The document discusses various topics related to hypospadias including:
1) The embryology of penile development and role of androgens and 5α-Reductase.
2) Diagnosis and classification of hypospadias and chordee.
3) Timing of hypospadias surgery, typically between 6-12 months.
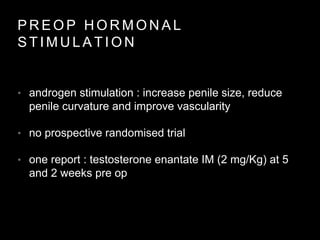
4) Preoperative hormonal stimulation to increase penile size for proximal cases.
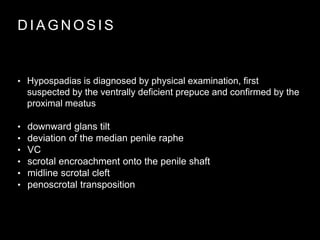
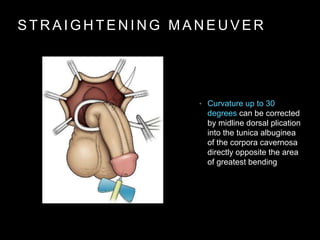
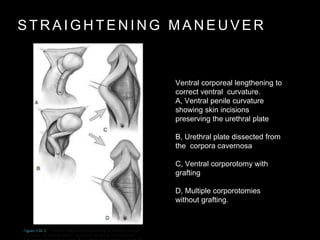
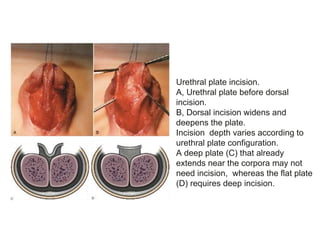
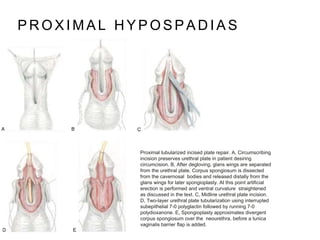
![A, Scrotal hypospadias with ventral curvature
B, Penis straightening included dissection of
the urethral plate and proximal urethra off the
corpora cavernosa
C, Despite elevation of the urethral plate from
the corpora, a dorsal midline incision for TIP
urethroplasty can still be performed without
creating separate strips
(Reprinted from Snodgrass W, Prieto J. Straightening ventral curvature while preserving
the urethral plate in proximal hypospadias repair. J Urol 2009;182[Suppl. 4]:1720–5.)
Mobilization of urethral plate and proximal urethra](https://image.slidesharecdn.com/hypospadias-160701112412/85/Hypospadias-17-320.jpg)