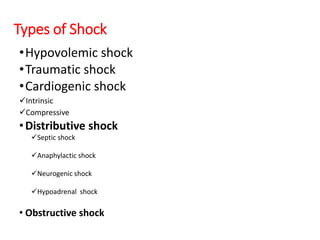
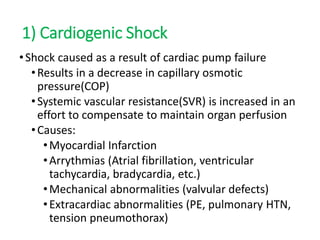
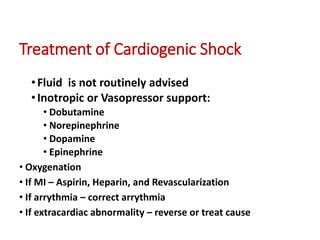
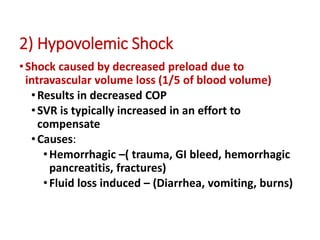
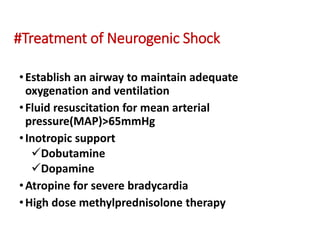
The document discusses shock, a physiological state marked by decreased systemic tissue perfusion leading to potential organ failure and death. It describes various types of shock, including cardiogenic, hypovolemic, and distributive shock, along with their causes, pathophysiology, and treatments. Effective management involves early identification, oxygen delivery, and addressing the underlying causes to improve survival outcomes.