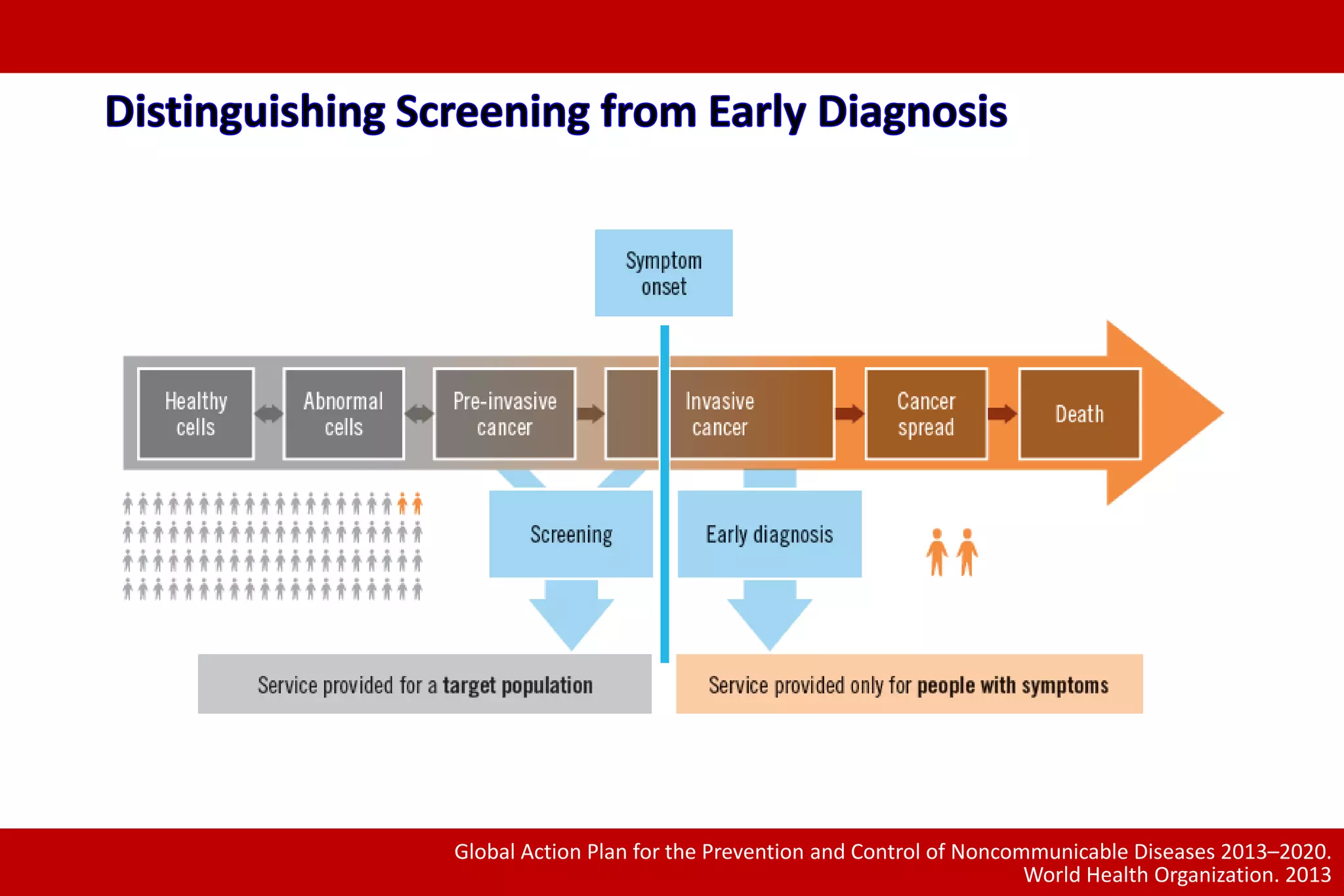
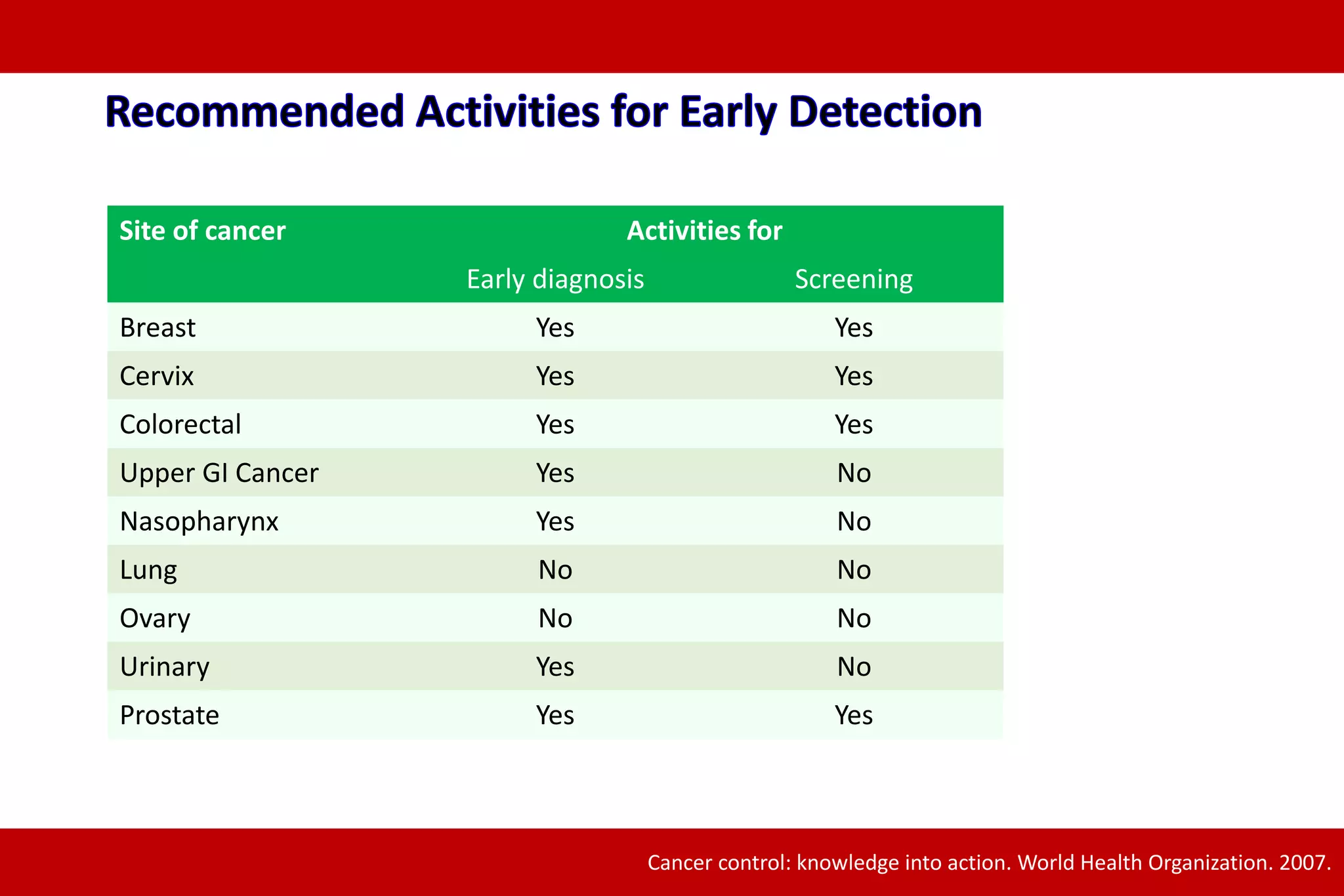
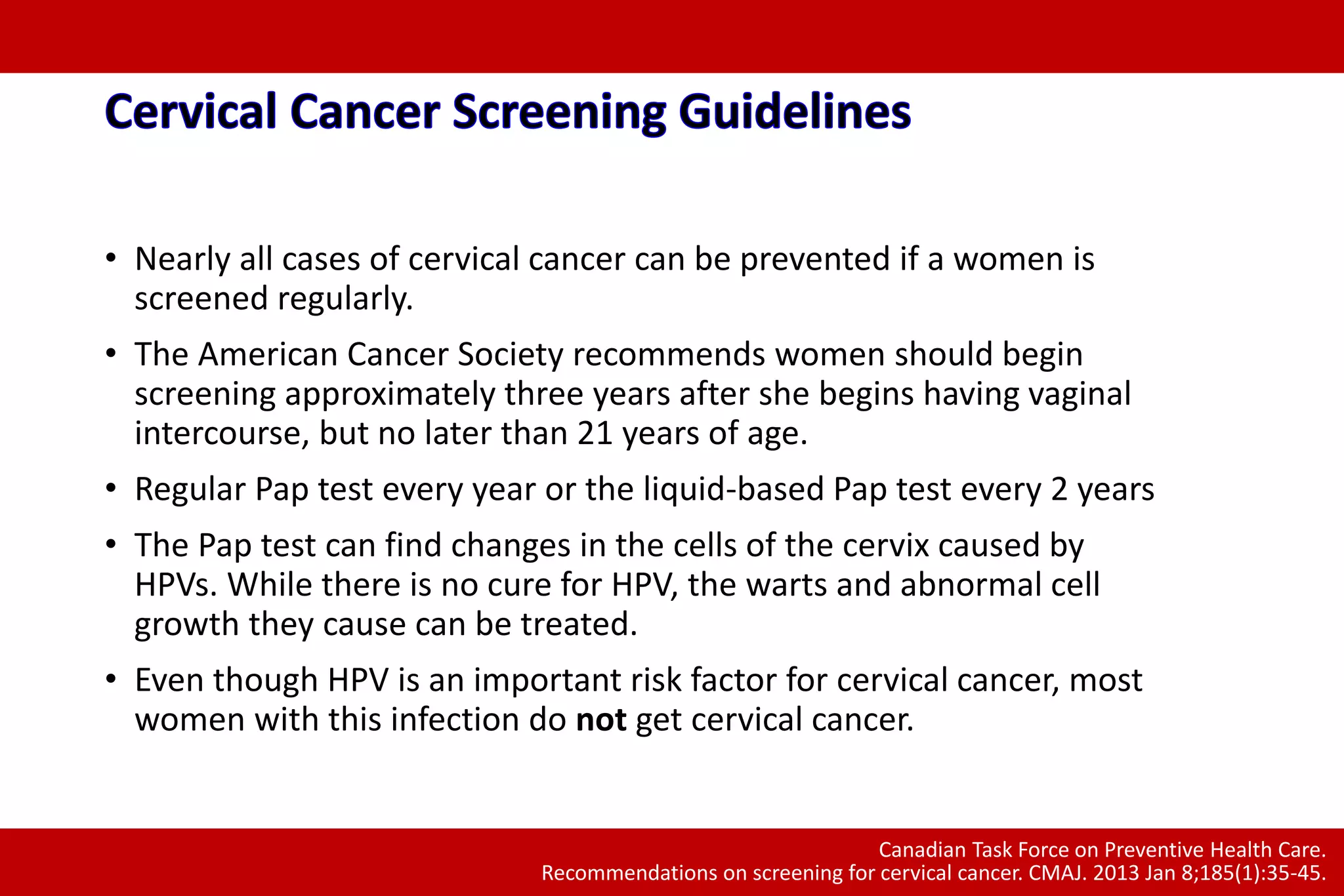
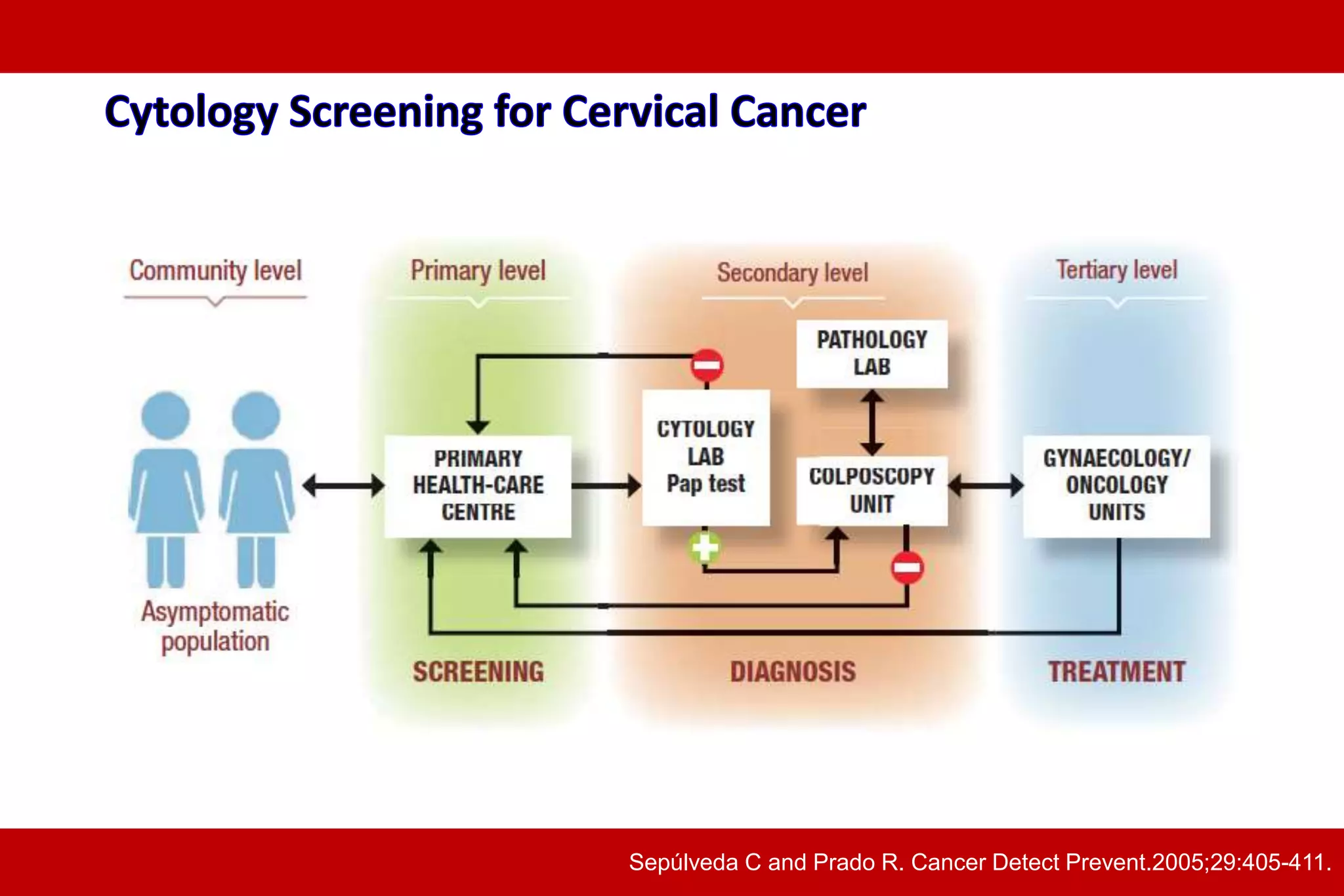
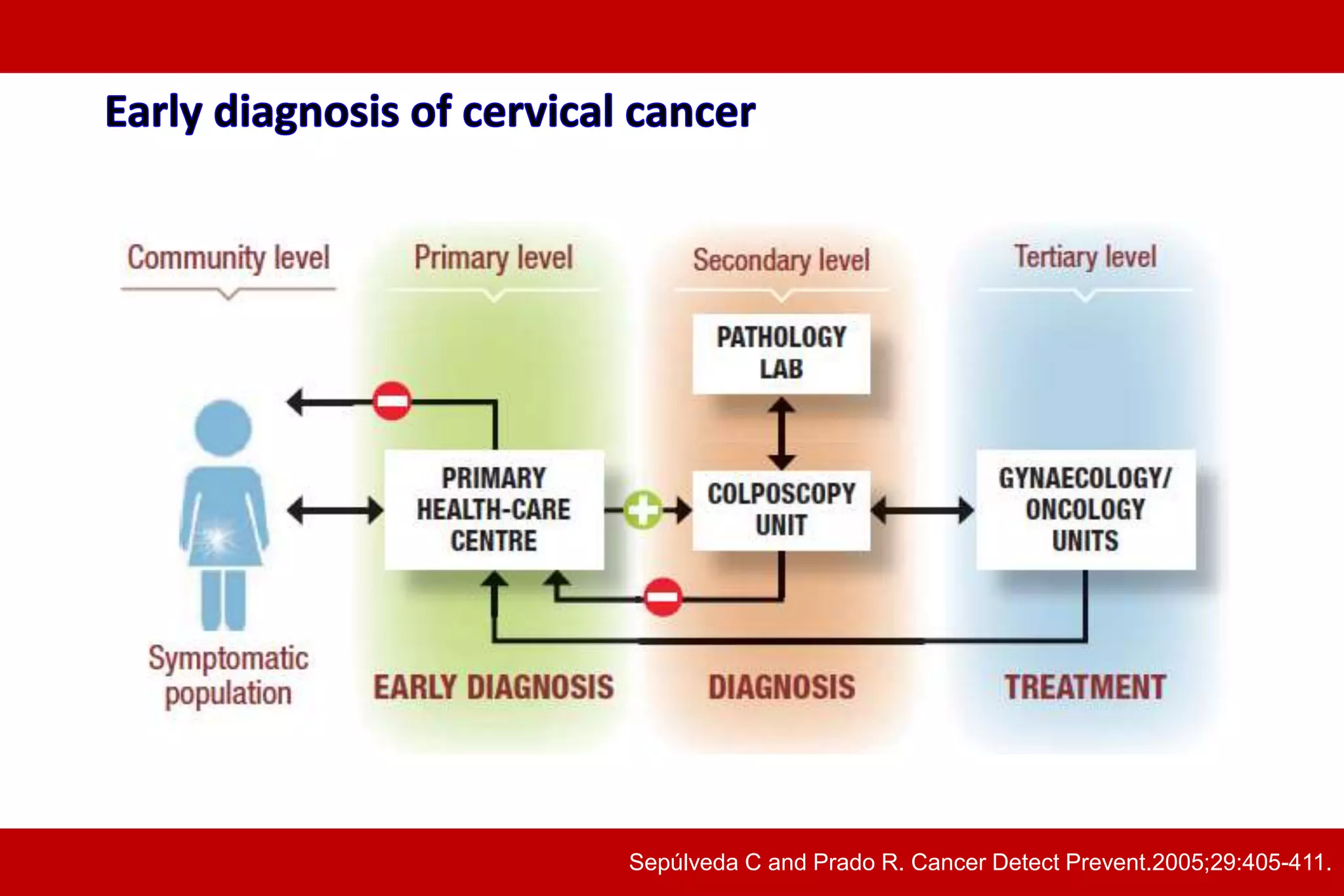
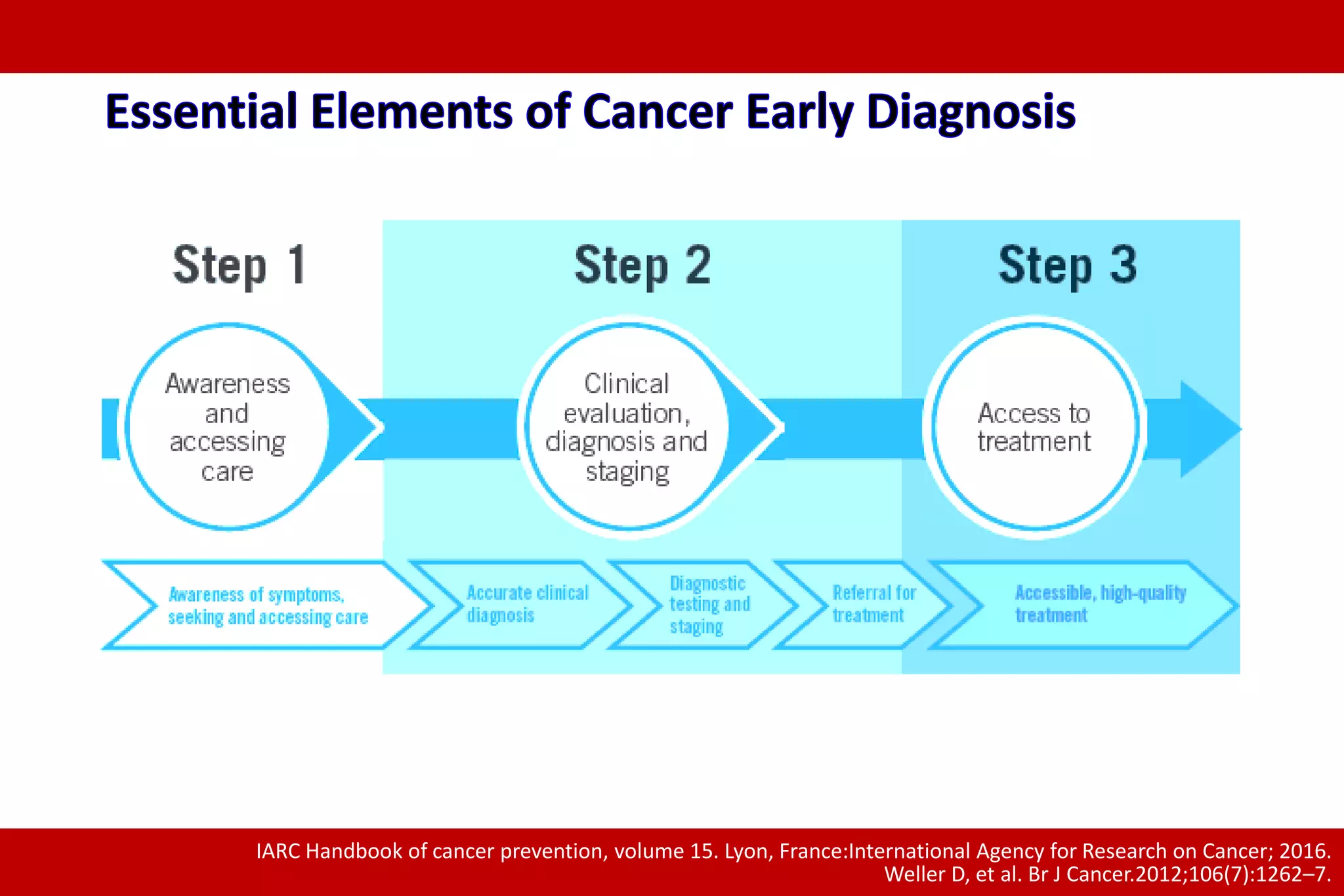
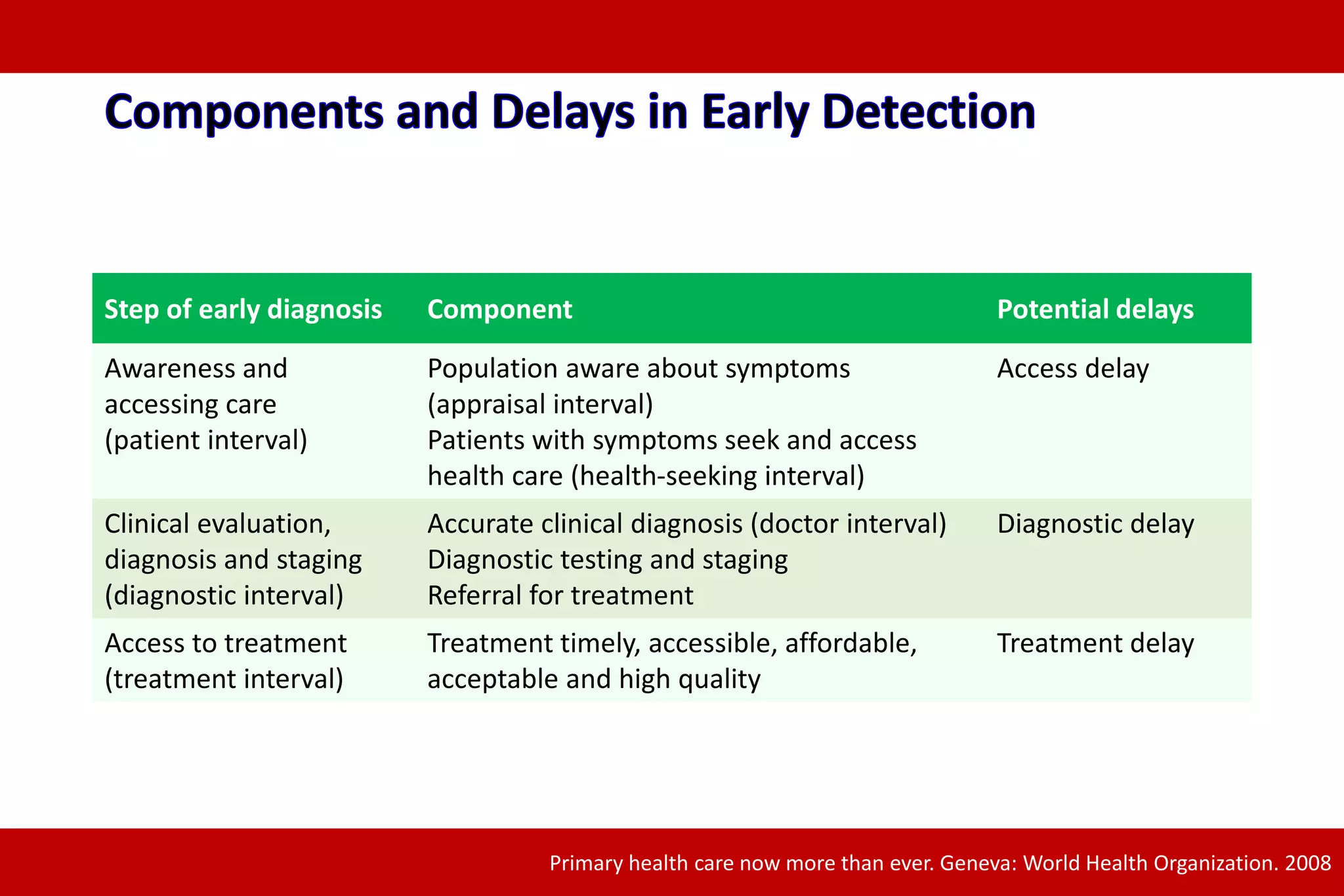
1. Early detection of cancer is important for effective treatment and reducing cancer deaths. When cancer is detected earlier, treatment works better and is less complex.
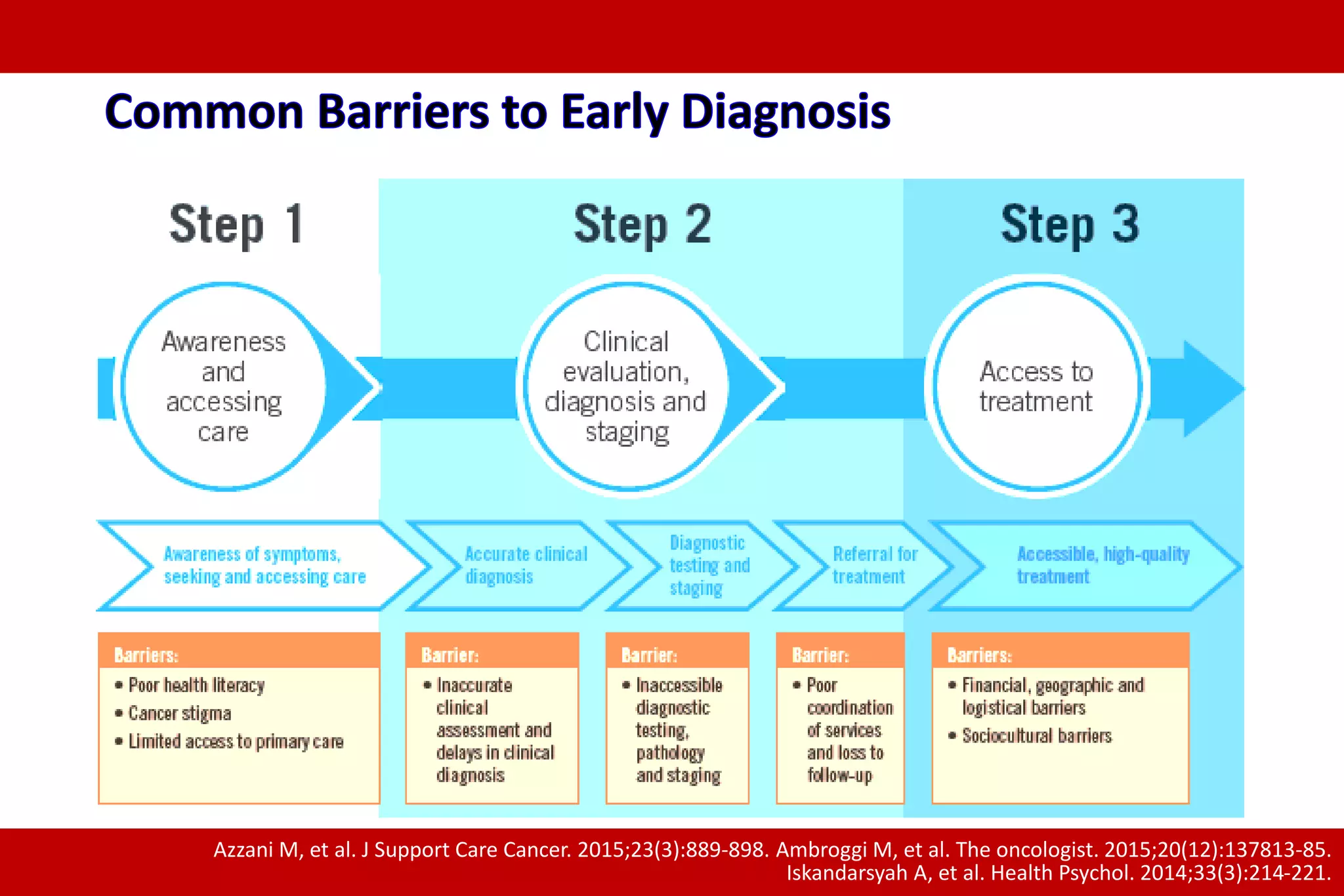
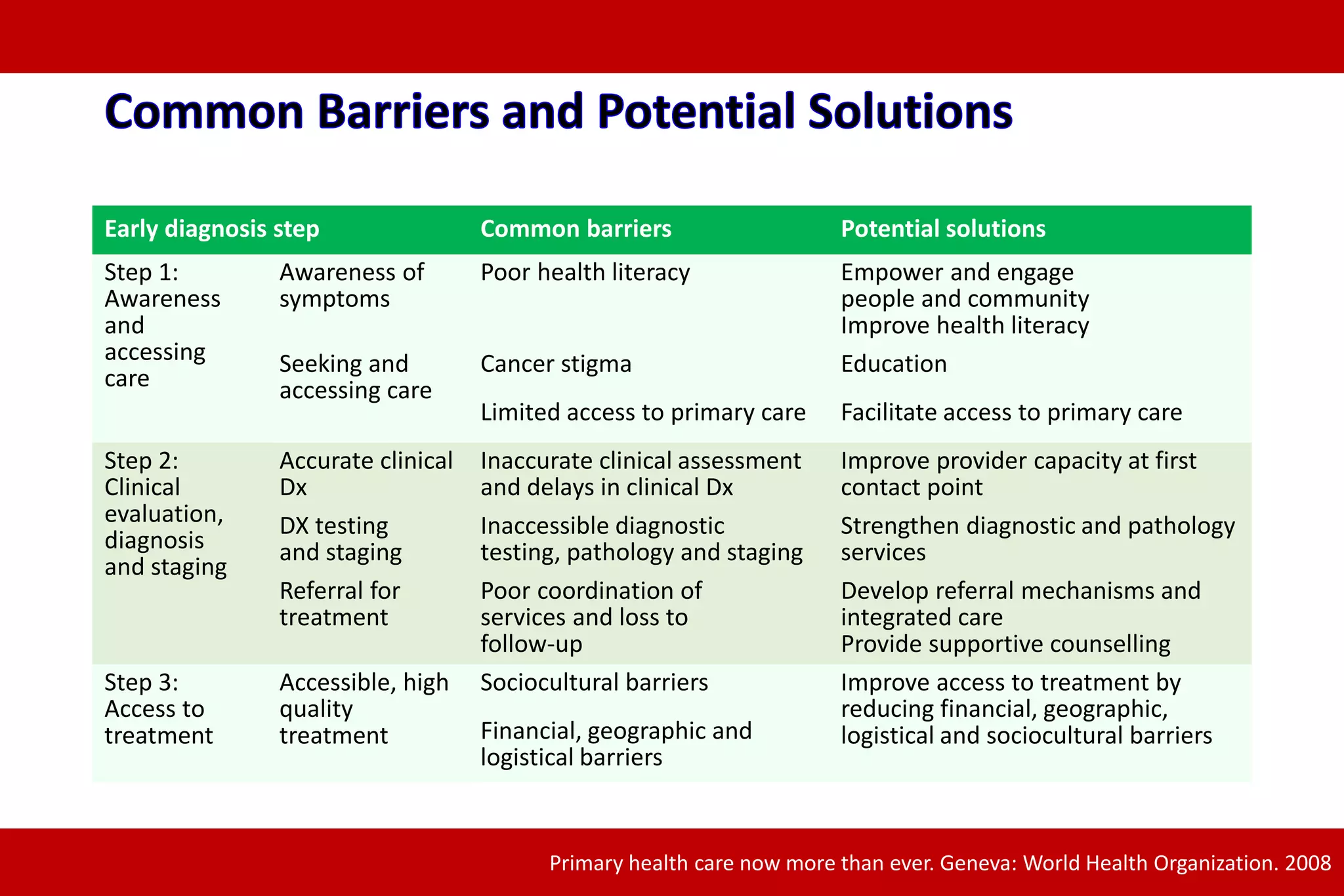
2. There are barriers to early detection like lack of awareness, access to care, and follow up. Building capacity for early diagnosis through education, accessible services, and coordinated care can help address these barriers.
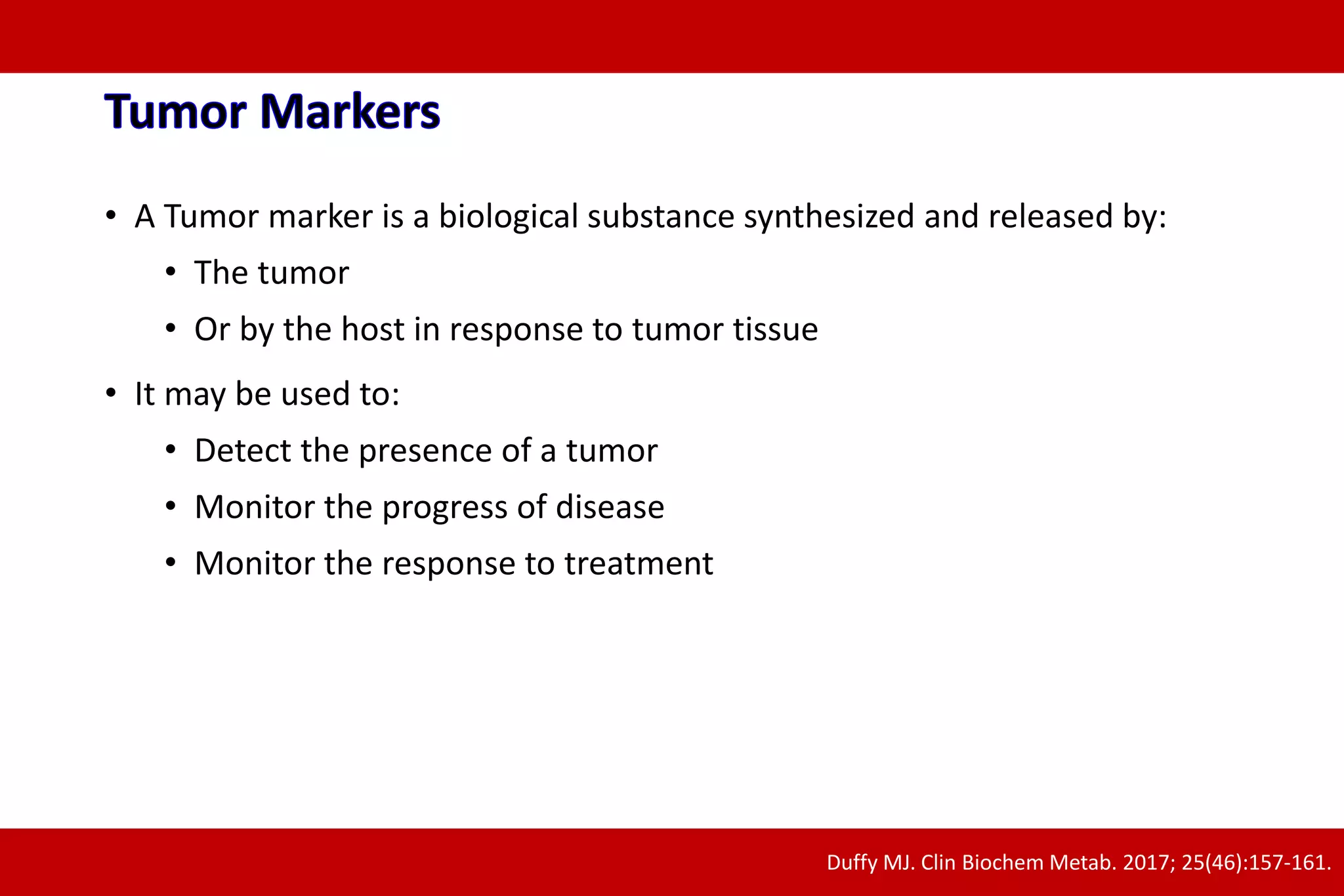
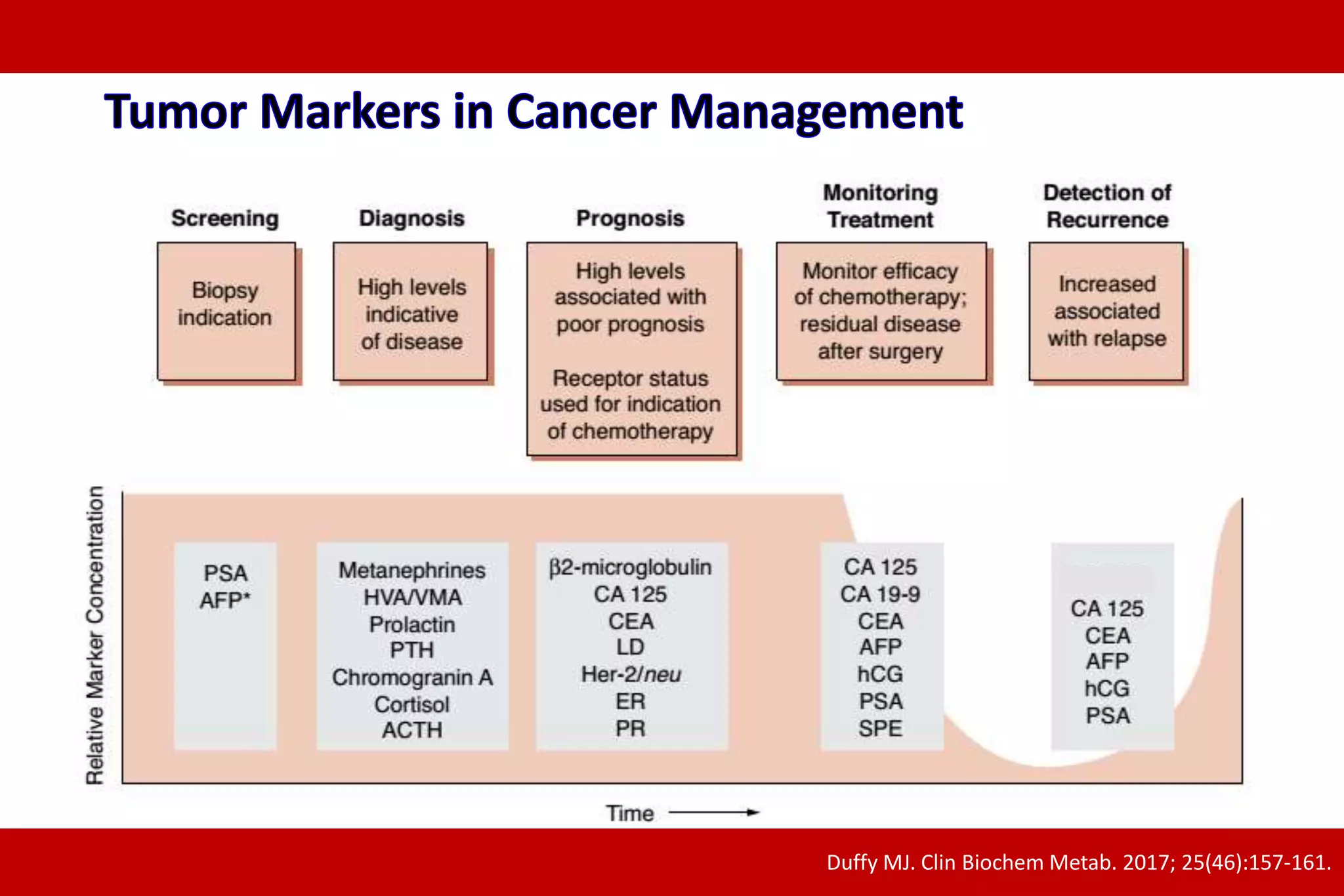
3. A strategic, integrated approach is needed to strengthen early diagnosis including improving primary care evaluation and diagnostic testing, as well as ensuring timely access to treatment.