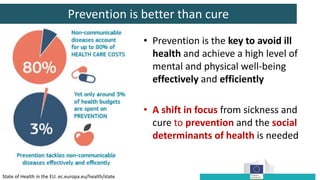
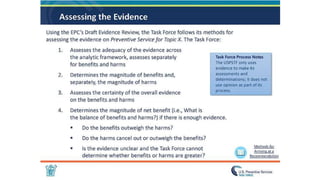
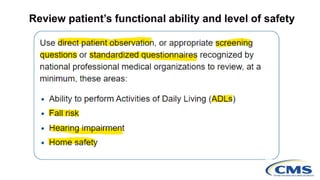
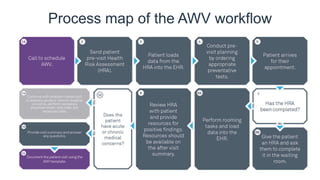
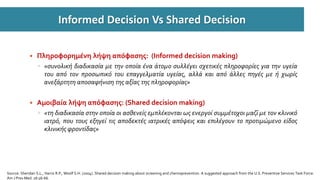
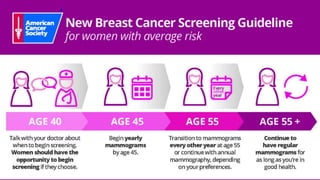
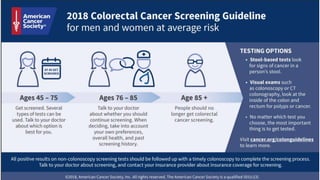
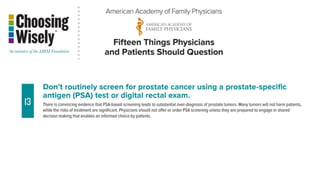
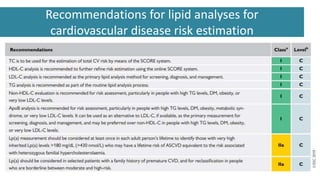
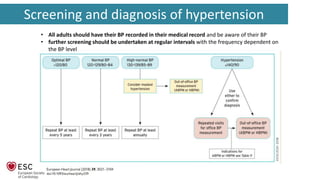
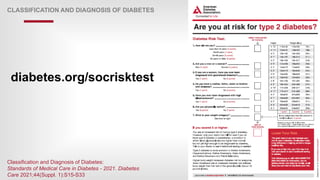
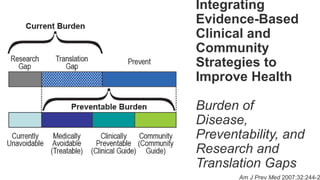
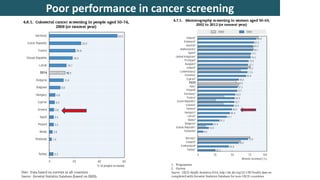
This document discusses the importance of preventive healthcare and screening for early detection of diseases. It provides guidance on screening recommendations and intervals for various common conditions like cancer, cardiovascular disease, diabetes, osteoporosis and others. The risks and benefits of different screening tests are presented to facilitate informed decision making. Emphasis is placed on integrating preventive services and chronic disease management into primary care to improve outcomes and reduce healthcare costs.