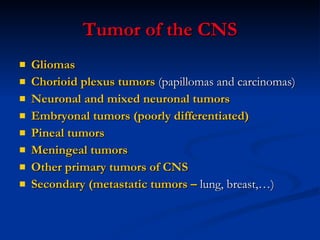
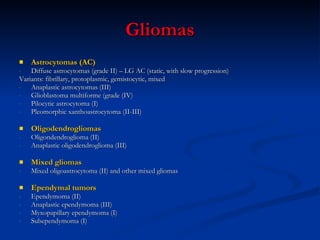
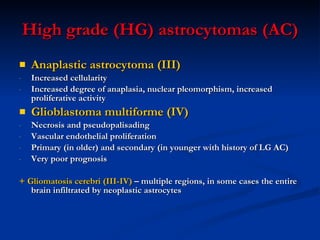
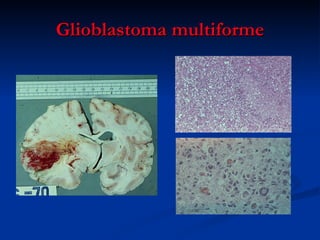
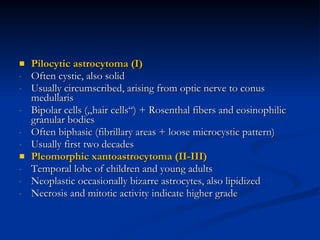
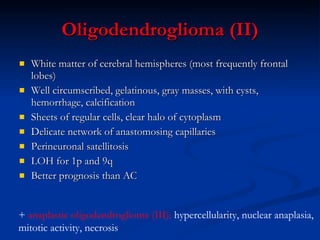
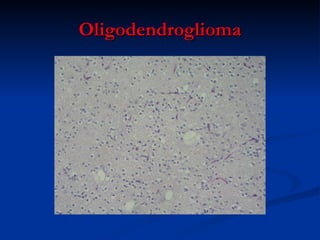
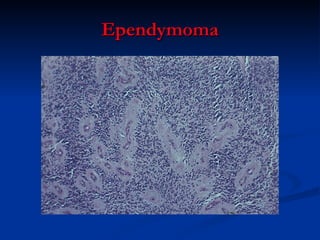
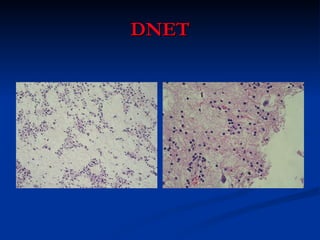
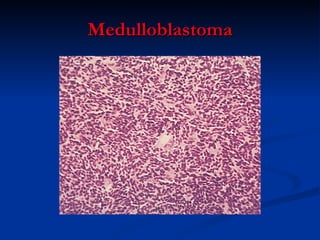
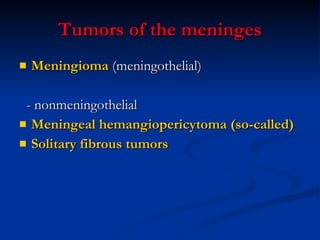
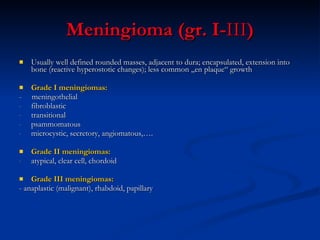
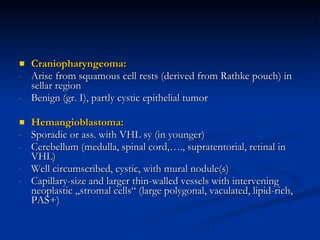
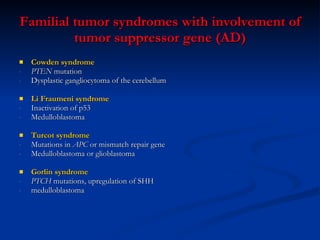
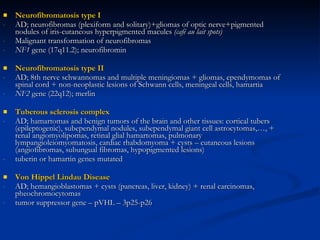
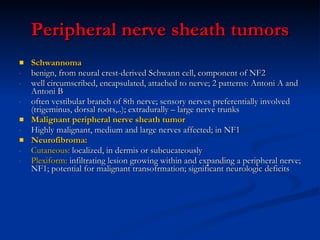
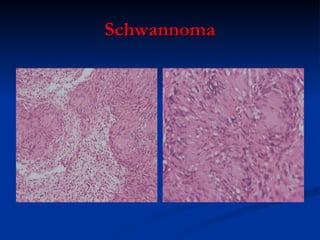
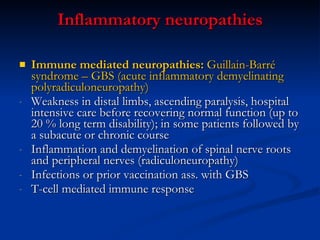
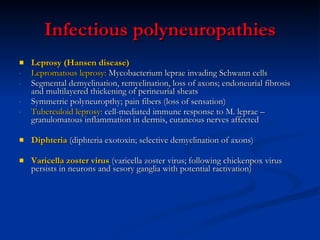
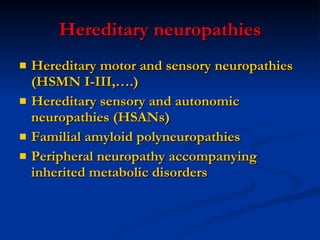
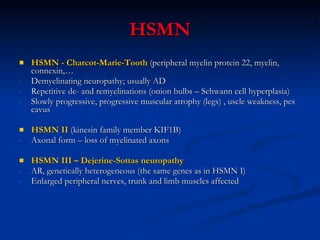
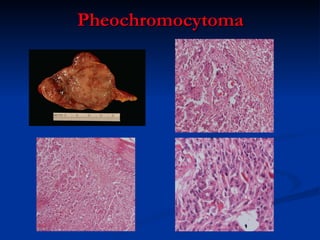
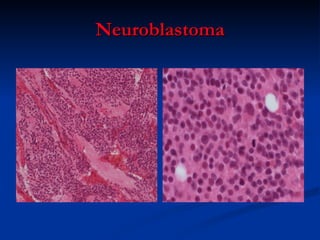
The document summarizes various tumors of the central nervous system (CNS) and peripheral nervous system. It describes different types of gliomas, neuronal and mixed neuronal tumors, embryonal tumors, meningiomas, and other primary and secondary CNS tumors. It also discusses peripheral nerve sheath tumors, diseases of the peripheral nerves including various hereditary, infectious, inflammatory, and acquired neuropathies.