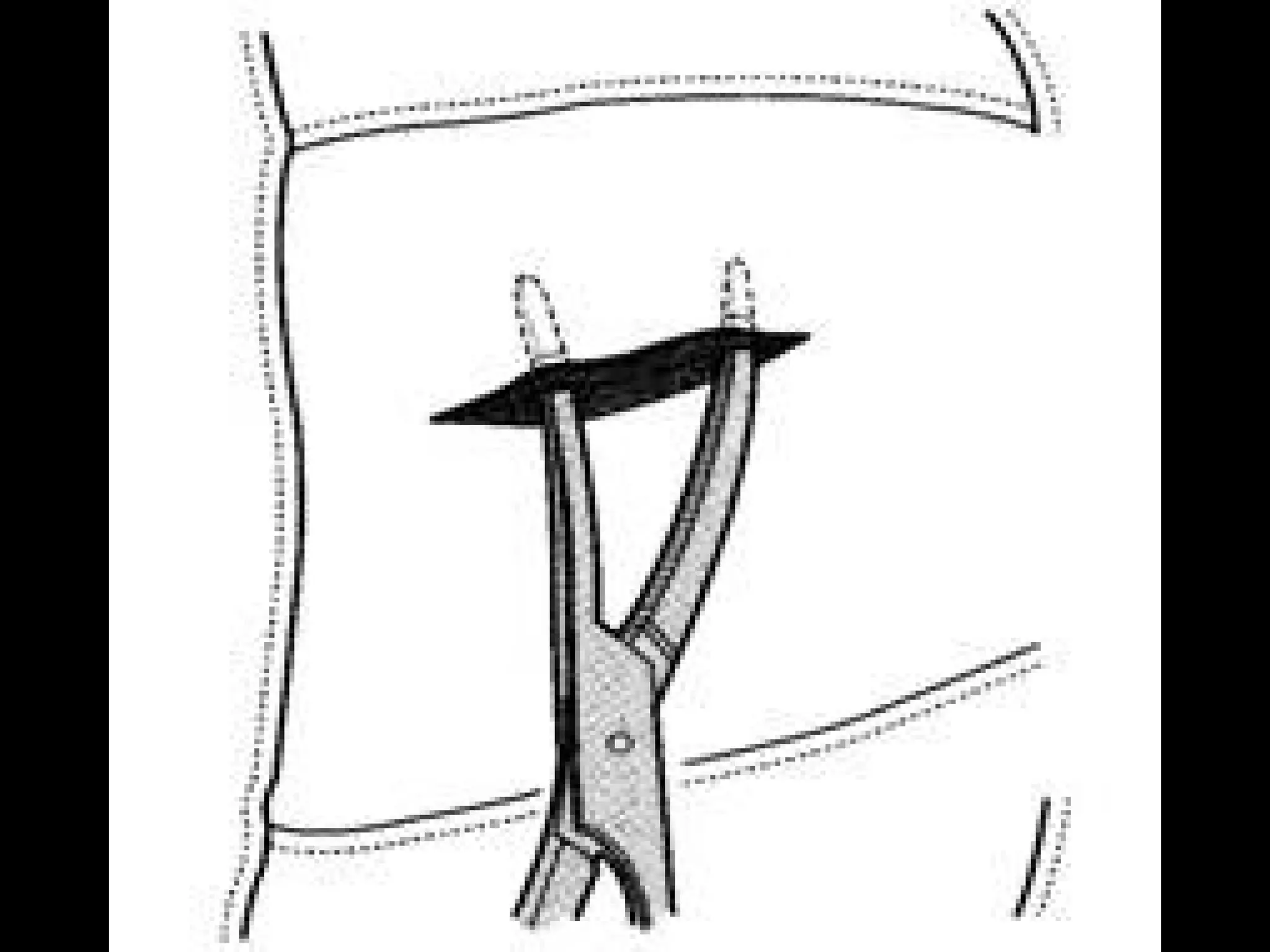
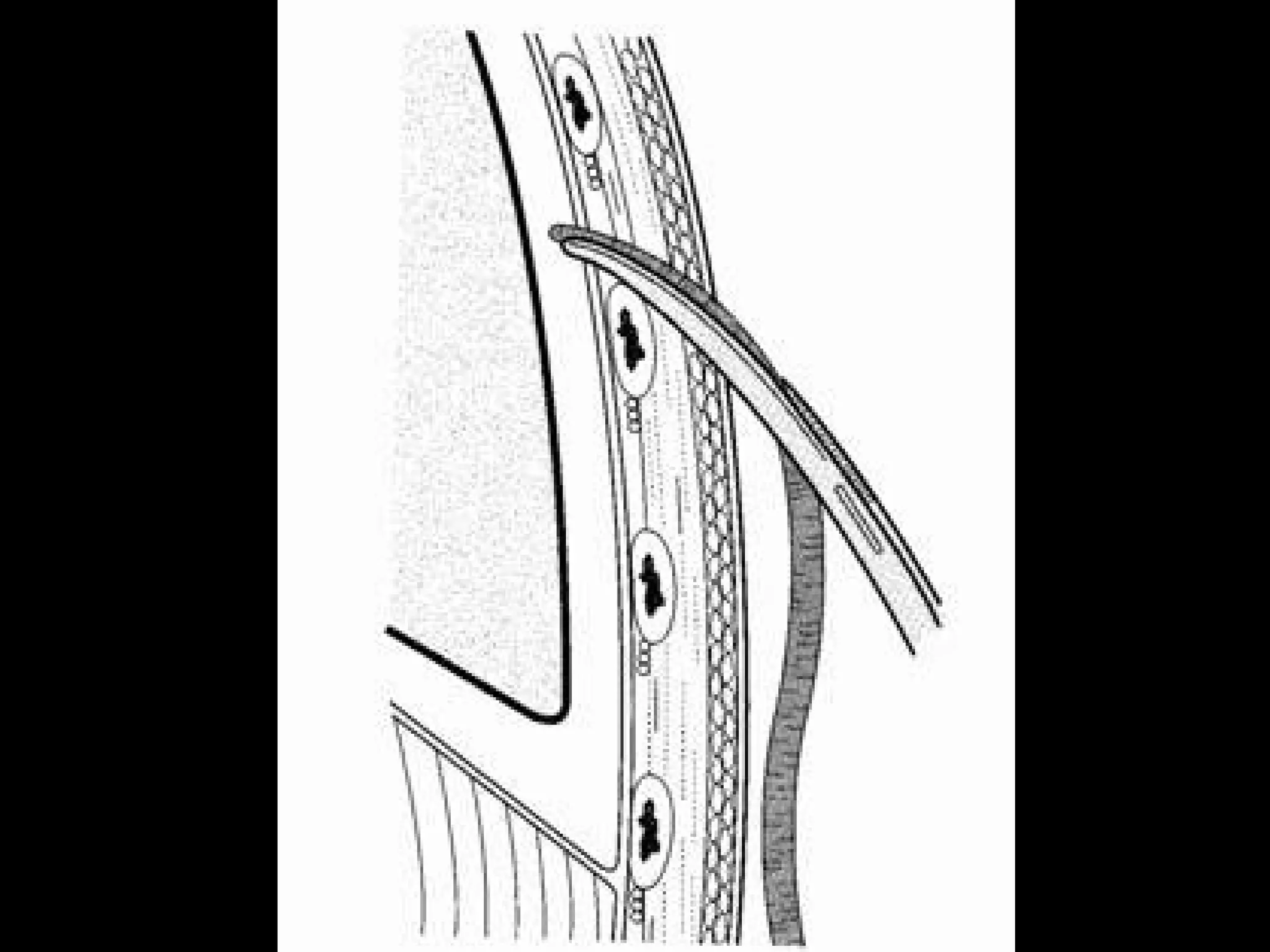
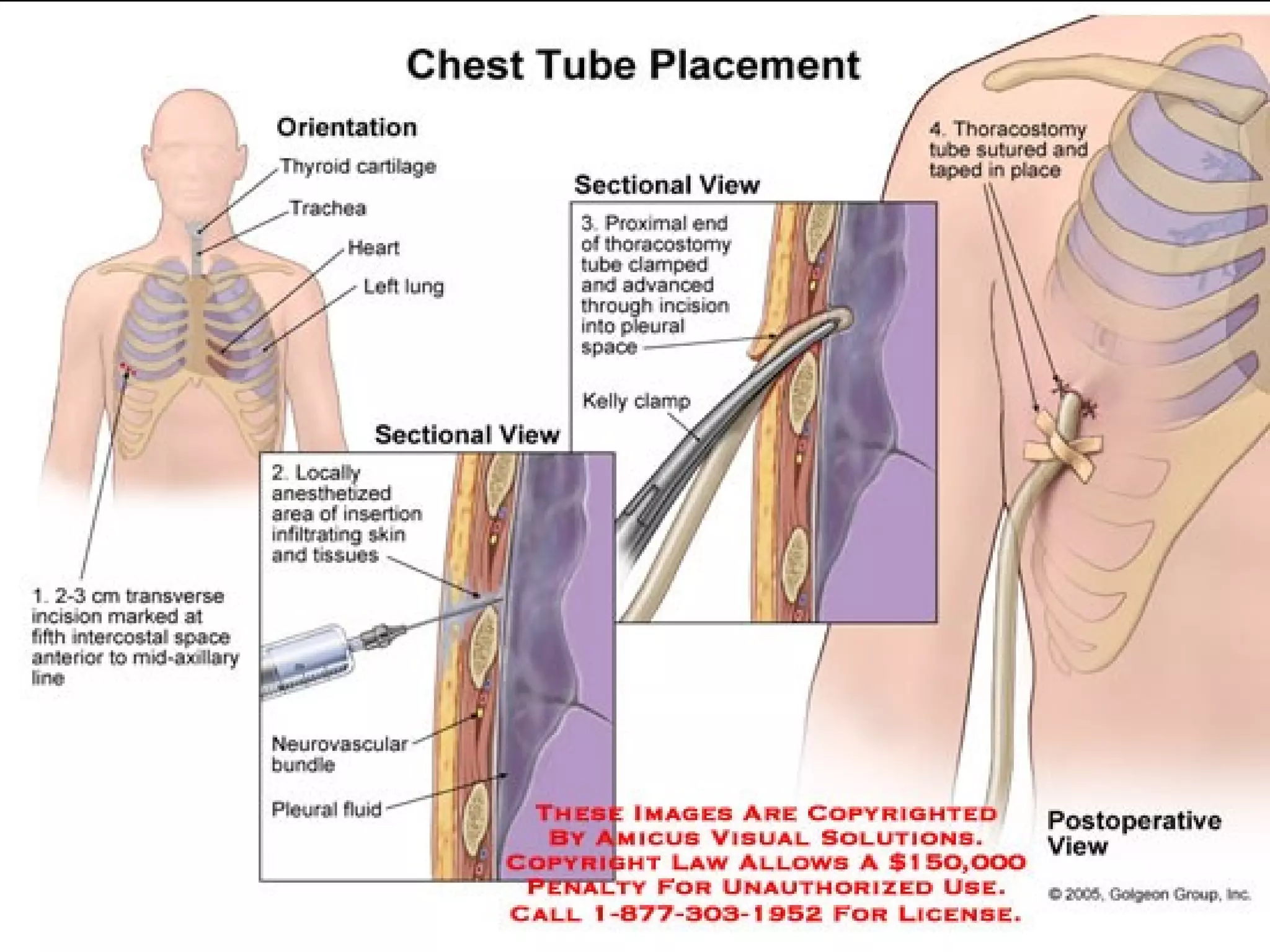
2. Immediate life-threatening conditions addressed in the primary survey are outlined, such as tension pneumothorax, massive hemorrhage. Techniques for airway control, needle decompression and bleeding control are described.
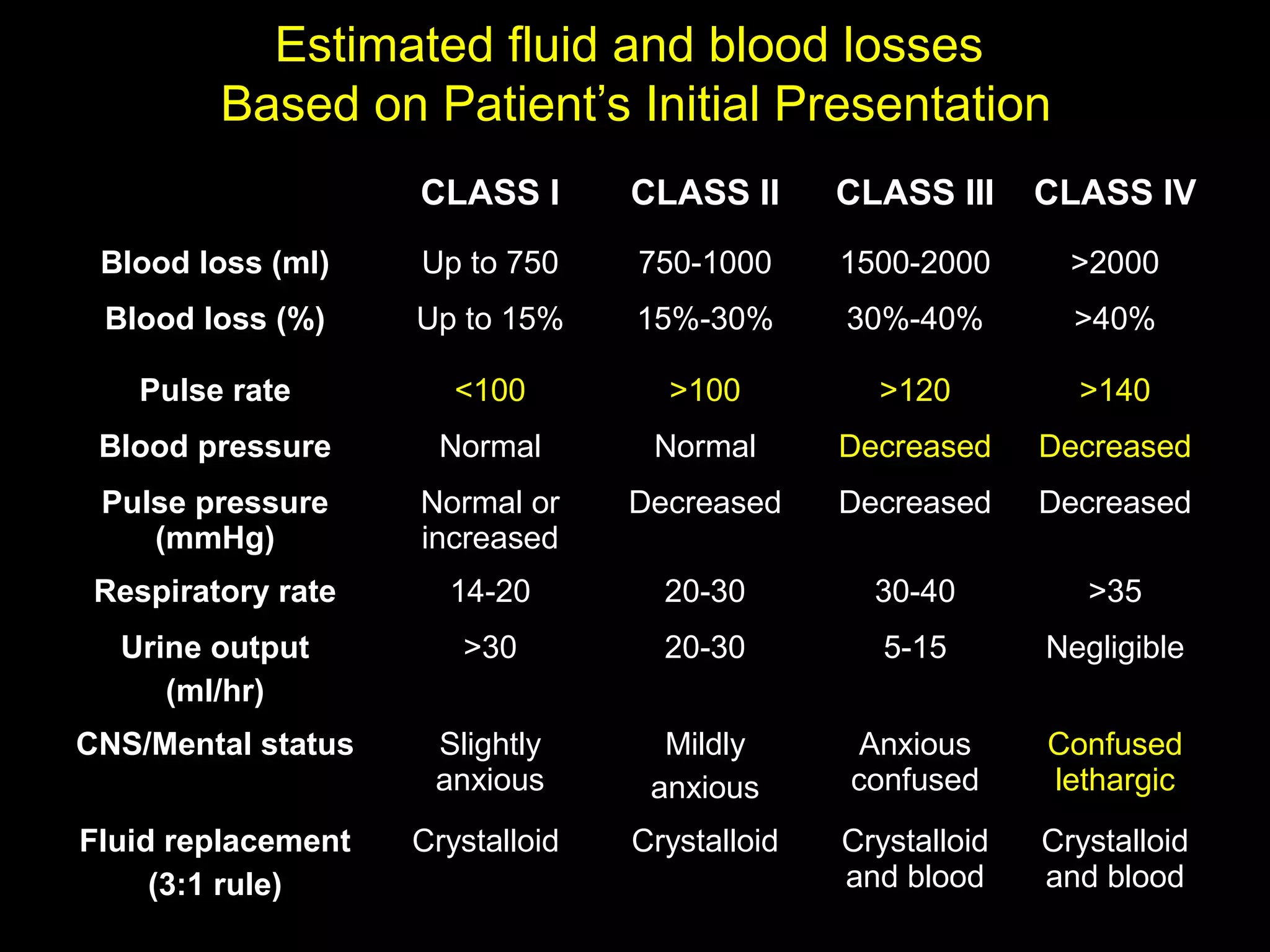
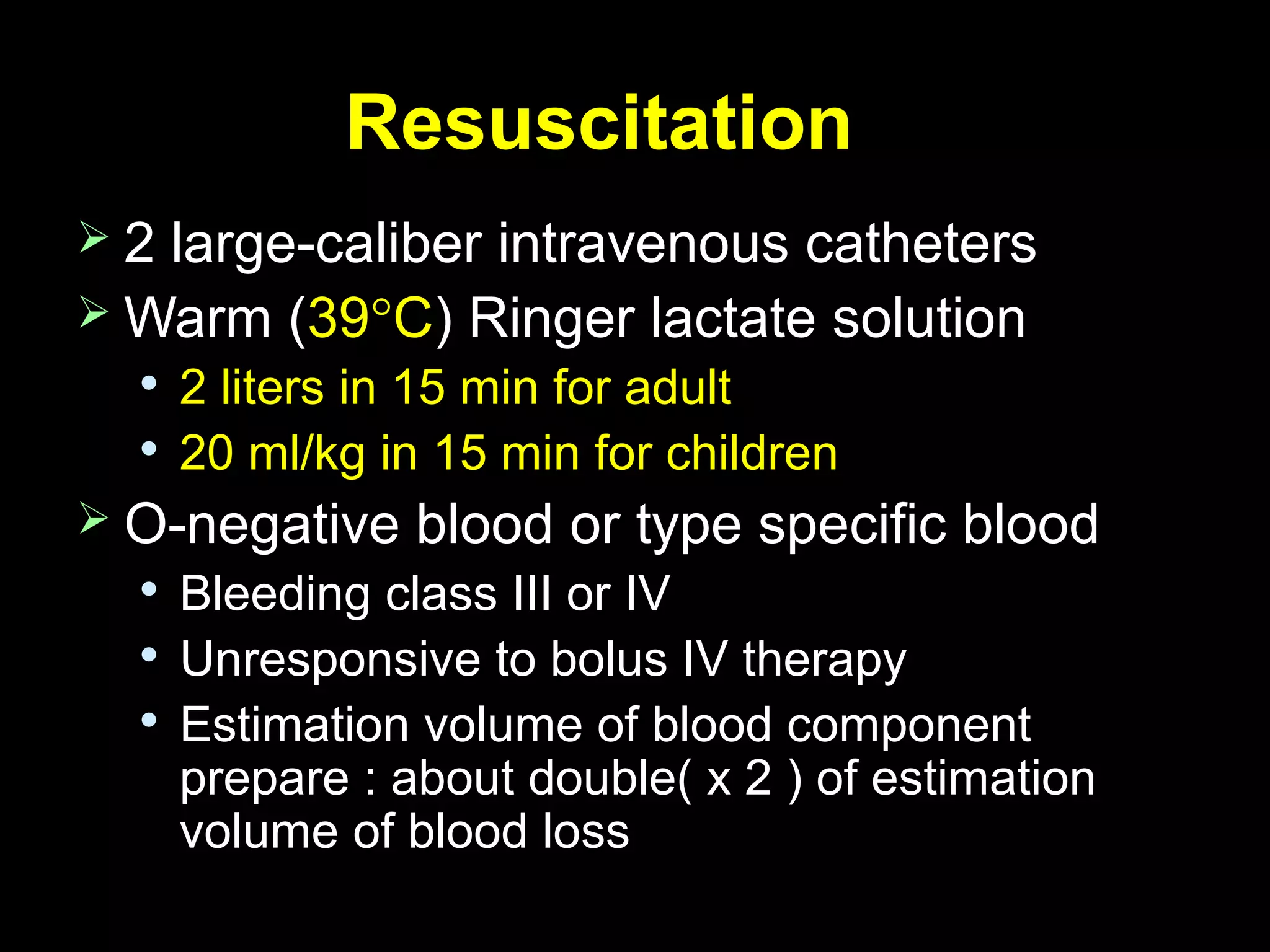
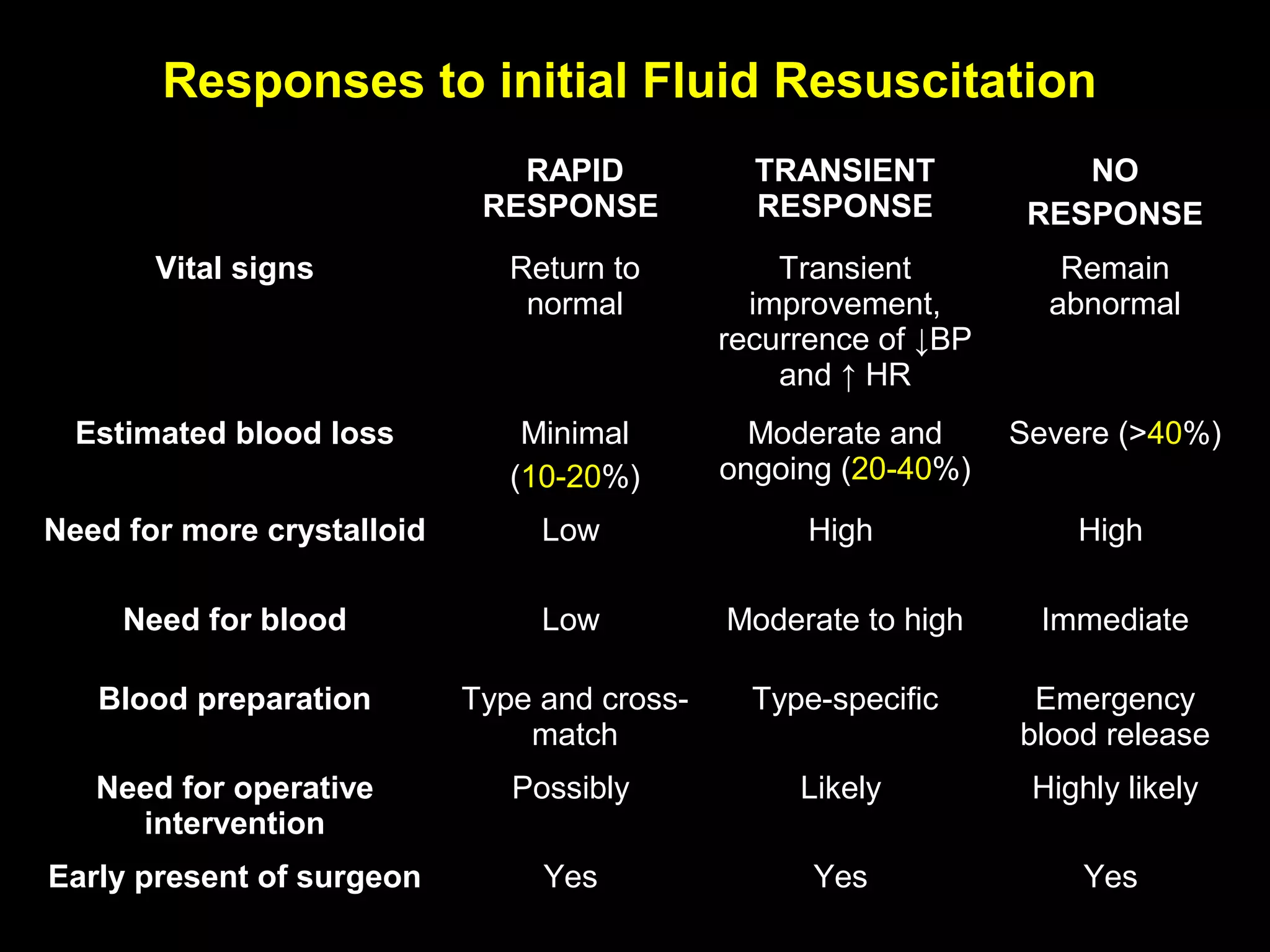
3. Estimation of blood and fluid loss is provided to guide volume resuscitation. Maintaining normothermia during resuscitation is also emphasized.