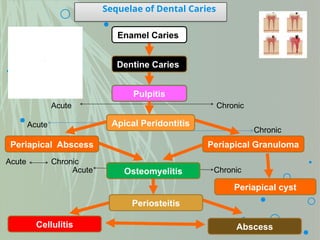
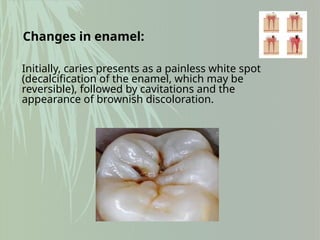
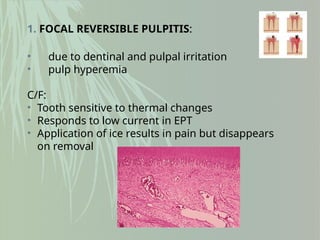
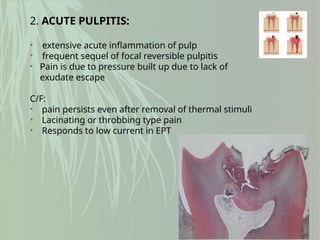
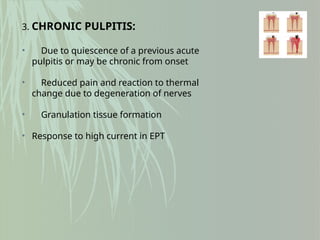
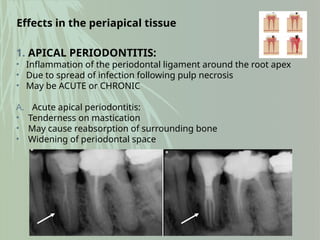
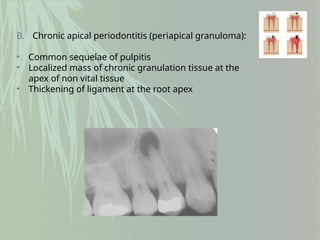
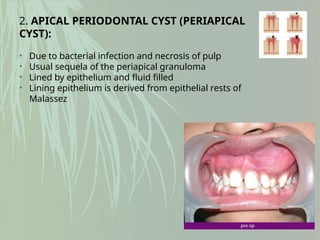
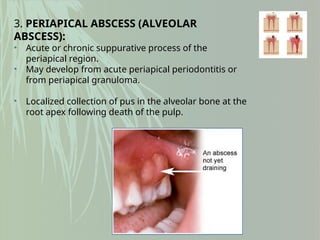
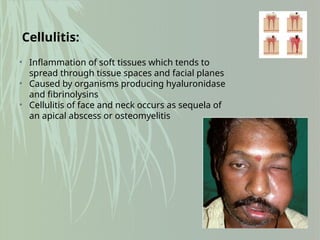
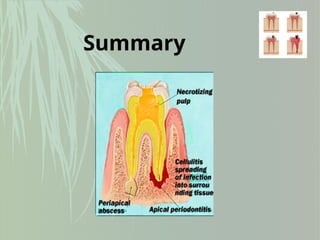
The document discusses the sequelae of dental caries, defined as a progressive microbial disease affecting tooth calcified tissues, leading to various conditions like pulpitis and periodontitis. It details the changes in enamel and dentin, types of pulpitis, and the implications for periapical tissues, including apical periodontitis and abscesses. References include authoritative textbooks on oral pathology and medicine.