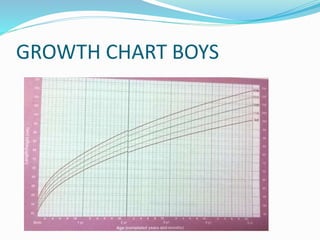
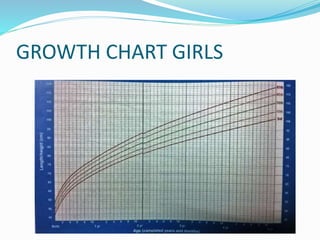
Mid-parental height is used to estimate a child's genetically determined height potential. It is calculated differently for boys and girls based on the average of the parents' heights. This value is plotted on a growth chart at age 18-20 to estimate the child's target height percentile. Evaluating short stature involves ruling out common causes through blood tests and imaging. If these are normal, tests are done to check for growth hormone deficiency, hypothyroidism, and Turner syndrome. Growth hormone therapy can increase final adult height by 20-30 cm for children with growth hormone deficiency.