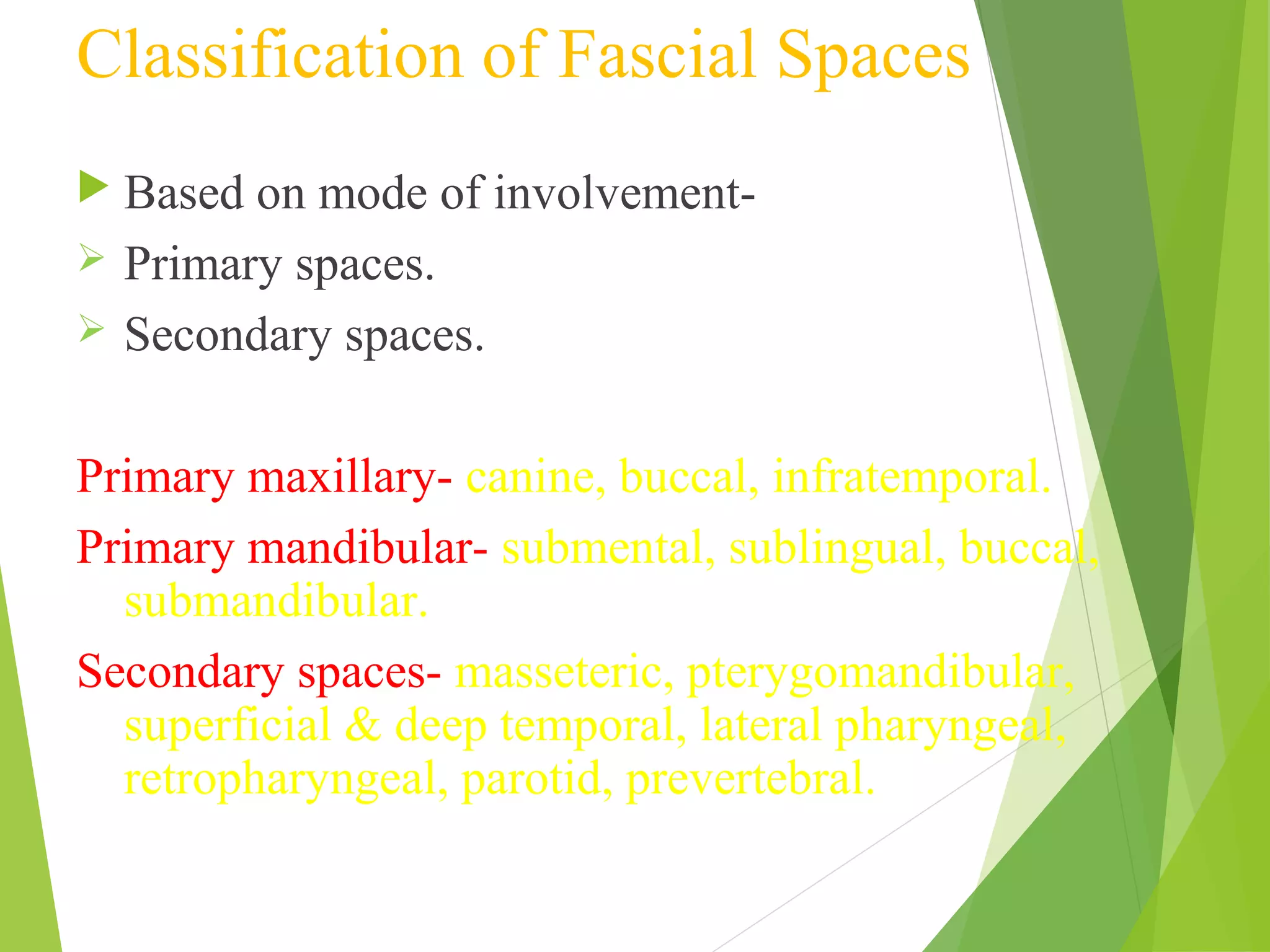
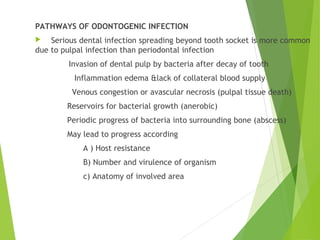
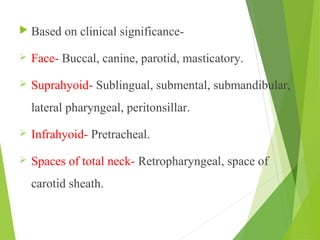
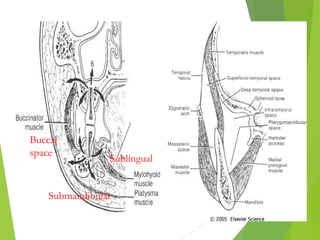
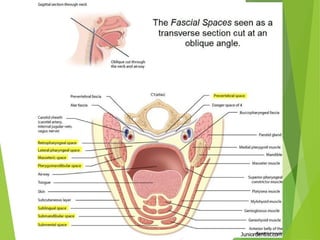
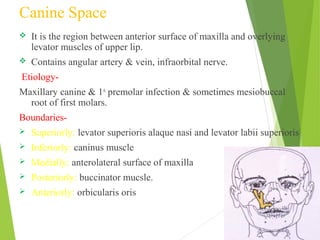
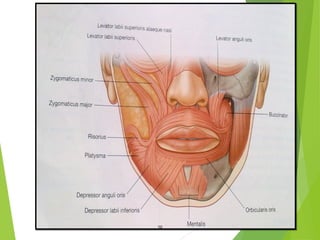
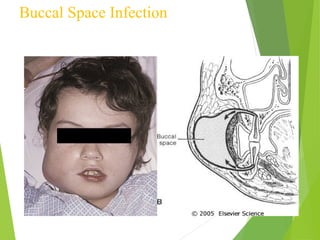
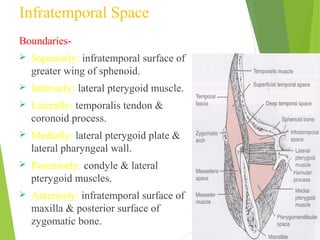
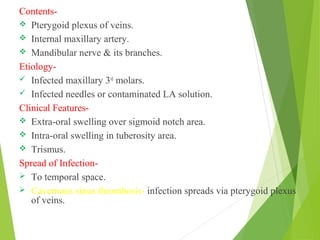
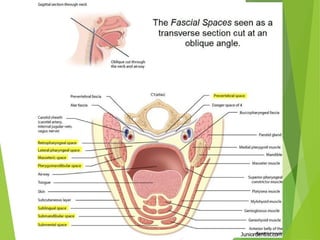
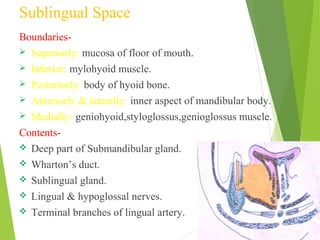
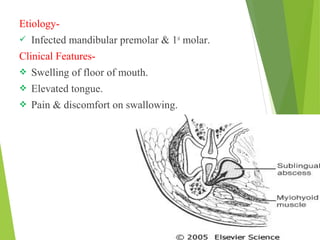
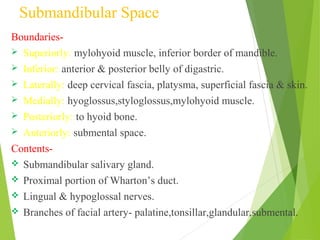
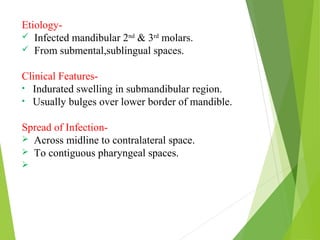
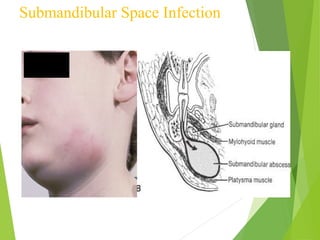
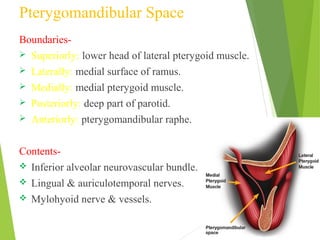
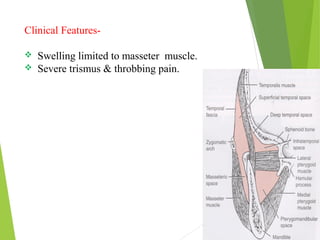
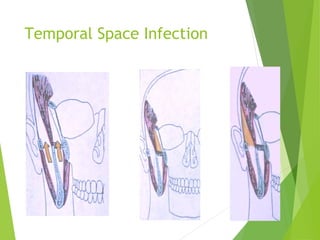
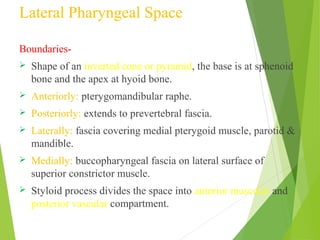
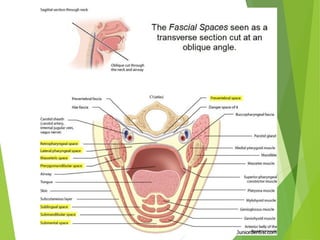
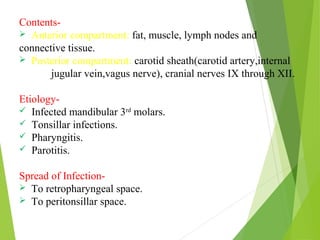
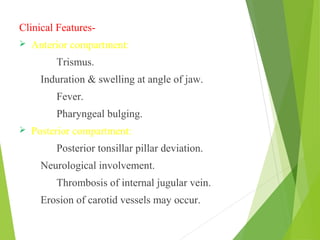
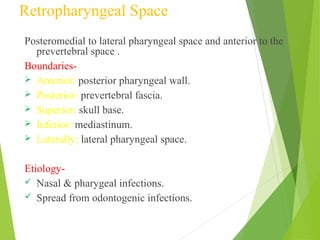
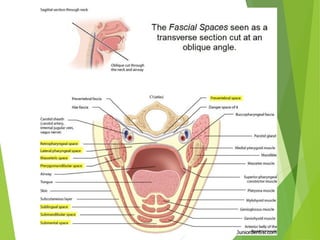
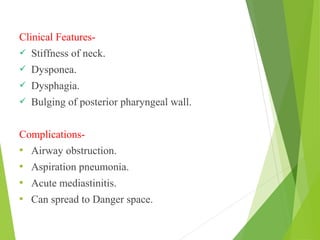
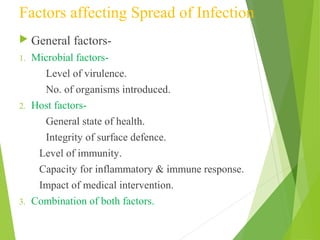
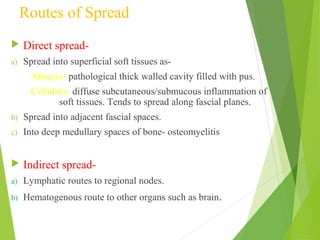
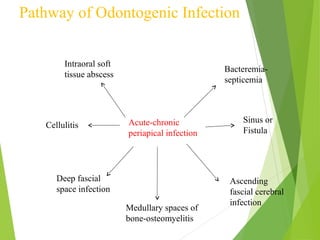
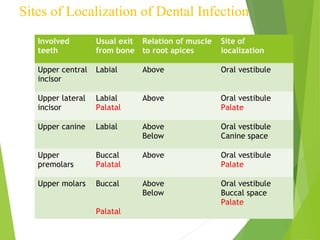
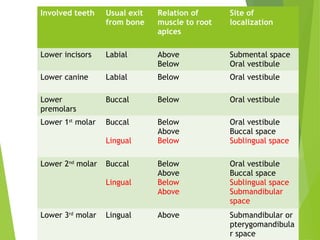
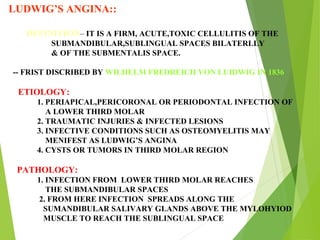
This document discusses the classification and pathways of spread of odontogenic infections. It begins by classifying fascial spaces as primary or secondary, and by clinical significance. Key primary spaces include the maxillary (canine, buccal, infratemporal) and mandibular (submental, sublingual, buccal, submandibular). Secondary spaces include the masseteric, pterygomandibular, temporal, and pharyngeal spaces. Odontogenic infections most commonly spread from the infected tooth to surrounding soft tissues and fascial spaces. The document then discusses specific spaces like the buccal, submandibular, and lateral pharyngeal spaces. Microbiology, clinical