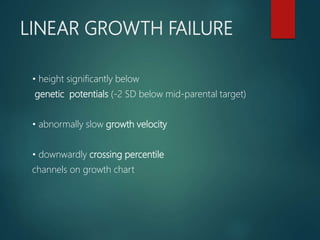
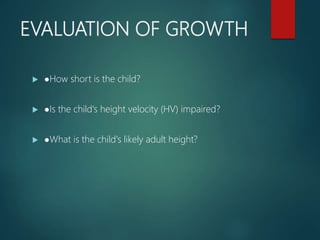
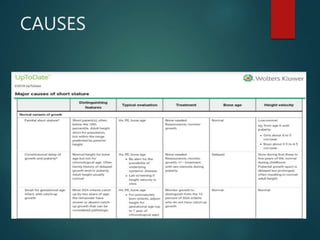
1) Short stature is defined as a height more than 2 standard deviations below the average for age and sex. A thorough evaluation considers the child's growth pattern, growth velocity, bone age, medical history, and family history.
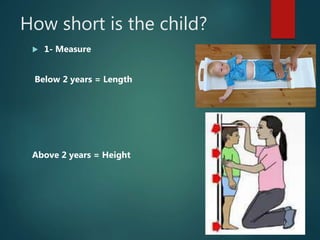
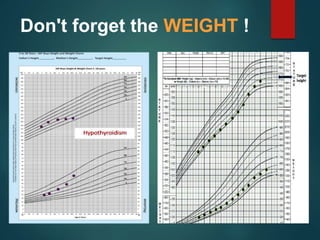
2) Basic evaluations include height, weight, bone age, and blood tests. Further testing may include thyroid function tests, serum IGF-1, karyotype, and morning LH/FSH if signs of precocious puberty are present.
3) Causes of short stature include genetic factors, malnutrition, endocrine disorders, chronic diseases, and idiopathic causes. Growth hormone therapy may be considered for growth hormone deficiency, Turner syndrome, and other conditions

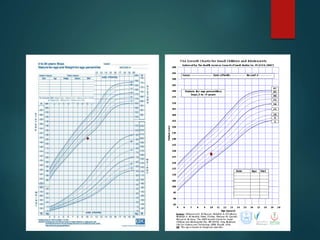
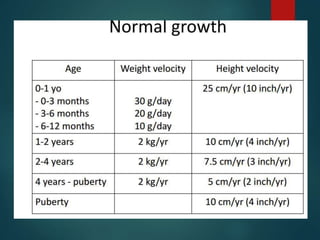
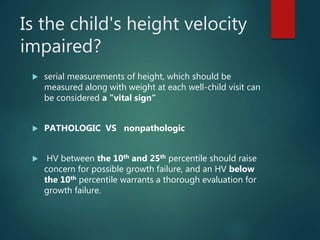
![NORMAL GROWTH
In general, a normal pattern of growth suggests good health.
Slow growth rate raises the possibility of an underlying pathological
cause of growth failure.
Statural growth is a continuous but not linear process.
There are three phases of postnatal growth (infantile, childhood, and
pubertal),
each of which has a distinctive pattern [5]. The phases are similar for
boys and girls, but the timing and pace of growth differ, particularly
during puberty.](https://image.slidesharecdn.com/shortstatureug210812-200113193602/85/Short-stature-a-Diagnostic-approach-4-320.jpg)
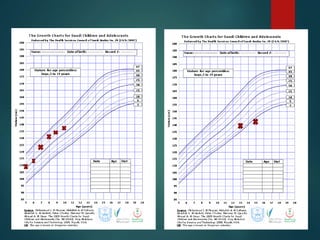


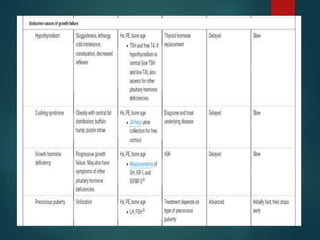
![Investigations
A basic evaluation : bone age determination is
appropriate for children with short stature, normal
growth rate and no other symptoms
Broader testing: severely short (eg, height ≤-2.5
standard deviations [SD, 0.6th percentile]), has growth
failure](https://image.slidesharecdn.com/shortstatureug210812-200113193602/85/Short-stature-a-Diagnostic-approach-23-320.jpg)
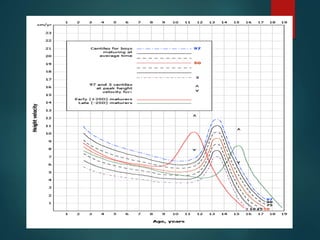
![ Celiac serologies (eg, tissue transglutaminase [tTG]
immunoglobulin A [IgA] and total IgA)
•Thyroid stimulating hormone (TSH), free thyroxine (T4)
Karyotype (in all girls, to rule out Turner syndrome, and in
boys with associated genital abnormalities)
, insulin-like growth factor-I (IGF-I), and insulin-like
growth factor binding protein 3 (IGFBP-3). •Karyotype (in
all girls, to rule out Turner syndrome, and in boys with
associated genital abnormalities).
•Morning luteinizing hormone (LH) and follicle-
stimulating hormone (FSH) in children with signs of sexual
precocity](https://image.slidesharecdn.com/shortstatureug210812-200113193602/85/Short-stature-a-Diagnostic-approach-25-320.jpg)