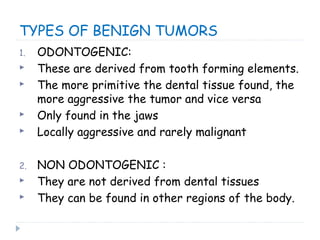
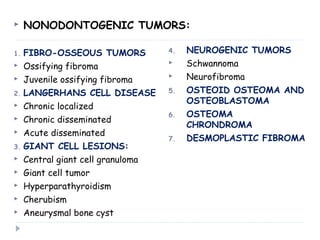
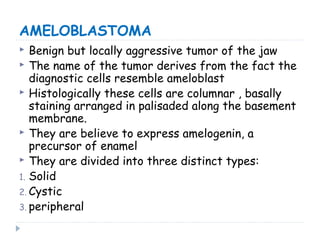
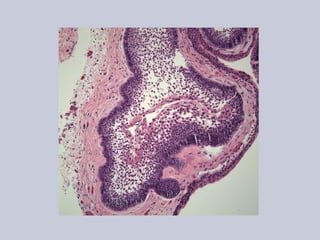
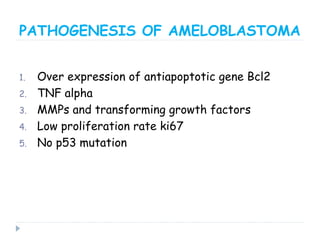
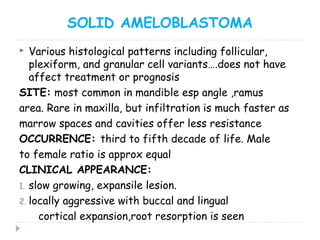
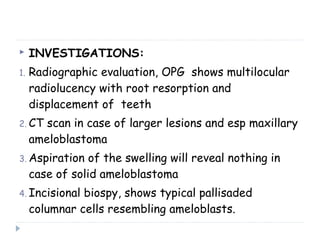
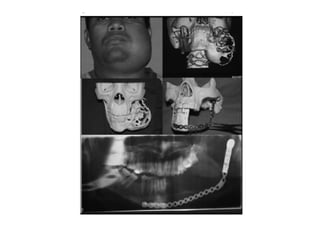
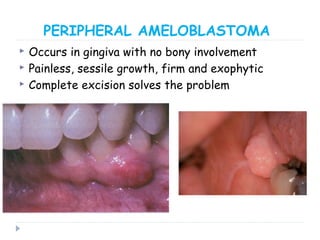
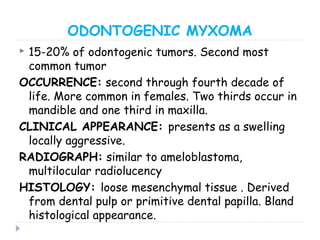
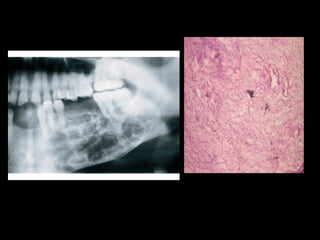
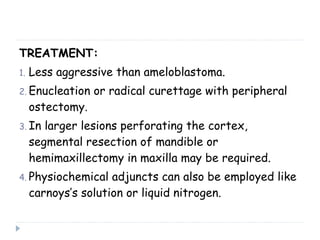
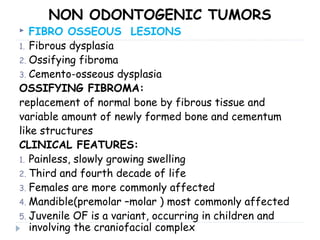
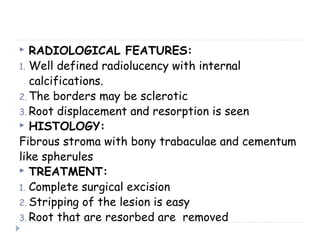
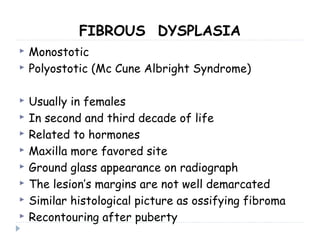
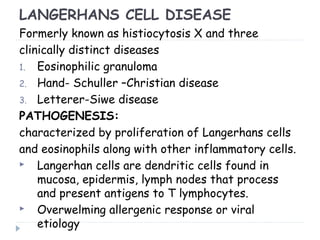
This document discusses benign tumors of the orofacial region, classifying them as either odontogenic or non-odontogenic tumors. Odontogenic tumors are derived from tooth forming elements and include ameloblastoma, calcifying epithelial odontogenic tumor, and adenomatoid odontogenic tumor. Non-odontogenic tumors include fibrous dysplasia, ossifying fibroma, and Langerhans cell disease. Ameloblastoma is the most common odontogenic tumor and presents as a slow growing, locally aggressive lesion that is treated with wide surgical resection. Calcifying epithelial odontogenic tumor contains sheets of epithelial cells and concentric calcification rings, while treatment involves wide excision.