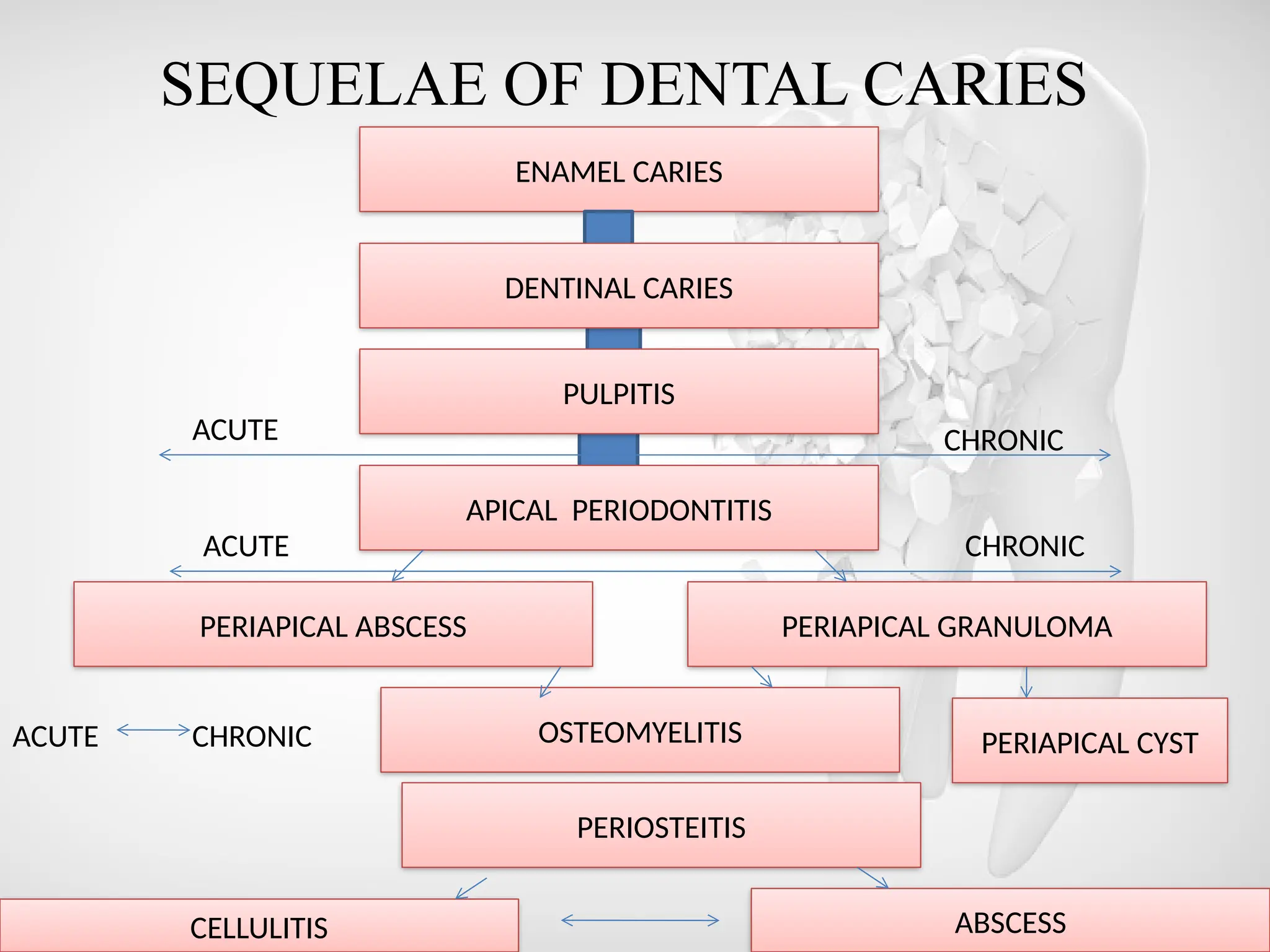
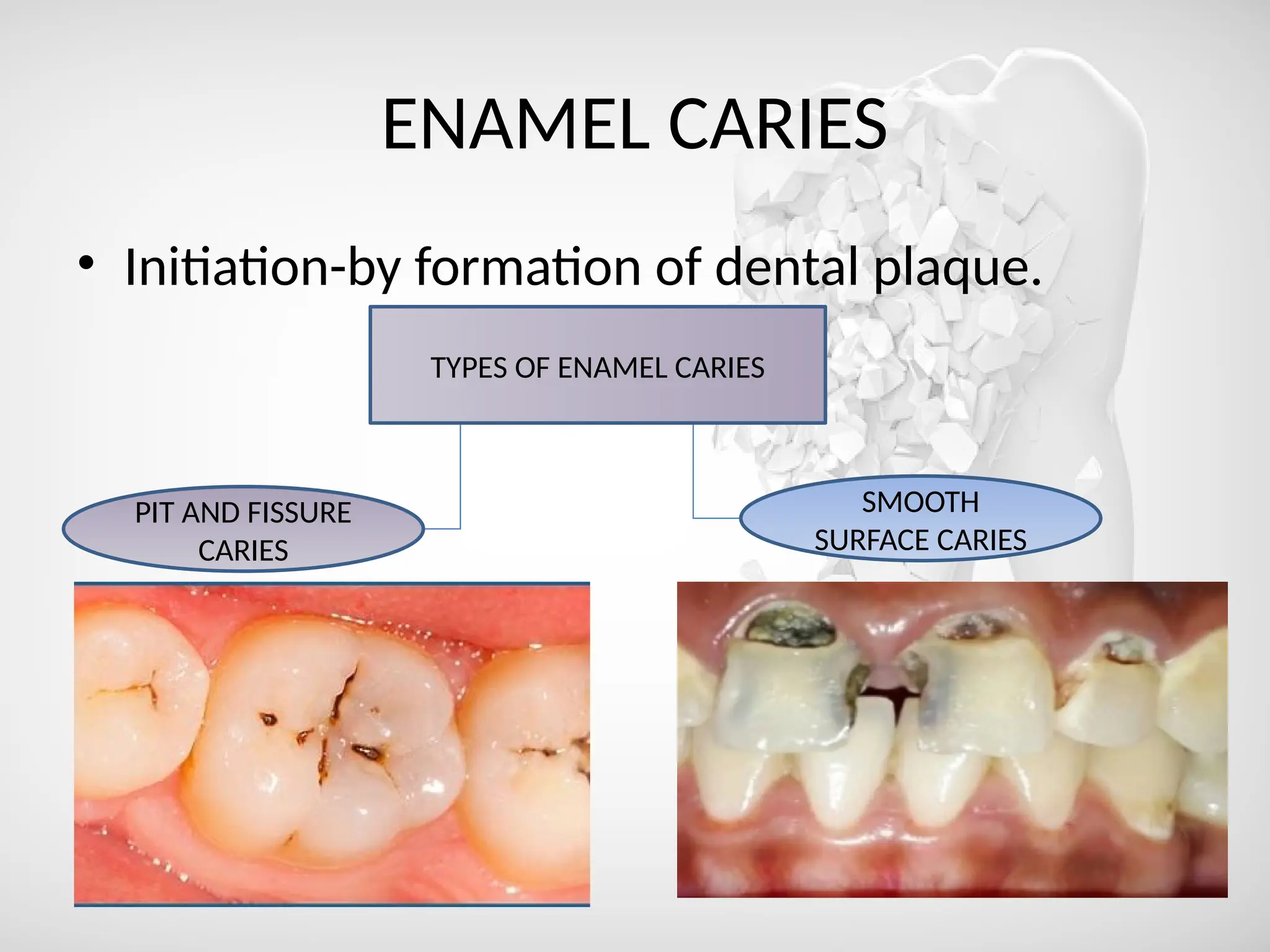
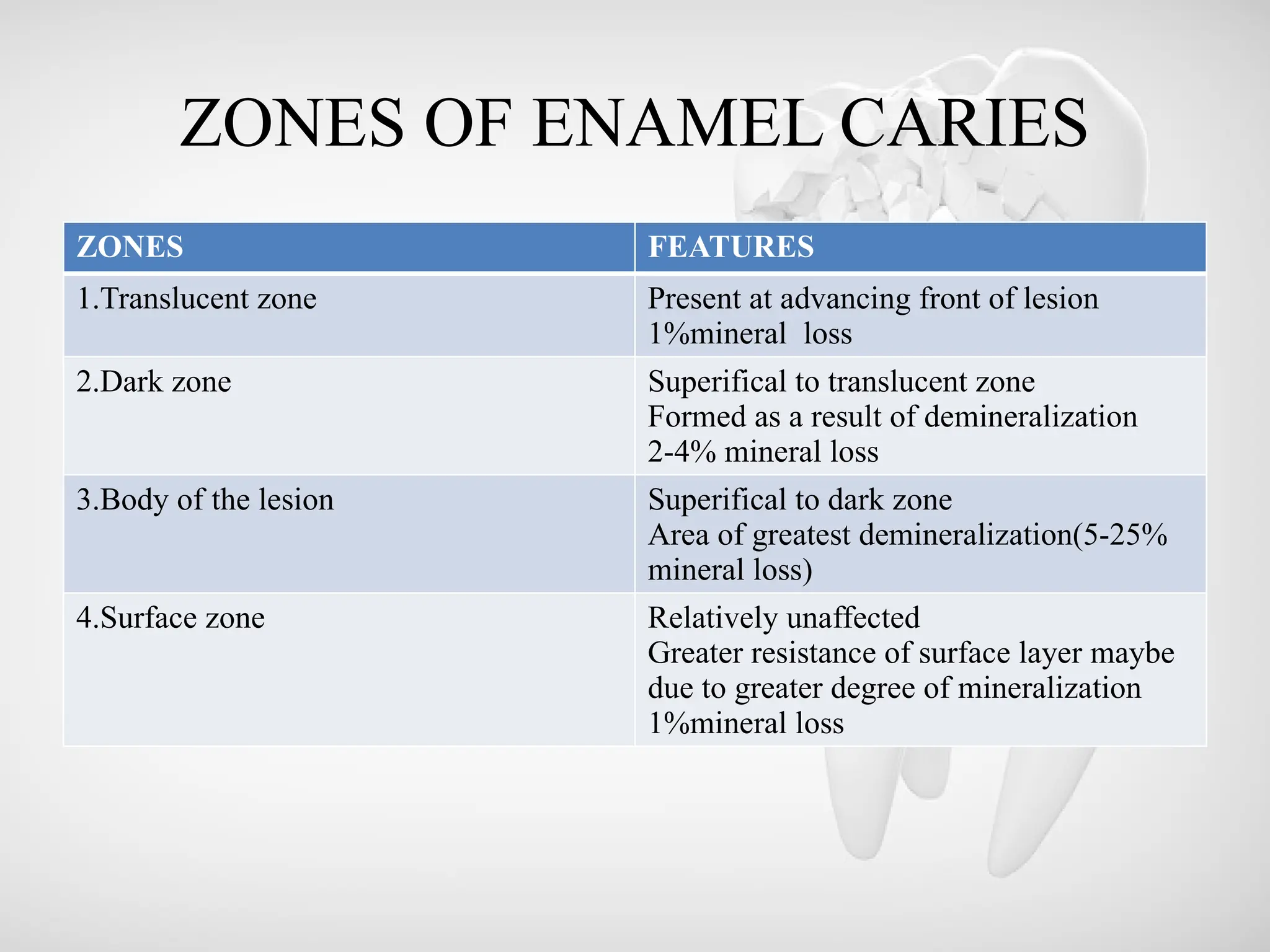
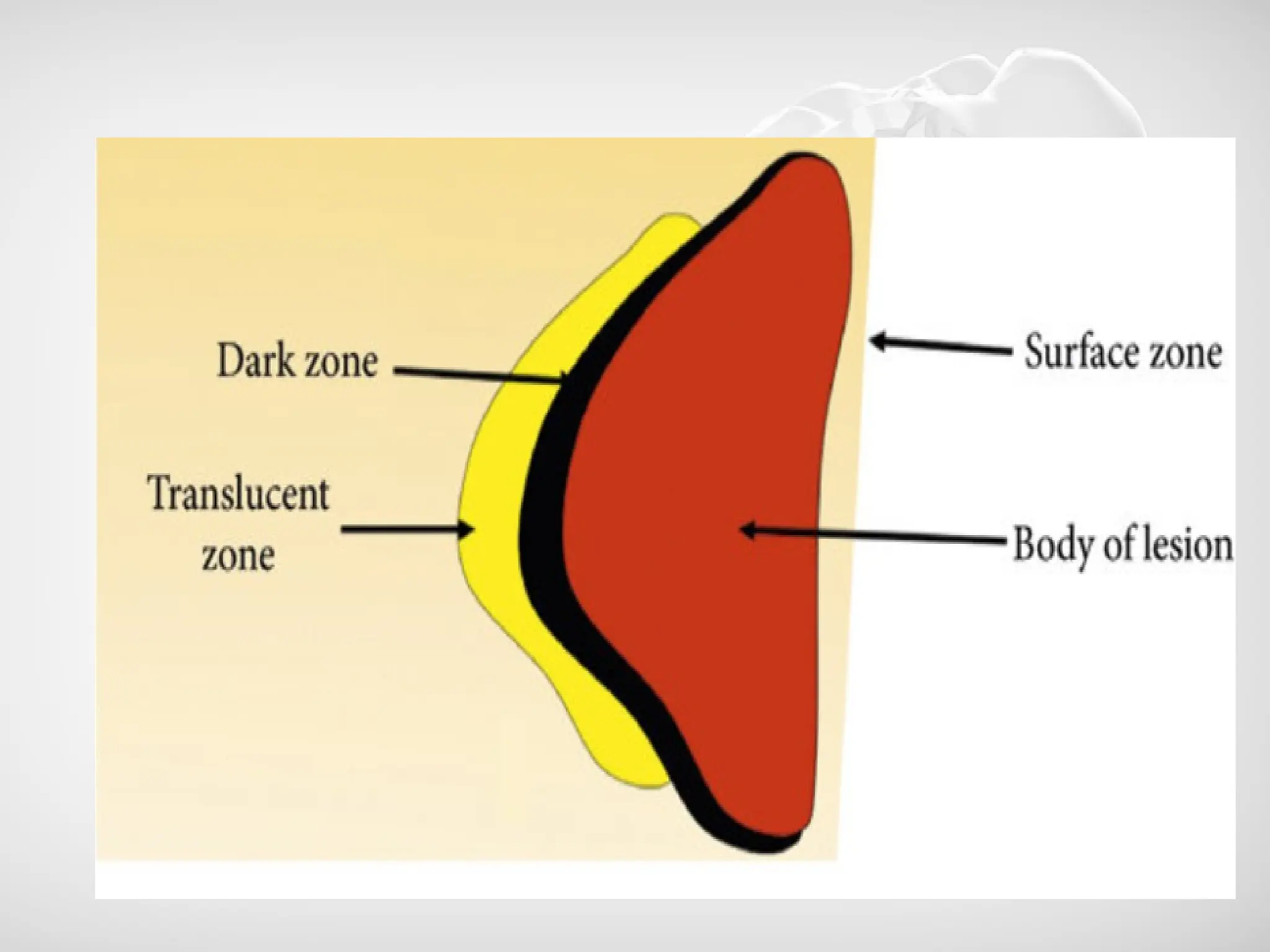
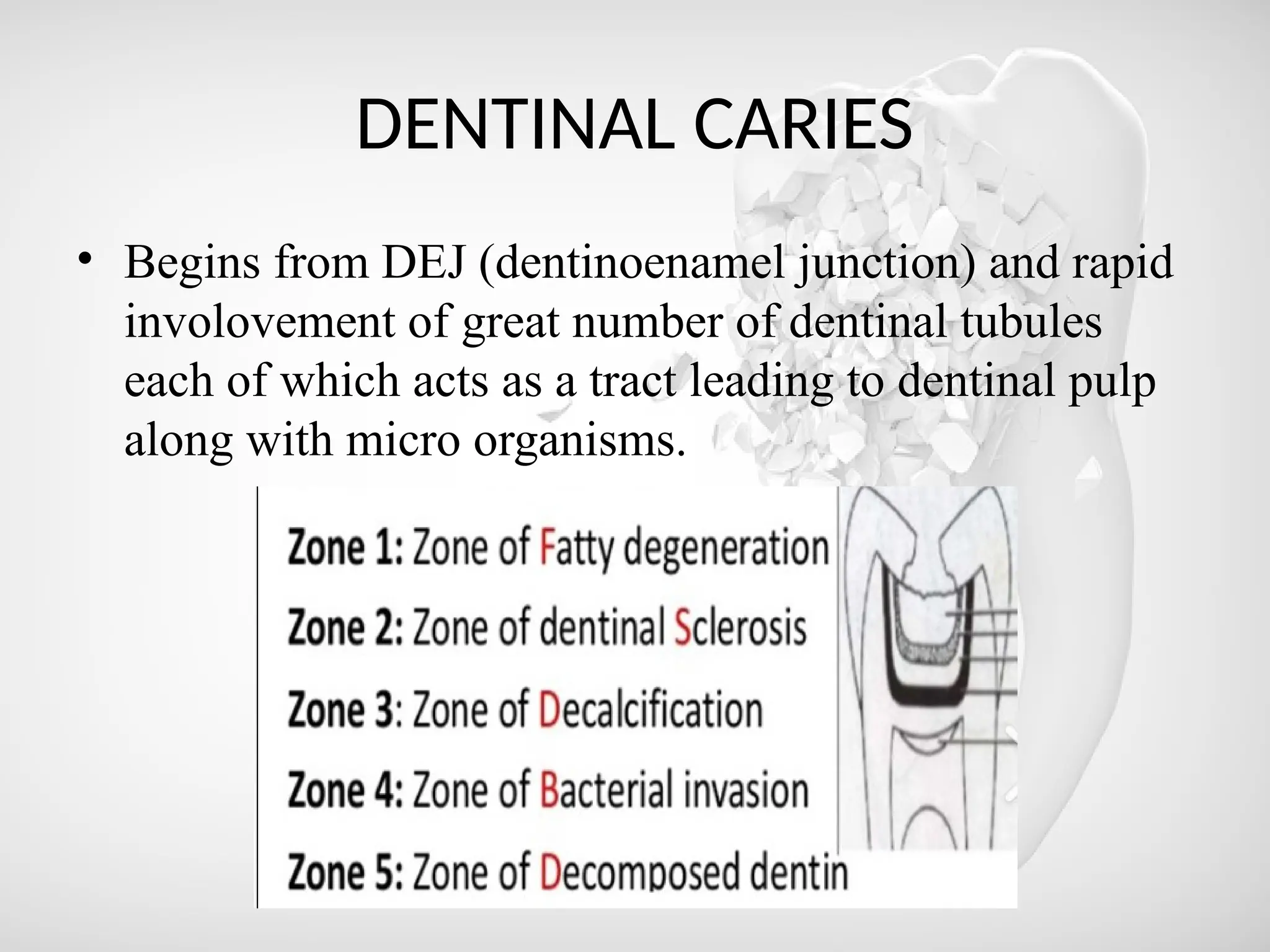
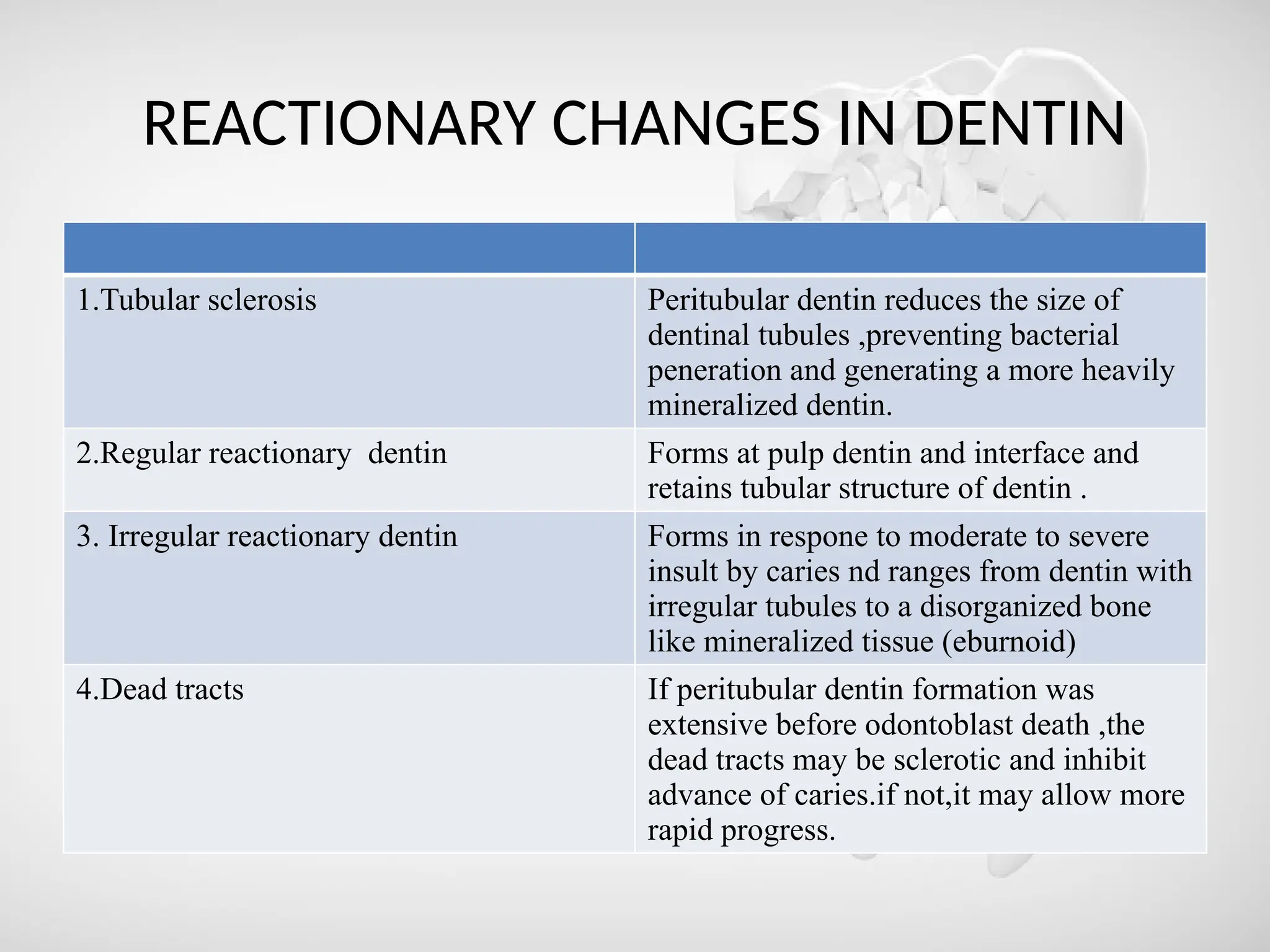
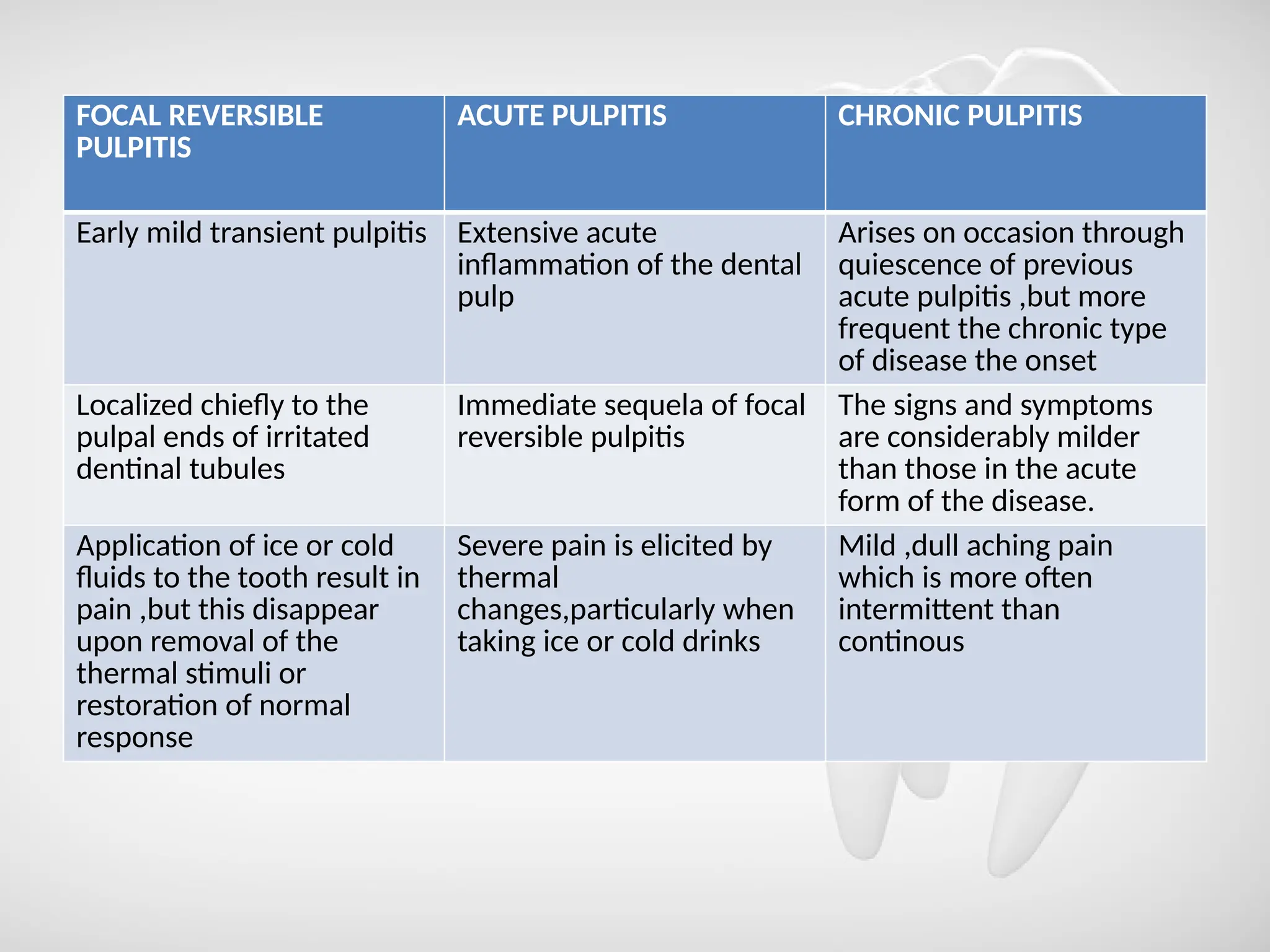
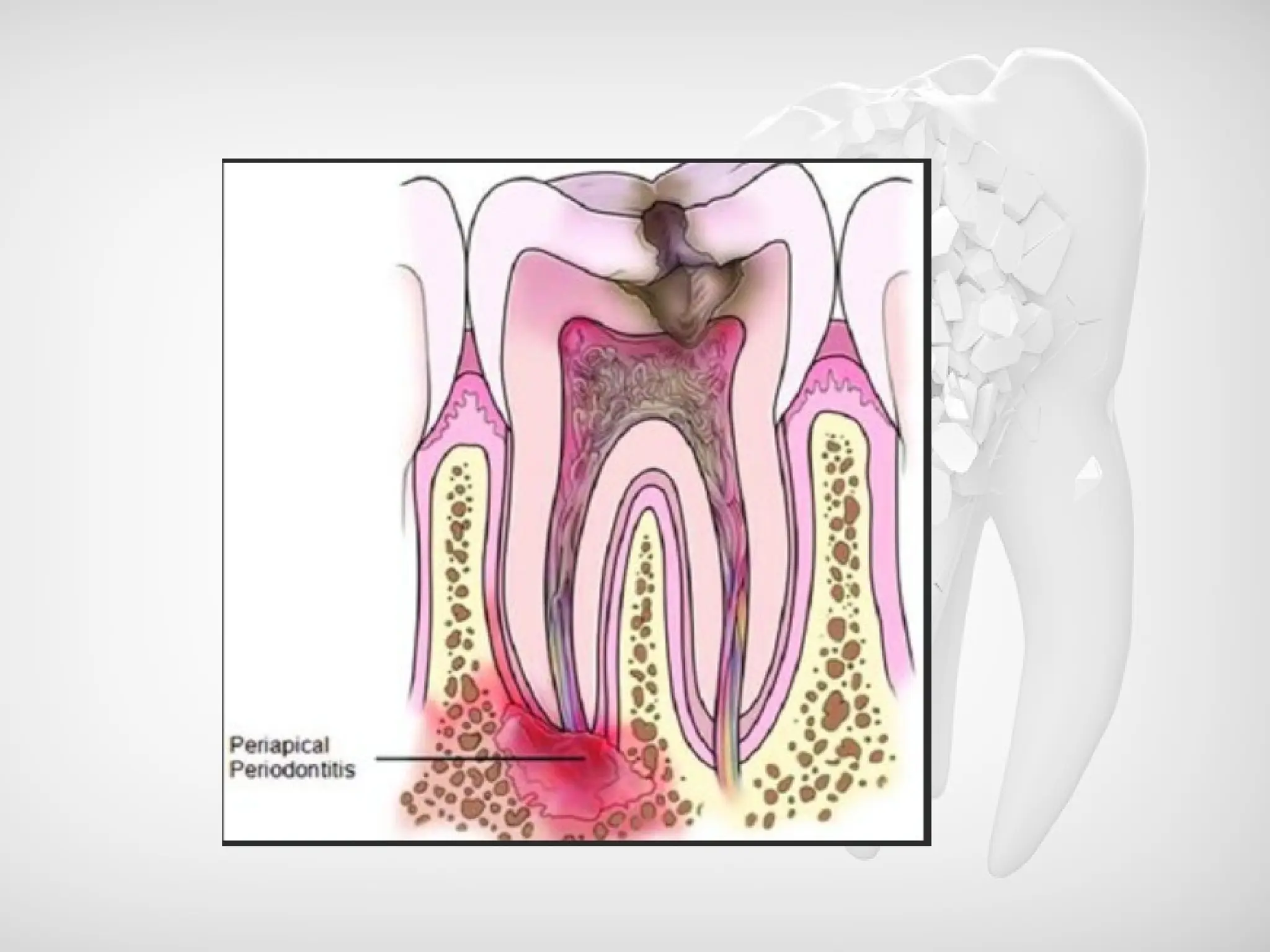
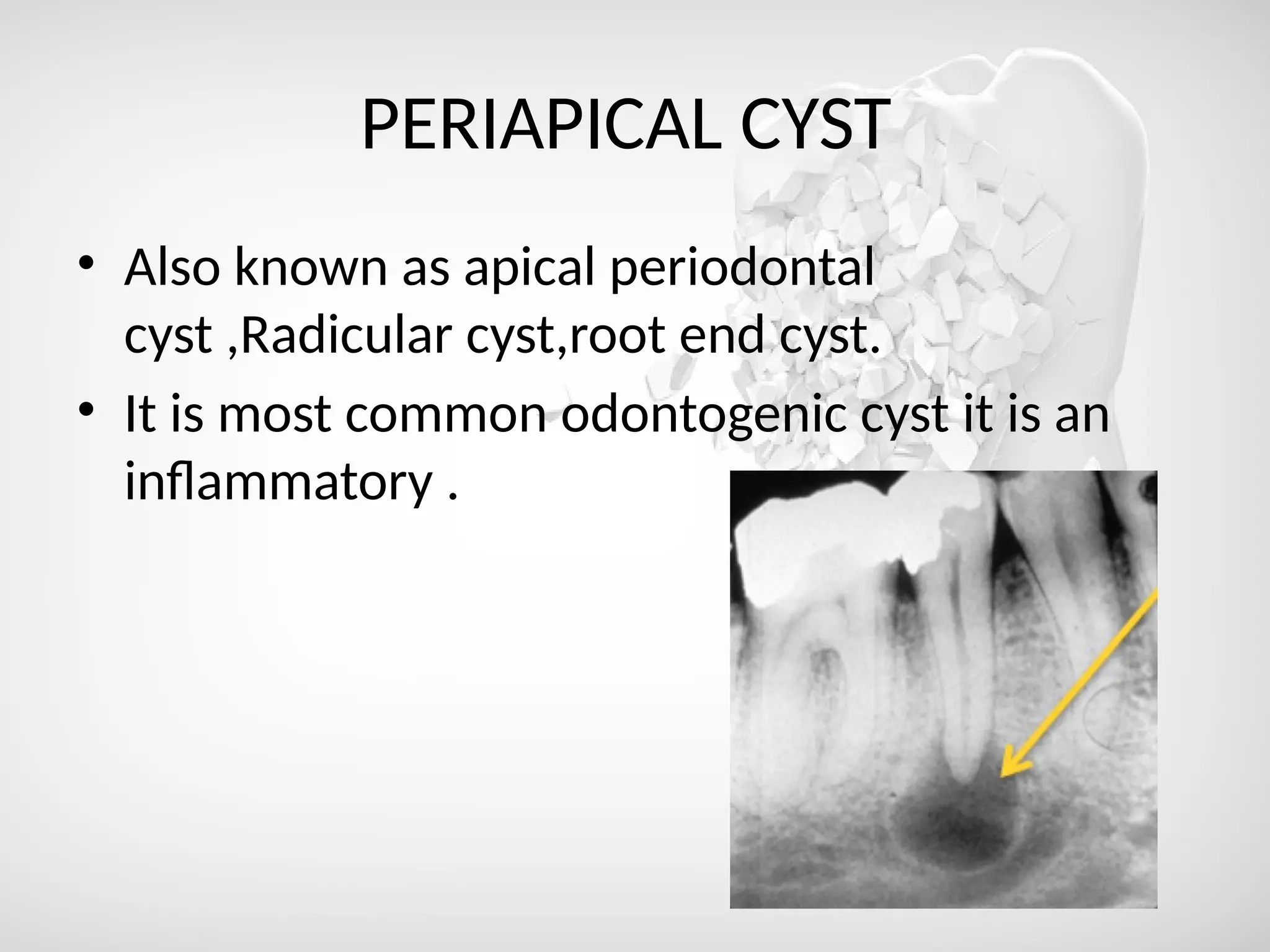
The document discusses the sequelae of dental caries, detailing definitions, types of caries, and related conditions such as pulpitis and periapical abscesses. It explains the progression from enamel caries to dentinal caries and associated inflammatory conditions like osteomyelitis. Treatments for these conditions vary from root canal therapy to extractions, highlighting the importance of addressing dental infections to prevent severe complications.