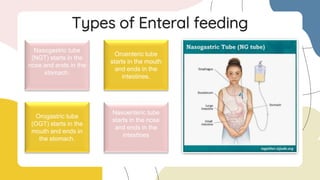
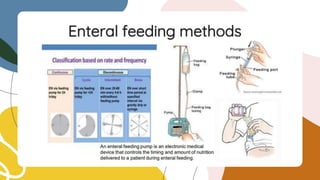
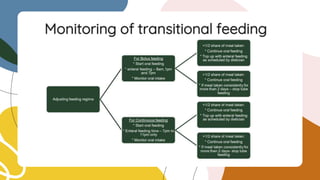
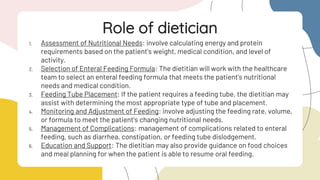
Nutritional support provides nourishment to patients who cannot eat normally. It involves either enteral or parenteral feeding. Enteral feeding delivers nutrients through the gastrointestinal tract using tubes, while parenteral feeding delivers nutrients intravenously. Transitional feeding involves gradually transitioning patients from parenteral to enteral feeding as their gastrointestinal function returns. Dietitians play an important role in assessing patients' nutritional needs, selecting appropriate formulas, educating patients, and managing complications during all stages of nutritional support.