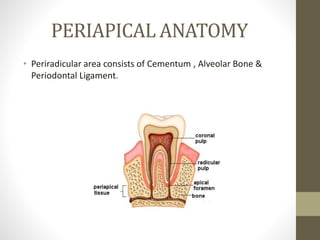
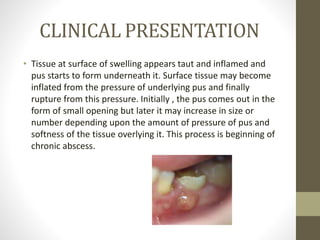
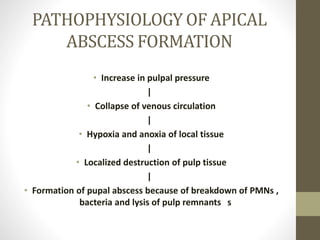
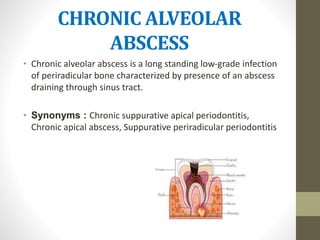
This document discusses different types of periapical abscesses, including acute periapical abscesses, phoenix abscesses, and chronic alveolar abscesses. It describes the etiology, symptoms, diagnosis, and treatment of each. Bacteria entering the pulp through breaks in dentin are the most common cause of these periradicular tissue lesions. Acute periapical abscesses present with rapid onset pain and swelling, while chronic alveolar abscesses are generally asymptomatic but can be detected by sinus tracts or radiographs. Treatment involves drainage, antibiotics if needed, and resolving the pulpal infection through root canal treatment or extraction.