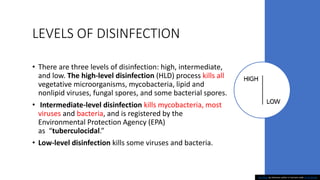
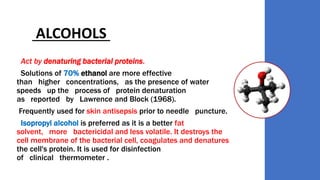
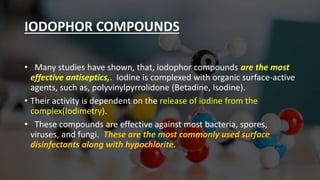
Proper cleaning, sanitization, and disinfection practices are important for reducing germs in surgical settings. Cleaning involves removing foreign material from surfaces using water and detergents. Sanitization reduces germs to a safe level using chemicals like bleach solutions. Disinfection uses chemicals to destroy pathogens, with high-level disinfection killing all vegetative microorganisms. Common disinfectants include alcohols, iodophors, and hydrogen peroxide, which act by denaturing proteins or oxidizing cell membranes. Surgical instruments must be thoroughly cleaned, sanitized, and disinfected using specific processes.