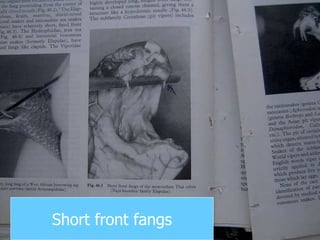
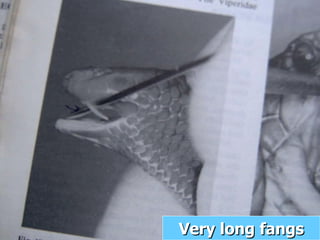
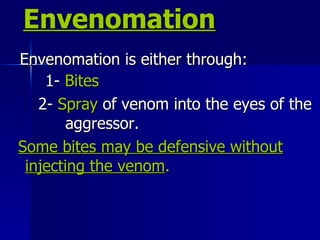
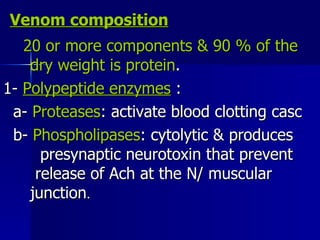
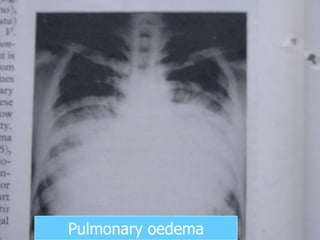
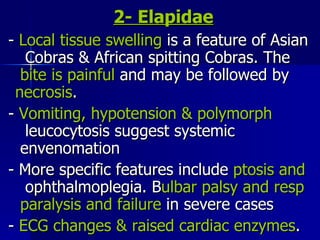
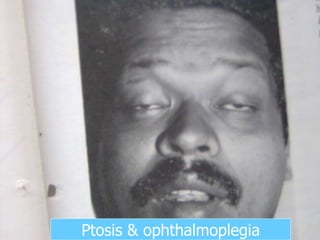
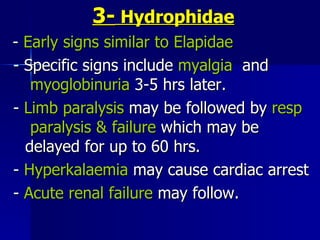
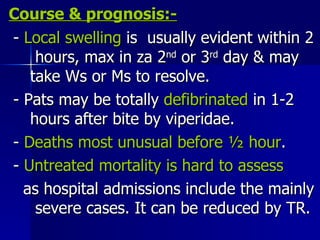
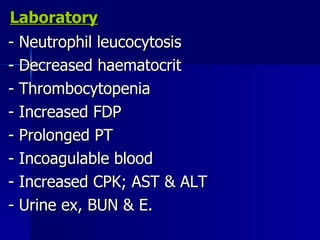
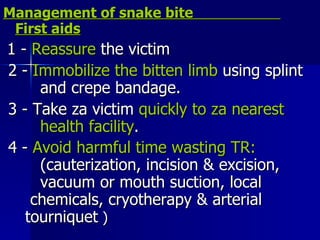
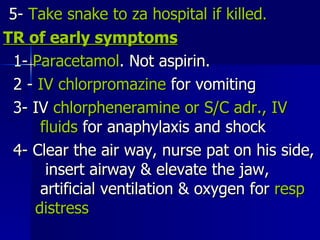
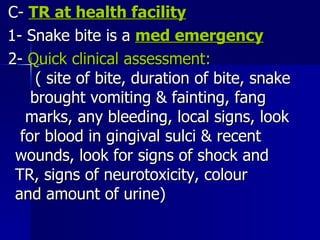
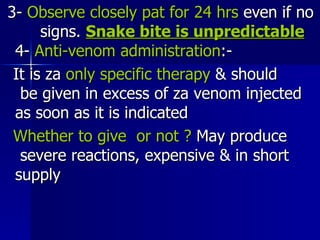
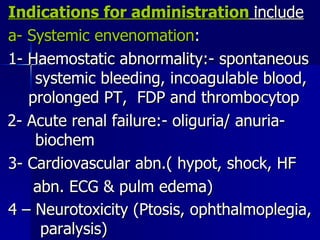
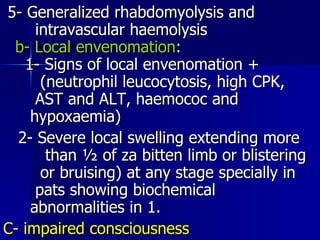
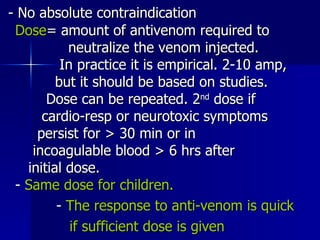
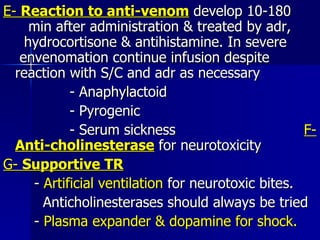
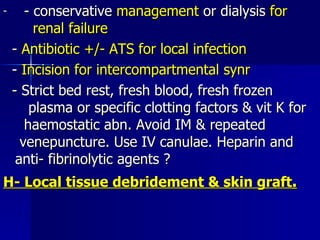
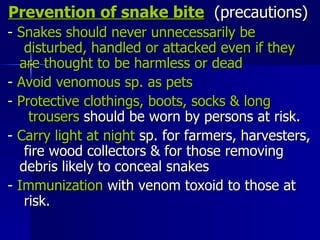
The document summarizes key information about snake bites, including that they are a major public health problem causing morbidity and mortality in tropical regions. It describes the three main venomous snake families and the types of toxins they contain. The clinical effects of envenomation are explained for each family, including local tissue damage as well as systemic effects like bleeding, shock, and paralysis. Diagnosis and management of snake bites are also outlined, emphasizing rapid treatment with antivenom as the only specific therapy.