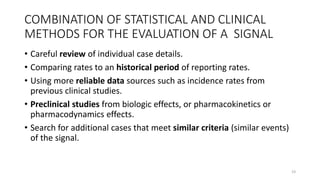
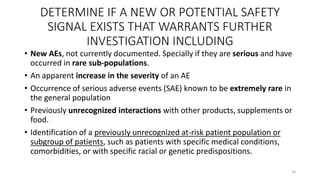
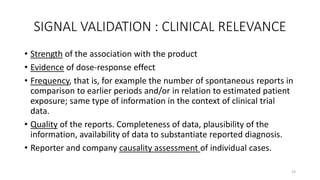
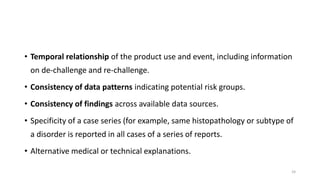
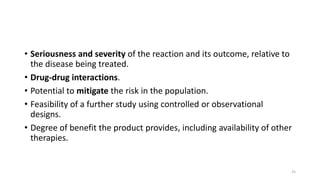
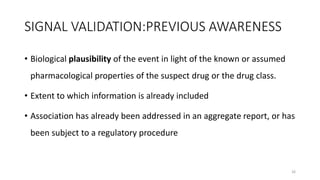
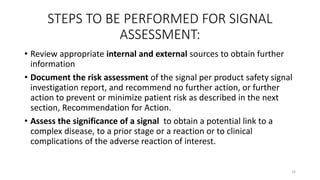
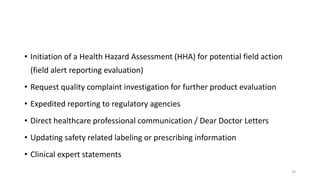
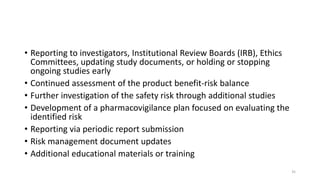
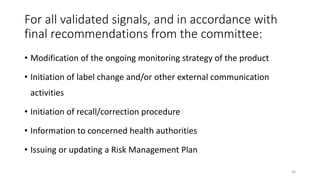
This document discusses signal detection and management in pharmacovigilance. It provides a brief history of pharmacovigilance programs internationally and in India. It defines pharmacovigilance and outlines the objectives, processes, and key steps involved in signal detection, validation, prioritization, assessment, and recommendation for action. These include ongoing monitoring of adverse event reports, signal detection methods, validation criteria, prioritization factors, signal assessment, and potential recommendations that may involve regulatory reporting, labeling changes, or additional studies. The goal is to identify potential safety issues and determine appropriate actions to prevent or minimize patient risk.