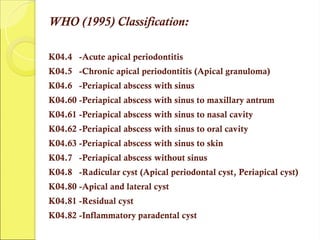
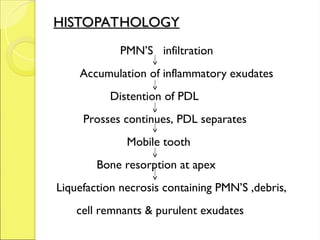
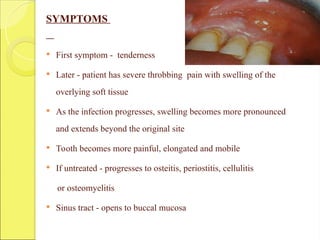
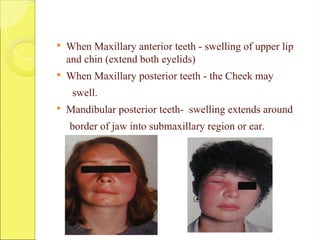
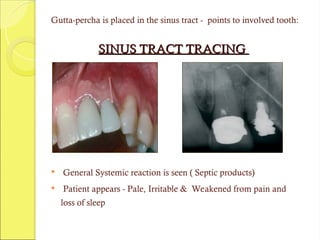
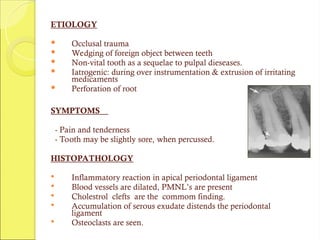
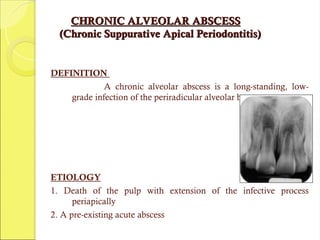
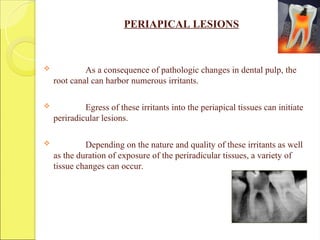
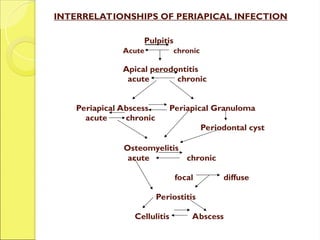
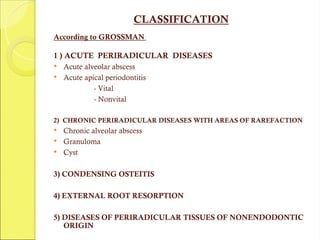
This document discusses the pathology and treatment of dental pulp and periapical infections, detailing symptoms, histopathological findings, and classifications of conditions such as acute and chronic periapical periodontitis and alveolar abscesses. It outlines diagnostic criteria and various treatment approaches including root canal therapy, establishment of drainage, and management of infections. The document also includes classifications by different authorities regarding the types of periapical diseases and their clinical presentations.
![WEINE’S CLASSIFICATION
PULPOPERIAPICAL DISEASE:
1] PAINFUL PULPOPERIAPICAL PATHOSES
a) Incipient acute periapical periodontitis
b) Advanced acute periapical periodontitis
i. Acute periapical abscess
ii. Recrudescent abscess
iii. Subacute periapical abscess
2] NON PAINFUL PULPOPERIAPICAL PATHOSES
a) Pulpoperiapical osteosclerosis
b) Incipient chronic periapical periodontitis
c) Advanced chronic periapical periodontitis
i. Periapical granuloma
ii. Chronic periapical abscess
iii. Periapical cyst](https://image.slidesharecdn.com/pulppatholgy3-241119192959-815f7234/85/Pulp-and-periapical-pathology-presentation-part-3-8-320.jpg)