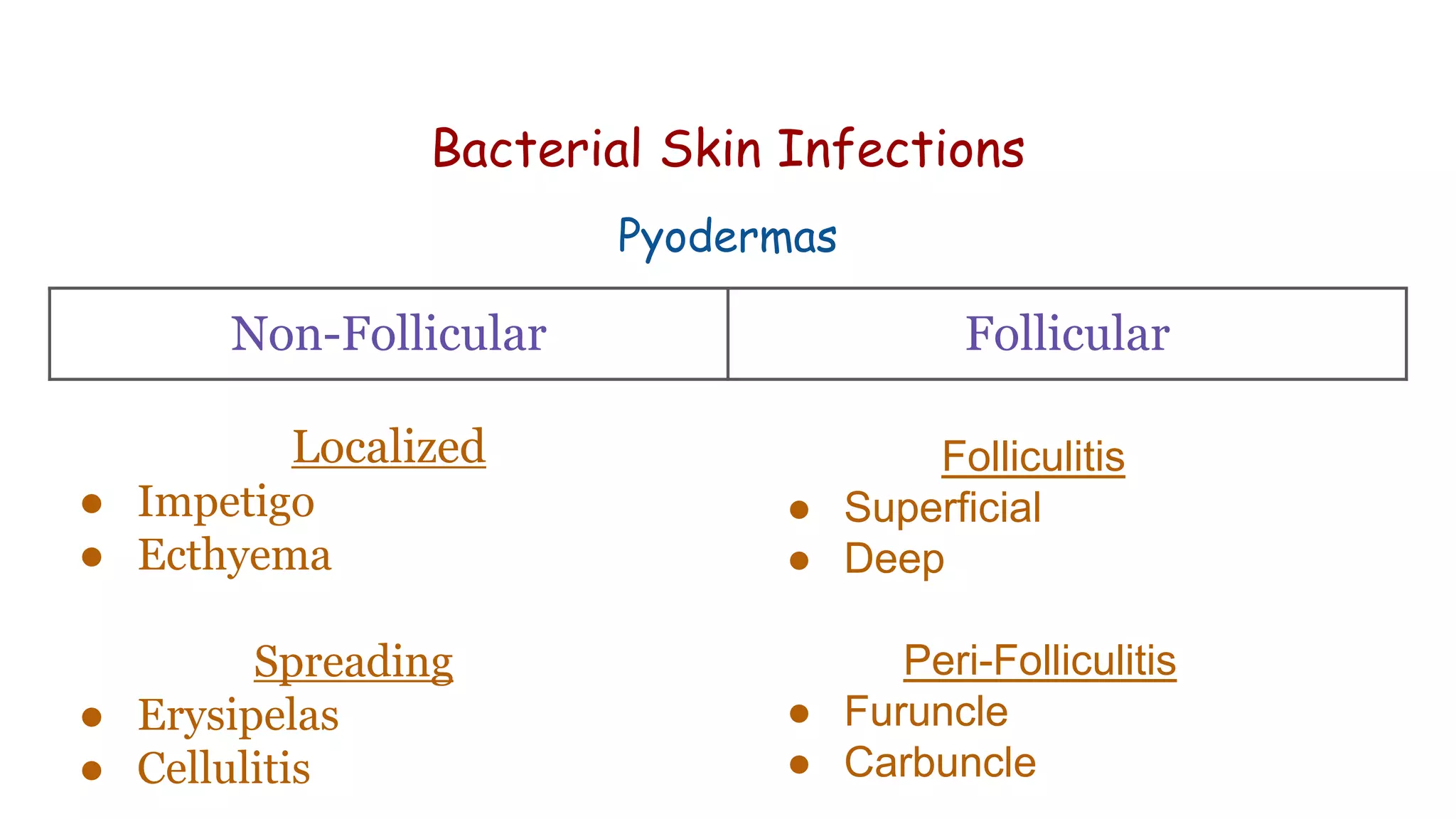
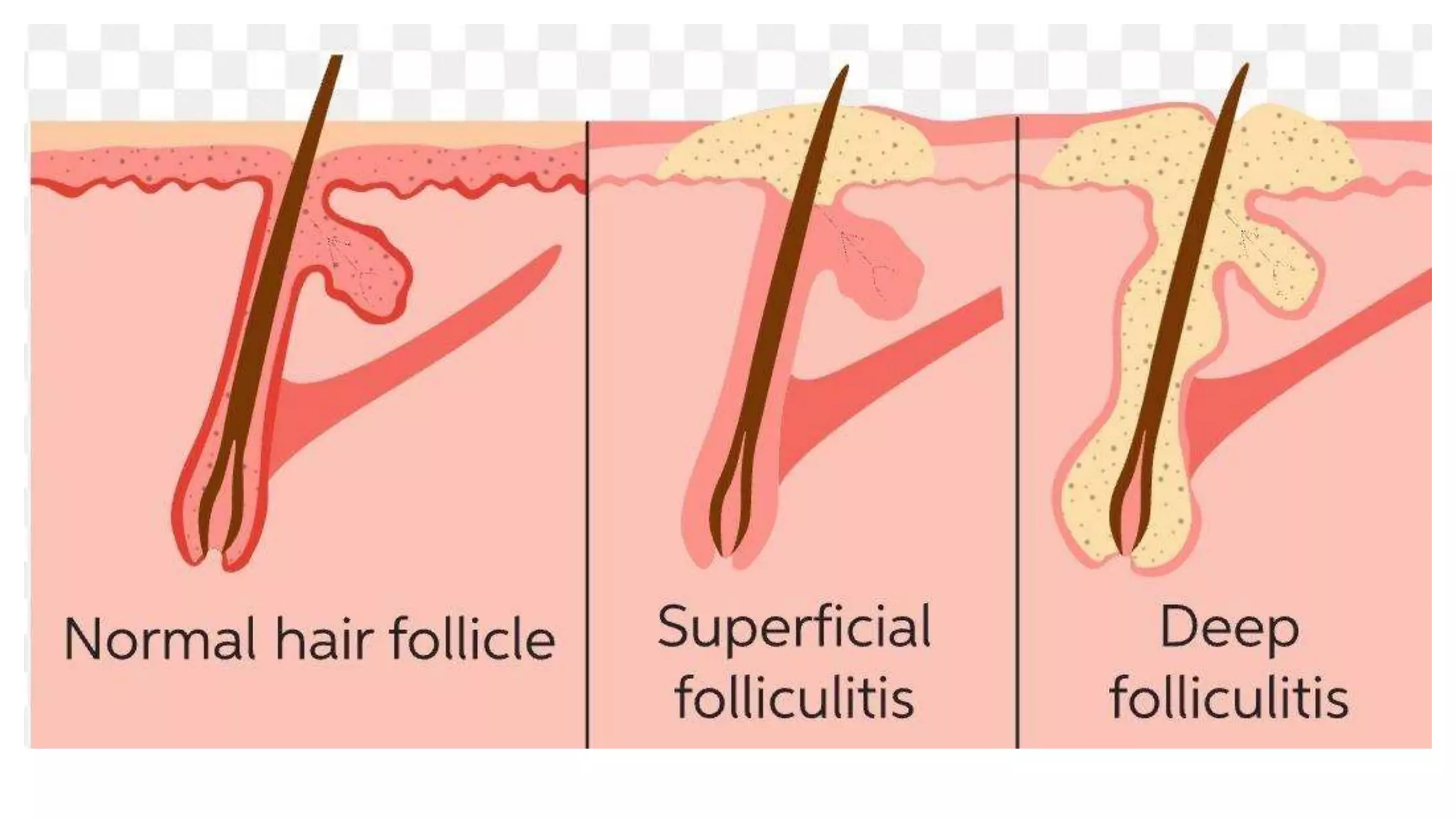
Bacterial skin disorders can be caused by resident or pathogenic bacteria on the skin. Common bacterial skin infections include impetigo, bullous impetigo, ecthyma, folliculitis, furuncles, carbuncles, erysipelas, and cellulitis. Impetigo is usually caused by Staphylococcus aureus or Streptococcus pyogenes and presents as crusty sores that can spread. Bullous impetigo caused by S. aureus causes fluid-filled blisters in infants. Folliculitis is a bacterial infection of hair follicles that can be superficial or deep. Furuncles are painful, pus-filled bumps under the skin caused by infected hair follicles