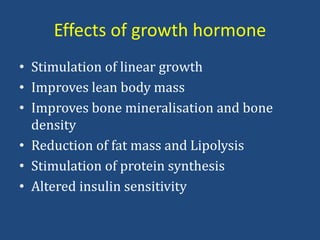
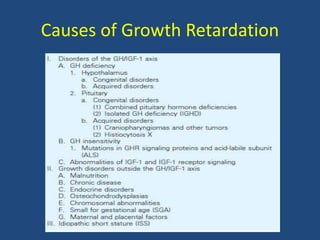
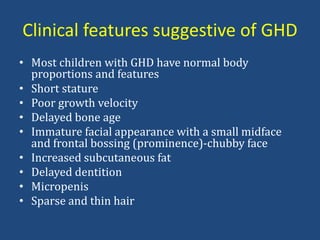
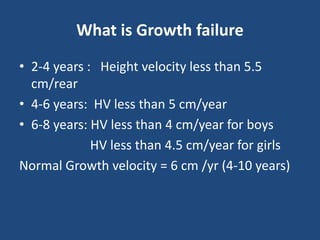
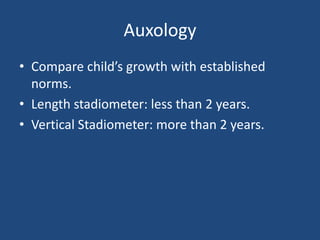
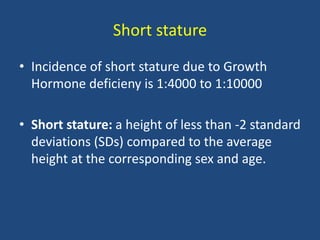
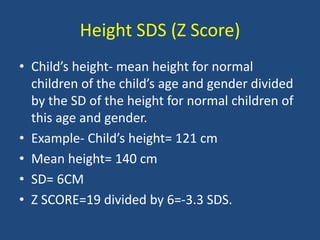
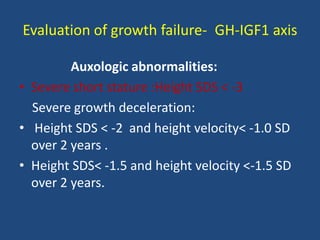
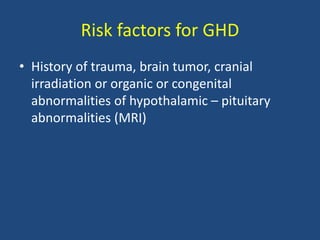
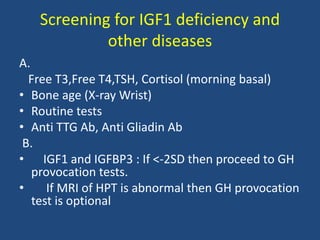
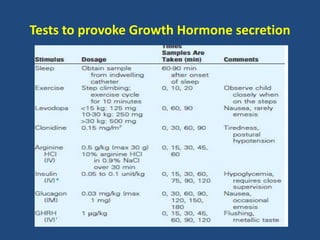
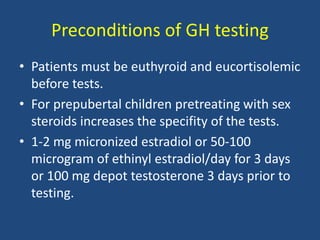
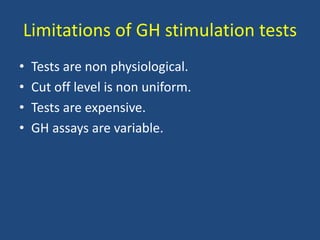
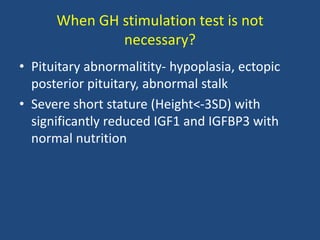
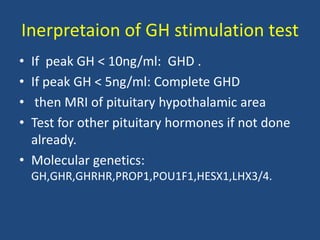
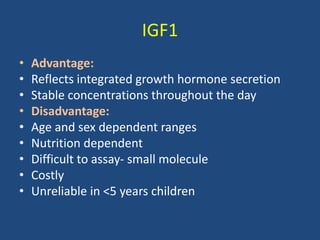
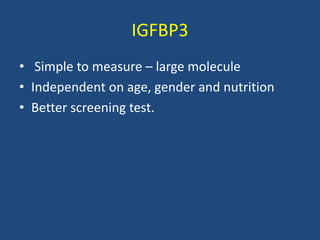
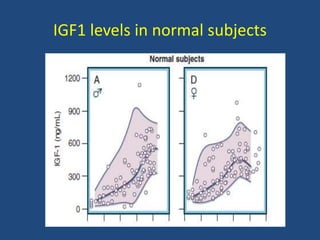
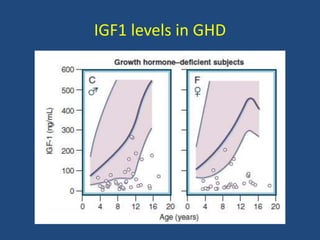
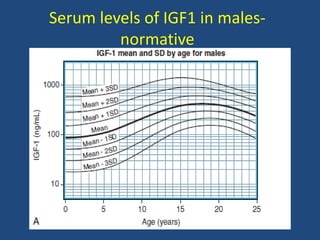
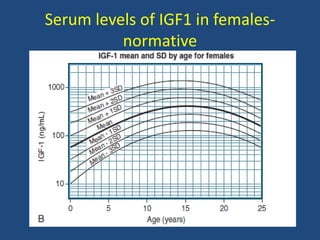
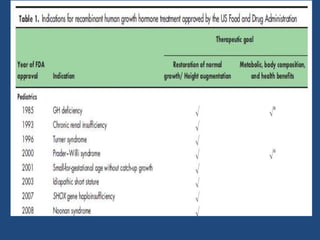
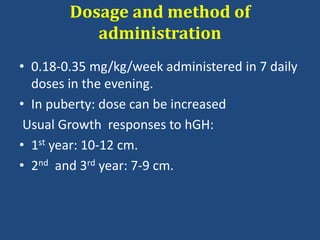
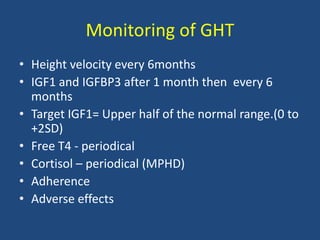
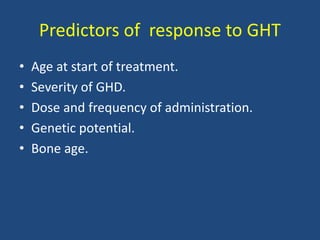
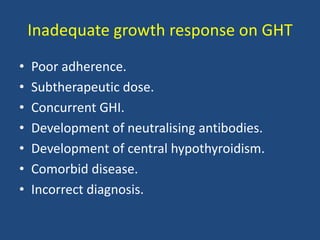
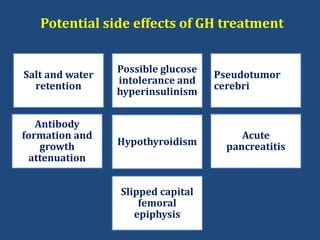
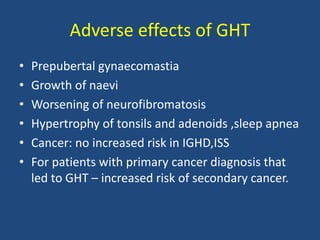
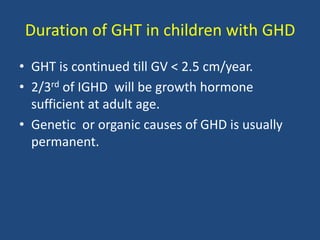
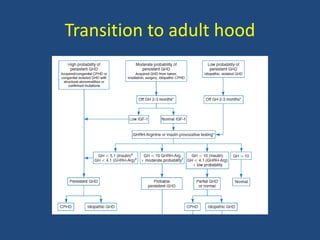
Growth hormone deficiency (GHD) is an important cause of short stature in children. Accurate diagnosis requires auxology, measurement of IGF1 and IGFBP3 levels, and GH stimulation tests. Recombinant human growth hormone therapy is effective and safe for treating GHD, but requires regular monitoring to ensure optimal results and growth responses.