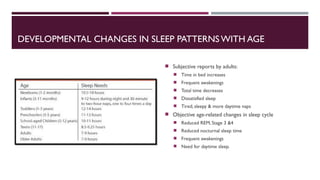
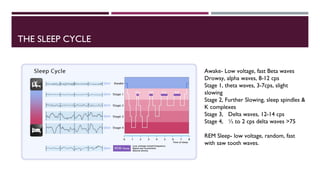
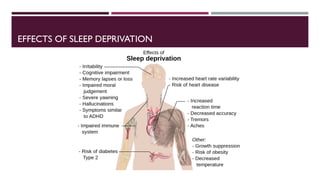
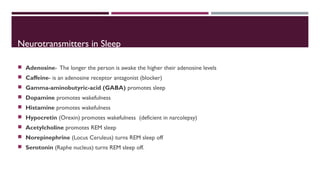
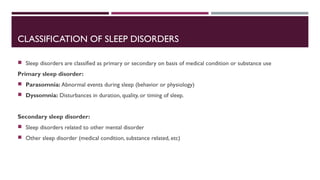
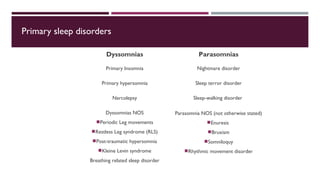
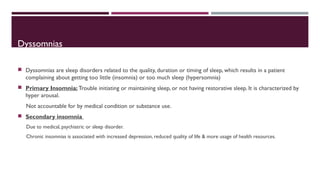
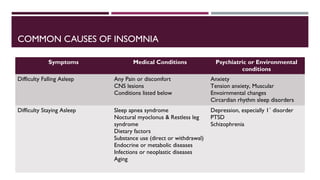
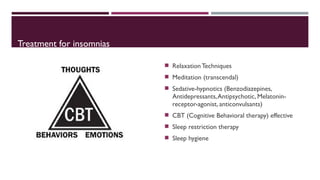
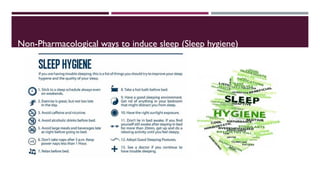
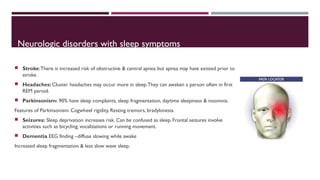
This document summarizes various sleep disorders and the normal sleep cycle. It discusses why sleep is needed, the stages of sleep including REM and NREM sleep, common sleep disorders like insomnia and sleep apnea, and factors that can influence sleep such as medical, psychiatric and environmental conditions. Treatment options are provided for various sleep disorders including lifestyle changes, medications, and therapies.