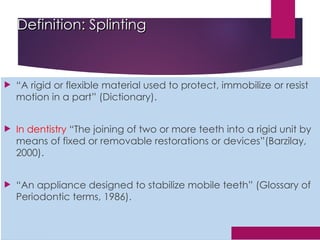
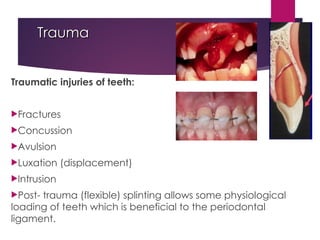
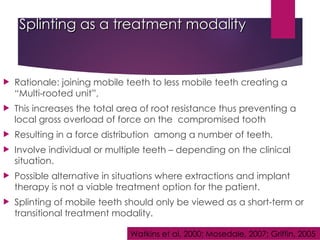
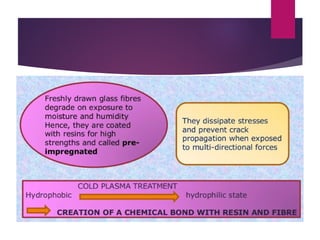
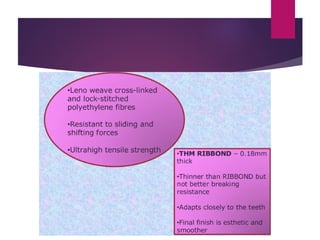
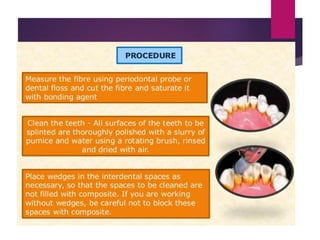
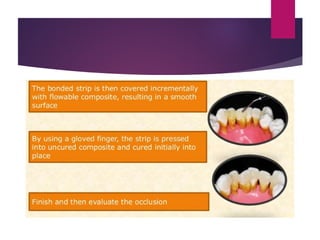
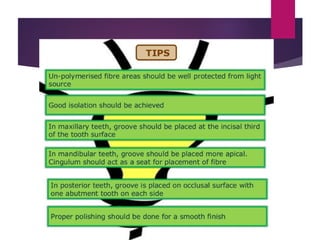
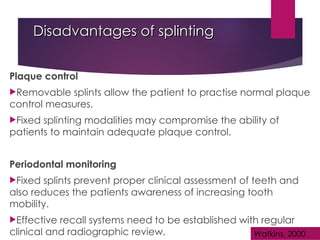
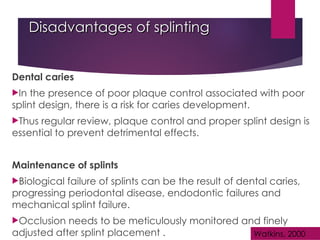
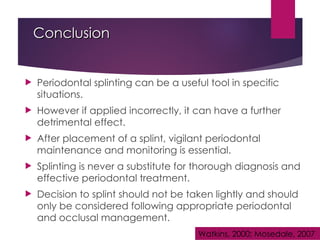
The document discusses periodontal splinting as a dental treatment technique used for stabilizing mobile teeth through the joining of two or more teeth. It outlines various applications, principles, indications, contraindications, classifications, and advantages and disadvantages of splinting, emphasizing its role in maintaining oral health. While it can be beneficial in specific situations, the document warns that improper use can lead to detrimental effects, necessitating thorough diagnosis and careful monitoring.