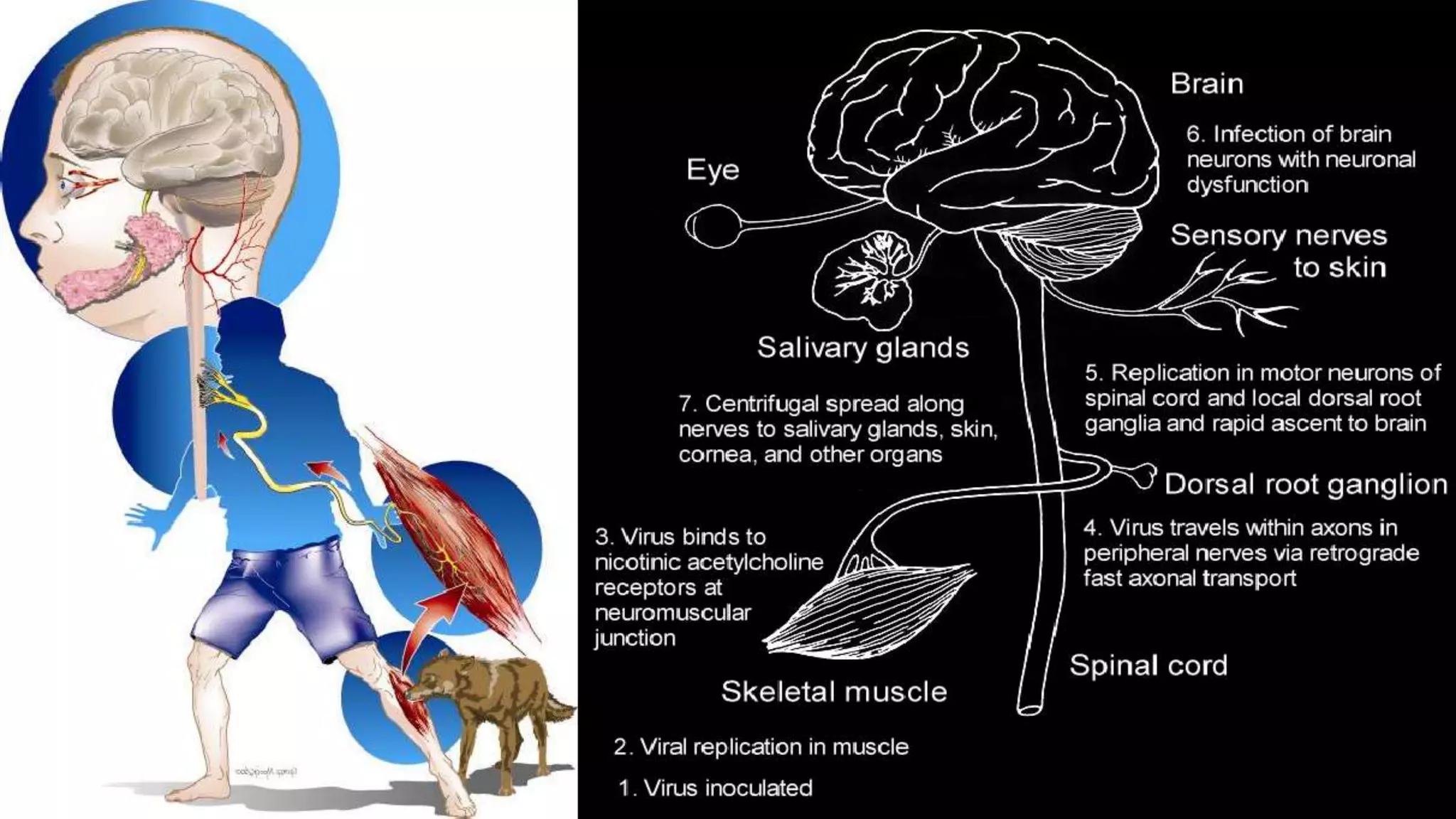
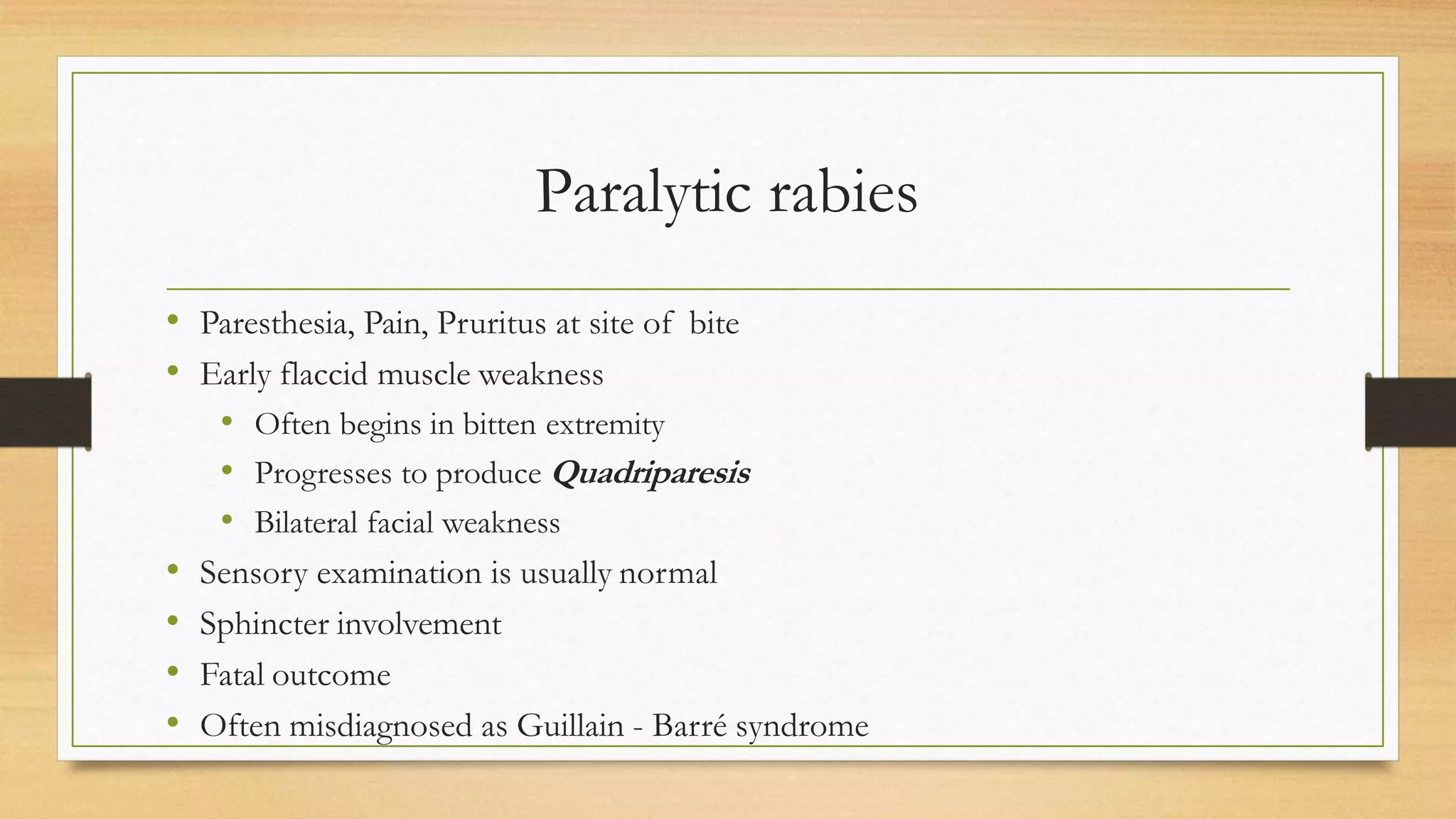
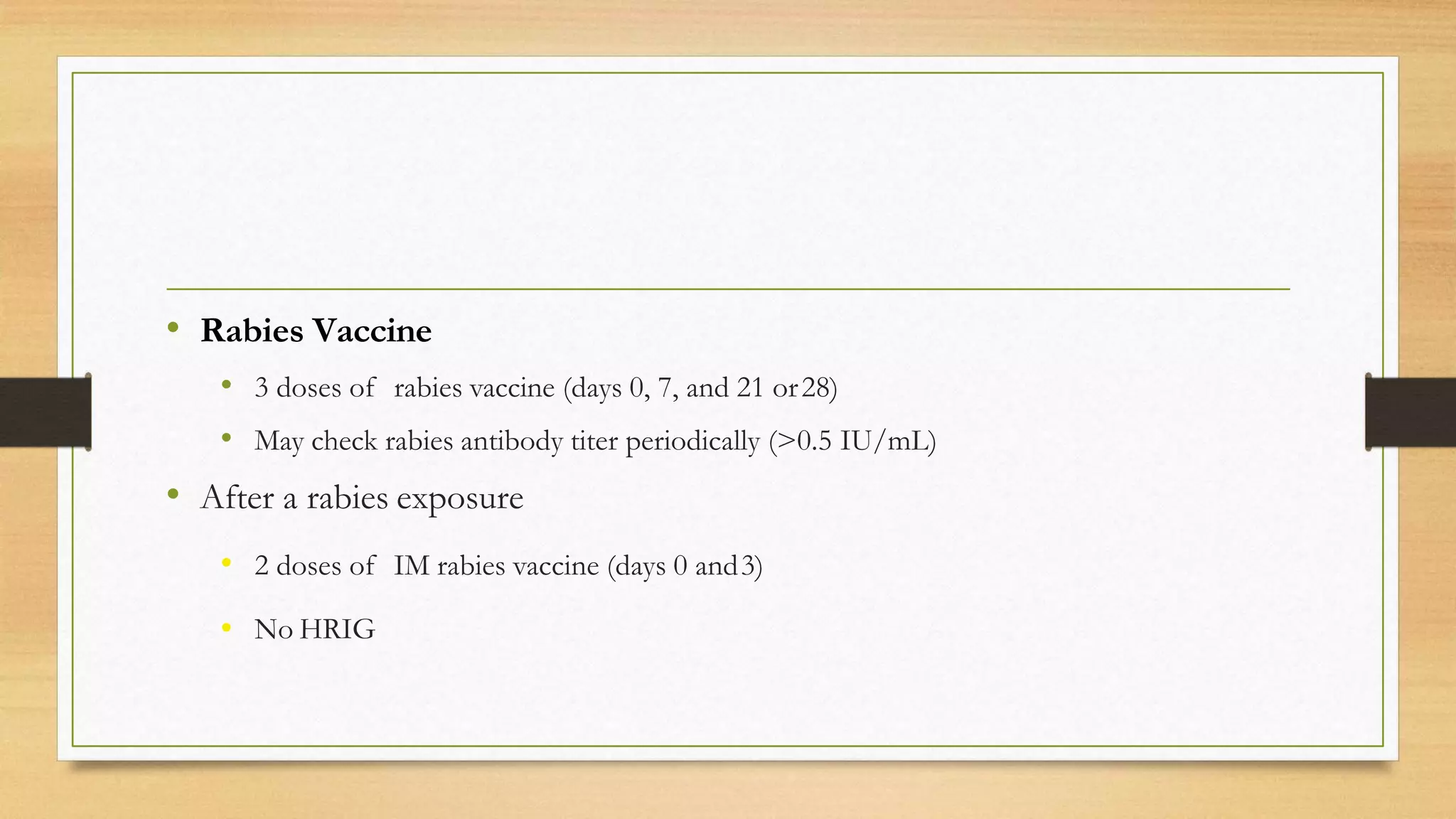
Rabies is a fatal zoonotic viral disease primarily affecting the nervous system and transmitted through bites or exposure to infected saliva. The document discusses the epidemiology, clinical manifestation, and prevention strategies for rabies, highlighting its prevalence in Asia and Africa. It emphasizes the importance of vaccination and immediate wound management for unvaccinated individuals post-exposure.