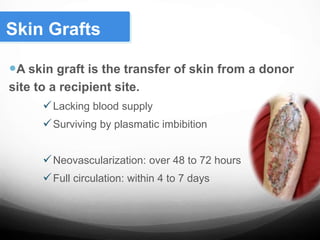
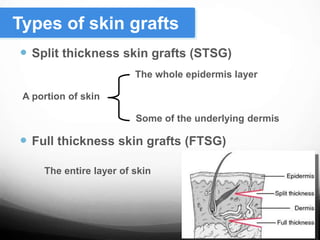
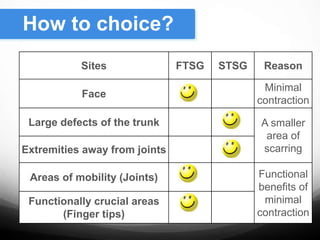
Skin grafting involves harvesting skin from a donor site and transferring it to a recipient site lacking adequate skin coverage. There are two main types of skin grafts - split thickness skin grafts (STSG) which transfer some of the epidermis and dermis, and full thickness skin grafts (FTSG) which transfer the entire skin layer. The recipient site must be properly prepared and grafted dermis side down. Grafts are secured and cared for until neovascularization occurs within 4-7 days. Factors like infection, poor wound healing, or graft movement can lead to graft failure. Skin grafting is commonly used to treat burns, wounds, and skin defects from trauma or cancer.