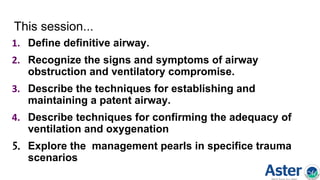
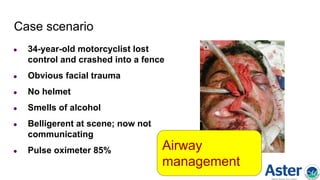
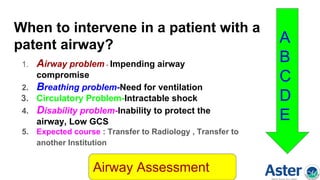
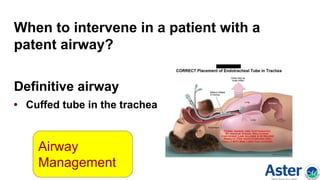
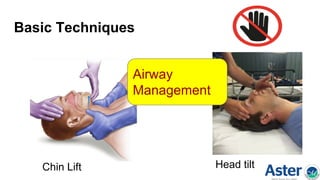
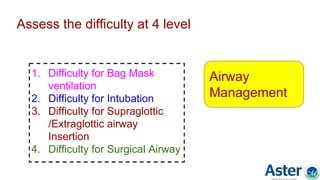
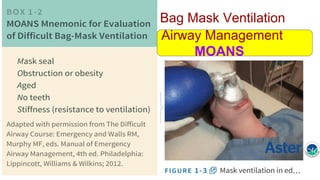
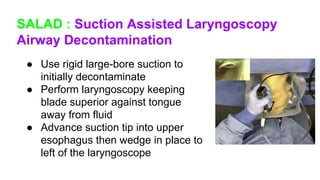
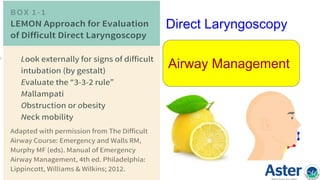
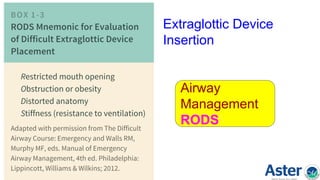
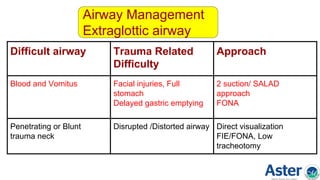
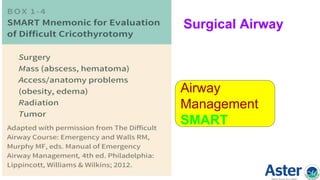
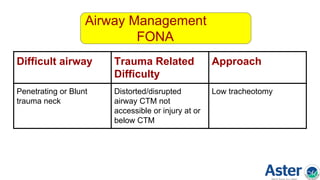
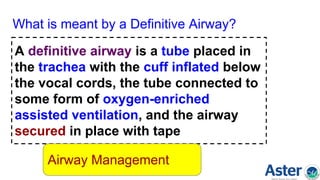
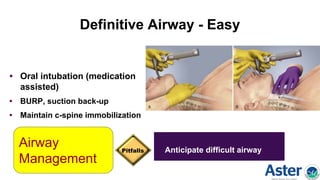
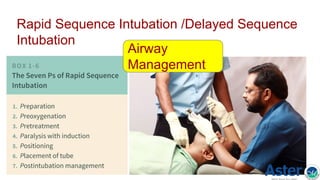
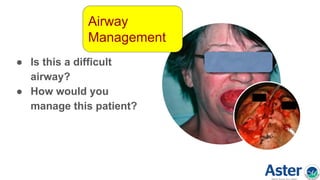
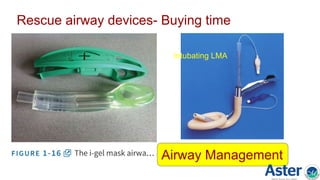
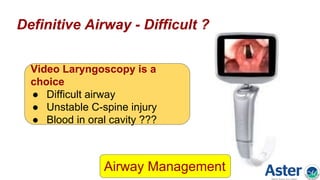
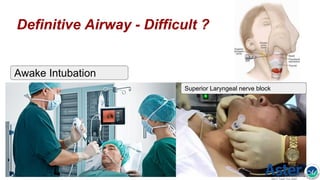
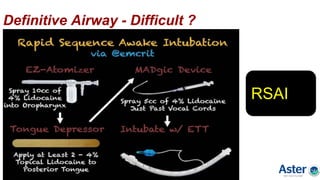
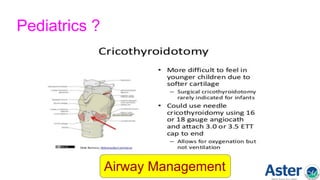
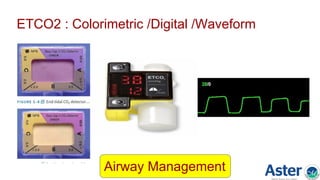
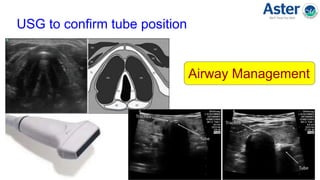
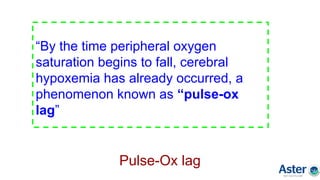
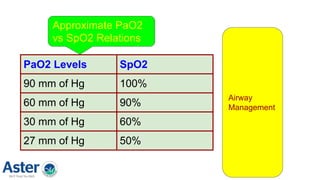
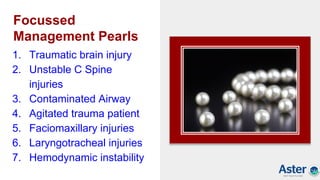
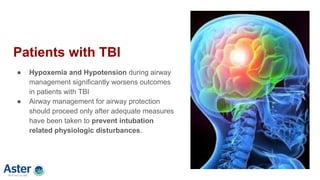
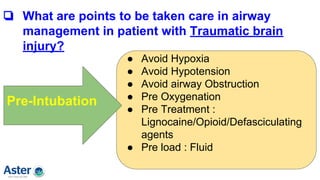
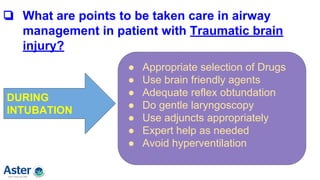
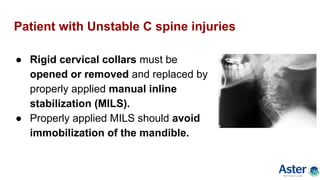
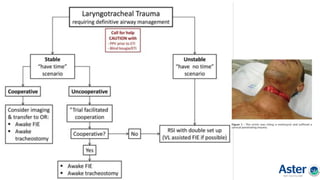
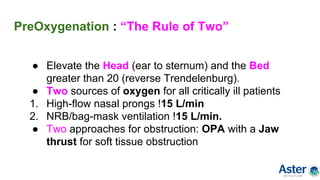
The document discusses advanced airway management in polytrauma, emphasizing the need for maintaining a protected airway and adequate ventilation as paramount priorities. It outlines the signs of airway compromise, assessment techniques, and critical interventions for trauma patients, including specific scenarios and management pearls for conditions like traumatic brain injury and unstable cervical spine injuries. Additionally, it provides practical tips and guidelines for intubation, confirmation of tube placement, and the use of advanced airway devices in emergencies.