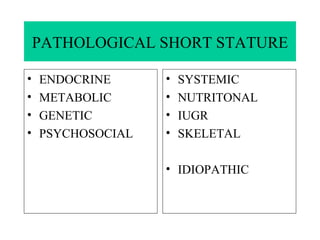
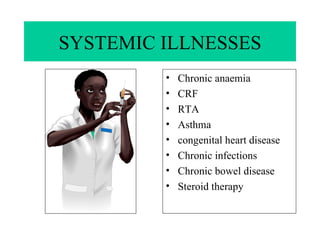
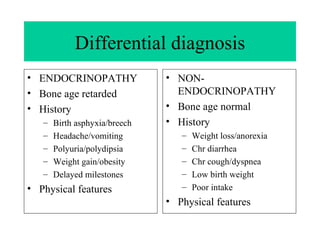
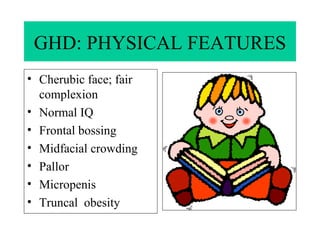
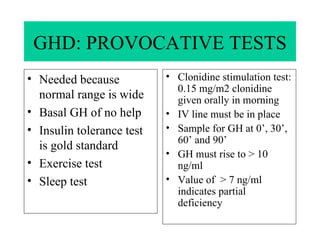
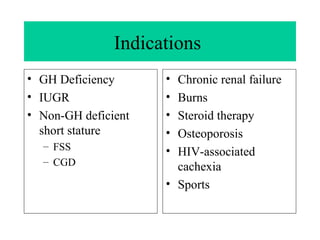
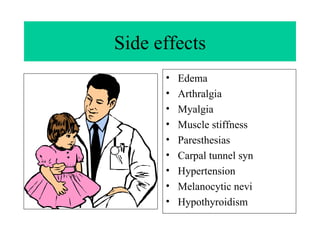
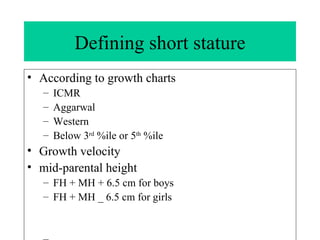
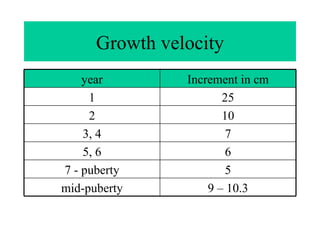
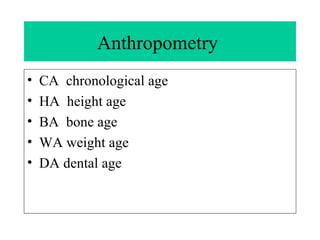
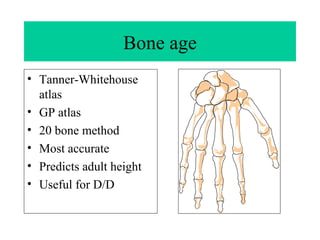
The document discusses various causes and types of short stature, including constitutional growth delay, familial short stature, and pathological short stature which can be due to endocrine, genetic, psychosocial, nutritional, or skeletal factors. Growth hormone deficiency is described as a potential endocrine cause, with details provided on growth hormone therapy and its administration. Differential diagnosis of endocrine versus non-endocrine causes of short stature is also covered.
![SHORT STATURE Dr SANJAY KALRA, D.M. [AIIMS]](https://image.slidesharecdn.com/cdocumentsandsettingslailaydesktopfrontpagegrowthinkidswithshortstature-100123022814-phpapp02/75/FTT-1-2048.jpg)
![Measuring stature Stadiometer Barefeet Four points touching the wall Frankfurt plane [line joining inferior orbital margin to ext auditory meatus] paralel to ground Serial measurements better](https://image.slidesharecdn.com/cdocumentsandsettingslailaydesktopfrontpagegrowthinkidswithshortstature-100123022814-phpapp02/85/FTT-6-320.jpg)
![Anthropometry US: LS ratio Arm span SE: EMC ratio Sitting height Supine length [if age< 2 years]](https://image.slidesharecdn.com/cdocumentsandsettingslailaydesktopfrontpagegrowthinkidswithshortstature-100123022814-phpapp02/85/FTT-7-320.jpg)
![Differential diagnosis Constitutional growth delay CGD Delayed puberty/ Late bloomer BL normal [upto 3 years] BA = HA < CA GV normal for BA AH normal](https://image.slidesharecdn.com/cdocumentsandsettingslailaydesktopfrontpagegrowthinkidswithshortstature-100123022814-phpapp02/85/FTT-12-320.jpg)