Salivary glands seminar
- 2. CONTENTS INTRODUCTION DEFINITION EMBRYOLOGY/DEVEOLPMENT HISTOLOGY OF SALIVARY GLANDS CLASSIFICATION OF SALIVARY GALNDS ANATOMY OF SALIVARY GLANDS AGE CHANGES CLINICAL CONSIDERATION CONCLUSION
- 3. INTRODUCTION What are Glands ? A gland is an organ which produces and releases substances that perform a specific function in the body. Classification of glands: Exocrine glands (Gr. Exo, outside,+ krinein, to separate) release their products onto an epithelial surface, either directly or through a duct e.g; the salivary glands.
- 4. Endocrine glands: (Gr, endon, within,+ krinein) release their products into the blood stream, e.g; thyroid gland. Mixed glands some glands possess both exocrine and endocrine function e.g; pancreas. Paracrine glands acts locally Secrete its products in to local extra cellular environment Ex: Entero endocrine cells of GIT
- 5. Baesd on the No. of cells. UNI CELLULAR MULTI CELLULAR I. Morphology of the duct/duct system. a. Simple b. Compound II. Shape of the secreting portion/portions. a. tubular b. alveolar or acinar gland. c. tubulo-alveolar (tubulo-acinar) glands. EXOCRINE
- 6. III. Basis of nature of secretory product: a. Mucous glands b. Serous glands c. Mixed (seromucous) glands IV. Basis of the mode of secretion: a. Holocrine glands b. Merocrine glands c. Apocrine glands d. Cytogenic glands
- 7. DEFINITION Salivary glands are compound tubuloacinar , merocrine , exocrine glands the ducts of which open into the oral cavity. - BERKOVITZ 3rd edition EMBRYOLOGY/DEVEOLPMENT Time of origin Gland Location Intra uterine life Parotid gland Corners of the stomodeum as placode 6th week I.U Submandibular gland Floor of the mouth End of 6th week I.U Sublingual gland Lateral to S.m.primordium 8th week I.U Minor salivary glands Buccal Epithelium 12th week I.U Maturity of secretory end piece: During last 2 months of gestation.
- 8. Stage I(Bud formation). Develops as proliferation of oral epithelium Into underlying ectomesenchyme (condensing around bud). A thin basal lamina separates the bud from underlying mesenchyme. Interaction of the epithelium with underlying condensing mesenchyme associated with salivary glands provide optimum environment for gland formation. DEVELOPMENT
- 9. Stage II (Formation and growth of epithelial chord.) The mesenchyme (MES) around the developing glandular epithelium also proliferates. Proliferation of the epithelial bud into the underlying mesenchyme results in long epithelial cords. Basal lamina is believed to play a role in influencing the morphogenesis & differentiation of the salivary glands.
- 10. Stage III (Initiation of branching in terminal parts of epithelial chord). Epithelial chord proliferates & its end branch into bulbs. Stage IV (Branching of epithelial chord and lobule formation): Terminal ends branch extensively forming numerous bulbs - cleft formation.
- 11. ECM component deposition within clefts apparently serve to stablise them. Connective tissue component below epithelial chord forms capsule & surrounds entire gland.
- 12. Stage V (Canalization): Lumen forms within the ducts before they develop within the terminal buds. Apoptosis of centrally located cells. Different rates of proliferation of outer and inner layers of epithelial chord. Lumen formation takes place at distal ends of chord, then in proximal and at last in central part. Secretion of fluid by ductal cells which increases the hydrostatic pressure within to form a canal.
- 13. Following lumen formation in the terminal buds, epithelium consists of two layers of cells. Inner cells differentiate into mucous or serous cells depending upon type of specific gland. Some of the outer cells of epithelium differentiate into myopithelial cells that are present around secretory end piece and intercalated ducts. Portion of epithelial bud close to the oral cavity forms main excretory duct, distal portion forms secretory end piece. Stage VI (Cytodifferentiation):
- 14. HISTOLOGY OF SALIVARY GLANDS SECRETORY UNITS(ACINI) -SEROUS -MUCOUS MYOEPITHELIA L CELLS DUCTAL UNITS INTERCALATED DUCTS -STRIATED DUCTS -EXCRETORY DUCTS CONNECTIVE TISSUE: Surrounding capsule Tissue septae Tissue elements
- 15. Serous cells: Pyramidal with a broad base on the basement membrane, apex facing the lumen Secretory granules – Zymogen granules present in the apical cytoplasm Abundance of RER Mature zymogen granules expelled from the cell surface by exocytosis
- 16. Mucous cells: Typically have a tubular configuration Mucous end pieces in some cases have serous cells associated with them in the form of a demilune The most prominent feature of mucous cells is the accumulation in the apical cytoplasm of their secretory product –mucus Have a large Golgi complex, located basal to the mass of secretory granules
- 17. Contractile elements associated with the secretory end pieces and intercalated ducts Stellate shaped, numerous branching processes which envelop the secretory end piece Contraction of these processes provides support to the end pieces during active secretion of saliva Myoepithelial cells:
- 18. Ductal Elements: Acini Intercalated ducts Striated ducts Excretory ducts Stenson’s/whartons duct
- 19. • Single layer of cuboidal cells • Secretory units may also secrete lysozyme and lactoferrin Intercalated ducts • Constitute largest portion of ductal system; Columnar cells • Modification of primary saliva by reabsorbtion and secretion of electrolytes Striated ducts • Pseudostratified columnar epithelium • Other types of cells viz. Tuft cells, lymphocytes and macrophages may be present within Terminal excretory ducts
- 20. CONNECTIVE TISSUE: Capsule –demarcate gland from adjacent structures. Septa –divide gland into lobes and lobules -Carry the nerves and blood vessels and excretory ducts. Fibroblast, Macrophages, Dendritic cells, Mast cells,Plasma Cells, Adipose tissue. Collagen fibers and elastic fibers along with glycoprotein and proteoglycans of the Ground substances
- 21. CLASSIFICATION OF SALIVARY GALNDS SALIVARY GLANDS BASED ON ANATOMY •MAJOR SALIVARY GLANDS •PAROTID GLAND •SUBLINGUAL GLAND •SUBMANDIBULAR GLAND •MINOR SALIVARY GLANDS •LABIAL AND BUCCAL GLANDS •GLOSSOPALATINE GLANDS •PALATINE GLANDS •LINGUAL GLANDS •-BLANDIN &NUHN •-VON EBNER’S GLAND •CARMALT’S GLANDS SALIVARY GLANDS BASED ON SECRETION SEROUS MUCOUS MIXED
- 22. SEROUS GLANDS •PAROTIDGLAND •VON EBNER’S GLAND’S MUCOUS GLANDS GLOSSOPALATINE & PALATINE GLANDS MIXED GLANDS • SUB LINGUAL GLANDS • SUB MANDIBULAR GLANDS • LABIAL & BUCCAL GLANDS • LINGUAL GLANDS
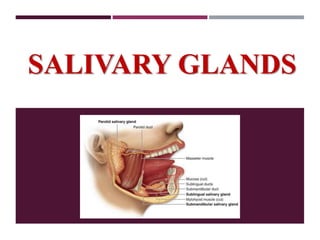
- 23. ANATOMY OF SALIVARY GLANDS PAROTID GLAND: Largest salivary gland 60 to 65% of total saliva. Pyramidal in shape. Weights between 14-28g. It is situated below external acoustic meatus ,b/w ramus of mandible and sternocleido mastoid muscle. Anteriorly the gland overlaps the masseter muscle.
- 24. Parotid Capsule • The investing layer of deep cervical fascia forms the capsule for the gland. • The fascia splits to enclose the gland. • Superficial lamina – thick & adherent to the gland. •Deep lamina – thin , attached to the styloid process, the mandible and tympanic plate. • A portion of deep lamina, extending between the styloid process and the mandible – thickened to form Stylomandibular Ligament, separates the Parotid gland from the Submandibular salivary gland.
- 25. External Features The glands has four surfaces a) Superior b) Superficial c) Antero-medial d) Postero-medial The surfaces are separated by three borders. a) Anterior b) Posterior c) Medial
- 26. Relations 1.Superior surface related to External acoustic meatus Superficial temporal vessels Posterior surface of TMJ Auriculotemporal nerve 2.Superficial surface (largest) a) Skin b) b) Superficial fascia i. Great auricular nerve ii) Pre-auricular lymph node iii) Posterior fibers of platysma c) Parotid fascia d) Deep parotid lymph nodes
- 27. 3. Anteromedial surface Masseter Lateral surface of TMJ Posterior border of the mandible Medial pterygoid Terminal branches of facial nerve 4. Posteromedial surface Mastoid process Sternocleidomastoid Posterior belly of the digastric Styloid process.
- 28. 6 . Anterior border : Separates the superficial surface from the Anteromedial surface Extends from –anterior part of the superior surface to the apex Structures emerging: a. Parotid duct b. Terminal branches of the facial nerve c. Transverse facial vessels
- 29. 7. Posterior border Separated the superficial surface from the posteromedial surface Overlaps the sternomastoid. 8.Medial border : Separates the Anteromedial surface from the posteromedial surface. Related to the lateral wall of pharynx
- 30. Parotid duct: Runs forward across masseter muscle, turns inwards at the anterior border of masseter & opens at a pappilla in oral cavity just opposite second maxillary molar crown. 5cm long.
- 31. Terminal branches of facial nerve a) Temporal b) Zygomatic c) Buccal d) Mandibular e) cervical Parasympathetic nerves are secretomotor. Reach the gland through the auriculotemporal nerve. NERVE SUPPLY:
- 32. Sensory – auriculotemporal nerve. Sympathetic nerves are vasomotor –Derived from the plexus around the external carotid artery.
- 33. VASCULAR SUPPLY ECA-external carotid artery Maxillary artery Superficial temporal vessels Posterior auricular artery
- 34. Veins Retromandibular vein divides into: 1. Posterior division drains into external jugular vein 2. Anterior division drains into common facial vein Lymphatic Drainage Upper deep cervical nodes
- 35. Situated in the anterior part of the Digastric triangle Size that of a walnut Is J-shaped Secretion of submandibular gland is both serous and mucous. SUBMANDIBULAR GLAND
- 36. The gland is partly enclosed in 2 layers of deep cervical fascia. 1. Superficial layer of fascia • Covers the inferior surface of the gland • Attached to the base of the mandible 2. Deeper layer of fascia • Covers the medial surface of the gland • Attached to the mylohyoid line of the mandible
- 37. Superficial Part: Inferiorly: Skin Platysma Cervical branch of facial nerve Deep fascia Facial vein Submandibular Lymph Nodes Laterally • Submandibular fossa on the mandible • Insertion of medial pterygoid • Facial Artery Medially: • Mylohyoid • Hyoglossus • Styloglossus Deep part: Laterally: • Hypoglossal nerve. Inferiorly: • Mylohyoid muscle. Medially: • Hyoglossus muscle.
- 38. Wharton’s Duct: Thin walled, about 5 cm long Emerges at the anterior end of the deep part of the gland Crossed by the lingual nerve at the region of anterior border of the hyoglossus Opens on the floor of the mouth, on the summit of the sublingual papilla, at the side of tongue frenulum
- 39. Blood and veins Supply: Supplied by the facial artery Veins drain into the common facial or lingual vein Lymphatic drainage: • Submandibular lymph node & deep cervical lymph nodes.
- 40. Submandib ular ganglion Secretomotor fibres Vasomotor sympathetic fibres from facial artery plexus Sensory fibres from lingual nerve Nerve Supply
- 41. SUB LINGUAL GLAND Smallest major salivary gland Almond shape wt. abt 3 to 4 gms. Lies above the mylohyoid muscle, below the mucosa of floor of the mouth, medial to sub lingual fossa of mandible, lateral to genioglossus muscle. Abt 15 ducts emerges from the gland. Most of them opens directly in to the floor of mouth on summit of sublingual gland fold.
- 42. Blood supply: Sublingual & submental arteries. Lymphatic drainage: Submental lymph nodes Nerve supply: Parasympathetic supply: Facial nerve reaching gland through the lingual nerve & submandibular ganglion. Sympathetic Supply: -Postganglionic fibers from plexus on facial artery.
- 43. They are located beneath the oral epithelium in almost all parts of the oral cavity except in the gingiva, ant. Hard palate and ant. 2/3rd of tongue dorsum 600 – 1000 in number present in small clusters of secretory units Rich in mucin, antibacterial proteins and secretory immunoglobulin. MINOR SALIVARY GLANDS
- 44. MINOR SALIVARY GLANDS Continuous slow secreting glands, thus have a important role in protecting and moistening oral mucosa, especially when major salivary glands are mostly inactive.
- 45. “Saliva is clean, tasteless, odourless, slightly acidic viscous fluid, consisting of secretions from the parotid, sublingual, submandibular salivary glands and the mucous glands of the oral cavity.” - Stedmans medical dictionary 26th edition. PROPERTIES OF SALIVA VOLUME:- 1000 to 1500 ml of saliva is secreted per day and it is approximately about 1ml/minute . Specific Gravity : 1.002 to 1.008 pH: 6.2 to 7.6 (6.7) TONICITY :- saliva is hypotonic to plasma. SALIVA
- 46. Saliva Organic substance Inorganic substance Water-99.5% solids 0.5% Enzymes Other org. substance 1.amylase 2.maltase 3.lingual lipase 4.lysozyme 5.phosphatas e 6.carbonic anhydrase 7.kalikrein 1.Proteins- mucin & albumin 2.Blood group antigen 3.Free amino acids 4.Non protein nitrogenous substances-urea,uric acid,creatinine,xanthi ne hypoxanthine 1.Sodium 2.Calcium 3.Potassium 4.Biocarbonate 5.Bromide 6.Chlorine 7.Fluoride 8.phosphate 1.Oxygen 2.Carbon dioxide 3.Nitrogen
- 48. AGE CHANGES Acinar Atrophy Peri Acinar Callus formation Ductal Dilatation Fatty infilteration Fibrosis Inflammatory Infiltration Oncocytes
- 49. Ptyalism is an abnormal condition characterized by increased secretion of saliva in the mouth. PTYALISM CLINICAL CONSIDERATION
- 50. APTYALISM (XEROSTOMIA) Aptyalism is the pathological condition characterized by a decrease or complete cessation of secretion of saliva, causing dryness of mouth.
- 51. Soreness, burning or pain sensations in the mouth. Due to dry, sticky oral mucosa, tongue always sticks to the palate and there is difficulty in swallowing. Taste disorder (dysgeusia) and burning tongue (glossodynia). Whatever saliva is present, it looks stringy, ropy or foamy. ‘Lipstick sign’ is positive for women (lipstick always sticks to the upper front teeth) Difficulty in wearing artificial prosthesis. Candidiasis is the most common oral infection, which is persistently present. CLINICAL FEATURES
- 52. Removal of local or systemic causes. Chewing xylitol containing gums Regular use of artificial saliva (carboxymethyl cellulose containing saliva) Antifungal drugs Administration of pilocarpine and use of transmucosal neurostimulatory devices to stimulate the salivary secretion in patients, who still retain some degree of salivary function. Avoidance of antihistaminic and decongestant drugs. TREATMENT
- 53. Cystic lesion developing from the salivary glands are commonly known as “mucoceles” Mucocele-(MUCUS EXTRAVASATION PHENOMENON). It results from the rupture of a salivary gland duct and spillage of mucin into the surrounding soft tissues. Mucocele is not a true cyst as it lacks epithelial lining Mucocele
- 54. Clinical Features 75 % of mucoceles occur in the lower lip. Mucoceles are dome shaped mucosal swellings measuring from 1-2 mm to several centimeters in size. They are mostly fluctuant and exhibit a bluish translucent hue as a result of the spilled mucin.
- 55. Some mucoceles are short-lived lesions that rupture and heal by themselves. Many lesions, however, are chronic in nature, and local surgical excision is necessary. To minimize the risk of recurrence, should remove any adjacent minor salivary glands that may be feeding into the lesion when the area is excised. Treatment
- 56. RANULA Ranula is a term used for mucoceles that occur in the floor of the mouth, arising from the sublingual gland. The name is derived from the Latin word rana, which means “frog,”because the swelling may resemble a frog’s translucent underbelly. Causes for Ranula Formation i. Trauma, ii. obstructed salivary gland or ductal aneurysm. Clinical Features It presents as a smooth, fluctuant, painless swelling on the floor of the mouth, lateral to the midline.
- 57. The color ranges from normal to a translucent bluish, and the size is usually in the range of 1–3 cm, or larger. “Plunging or cervical ranula” is a term used to refer to deep seated lesion that herniates through the mylohyoid muscle and extends along the fascial planes.
- 58. Intralesional injection of corticoseroids can be used for treating small lesions and to reduce the size of larger ranulas. Marsupialiazation along with unroofing of the lesion is generally helpful. Surgical excision of lesion and the associated salivary gland is carried out for larger lesions Treatment
- 59. SIALOLITHIASIS Sialolithiasis is a pathological condition, characterized by the presence of one or more calcified stones (sialoliths) within the salivary gland itself or within its duct. Clinical Feature: Patient complains of episodic pain and swelling of the affected gland especially with the intake of food.
- 60. Sialogogues that stimulate salivary secretion can be prescribed. Larger sialoliths can be removed surgically Treatment: Sialoliths of smaller dimension can be milked through the duct to the ductal orifice by gentle massage of the obstructed duct. Sialoliths that are presented at the terminal portion of the duct can be palpated as a hard mass
- 61. Sjogren’s syndrome is a multi-system immunemediated chronic inflammatory disease, characterized by lymphocytic infiltration and acinar destruction of salivary and lacrimal glands,with a marked predilection for women. Clinical Forms 1. Primary Sjögren’s syndrome: (sicca syndrome)–xerostomia and xerophthalmia 2. Secondary Sjögren’s syndrome – sicca syndrome + presence of an autoimmune disorder SJOGREN’S SYNDROME
- 62. Xerostomia or dryness of mouth often causes soreness of mouth with difficulty in eating, swallowing and talking, etc. parotid glands are persistently enlarged, often bilaterally and the swelling is usually painless. CLINICAL PRESENTATION
- 63. Pt may have dryness of the nasal,pharyngeal and laryngeal mucosa. Histologically the disease is characterized by lymphocytic infiltration and acinar destruction of salivary and lacrimal glands. INVESTIGATIONS Biopsy Sialography Scintigraphy Schirmer test
- 64. TREATMENT • Use of artificial saliva • Use of systemic steroids • Antibiotic eye drops • Anti fungal drugs • Maintenance of oral hygiene, avoidance of sweets and fluoride applications to control caries.
- 65. 1. Adenomas • Pleomorphic adenoma • Basal cell adenoma • Warthin’s tumor (adenolymphoma) • Oncocytoma (oncocytic adenoma) • Sebaceous adenoma • Cystadenoma 2. Carcinomas • Acinic cell carcinoma • Mucoepidermoid carcinoma • Adenoid cystic carcinoma • Basal cell adenocarcinoma • Squamous cell carcinoma • Small cell carcinoma • Undifferentiated carcinoma • Other carcinomas 3. Nonepithelial tumors 4. Malignant lymphomas 5. Secondary tumors 6. Unclassified tumors 7. Tumor like lesions classification of salivary gland tumors(WHO 1991) • Sialadenosis • Oncocytosis • Necrotizing sialometaplasia • Salivary gland cysts
- 66. PLEOMORPHIC ADENOMA Pleomorphic adenoma or benign mixed tumor is the most common neoplasm of the salivary glands, which is histologically characterized by complex intermingling of epithelial components and the mesenchymal areas. ORIGIN According to the multicellular theory, these tumors originate from intercalated duct cells and myoepithelial cells of the salivary glands.
- 67. Clinical Features slow growing, painless, well-delineated, nodular exophytic growth. It is usually solitary but sometimes there can be multiple lesions (multinodular) . smooth surfaced, soft or slightly firm, dome-shaped nodular swellings on the hard or soft palate. Facial nerve palsy is a rare feature.
- 68. The neoplasm exhibits proliferation of glandular, basophilic epithelial cells in the form of diffuse sheets or clusters. These neoplastic have a tendency to form duct like structures, which are often filled with eosinophilic mucins. The connective tissue stroma of pleomorphic adenoma often characteristically exhibits metaplastic changes, which results in the formation of mucoid, myxoid, chondroid and osseous tissues within the tumor. HISTOPATHOLOGY
- 69. CONSERVATIVE SUPERFICIAL PAROTIDECTOMY Treatment Tumour along with the normal lobe is removed Preserve the facial nerve, even in malignant tumours unless grossly involved Avoid rupture of the gland Enucleation should not be done as it causes recurrence
- 70. Adenolymphoma is a benign salivary gland neoplasm with limited growth potential. It is primarily occurring in the parotid and is composed of cystic spaces with intraluminar projections lined by double layer of cells. CLINICAL FEATURES Middle aged or elderly males are commonly affected—usually they are smokers. Can be bilateral, in some cases (10%). May be multicentric ADENOLYMPHOMA (WARTHIN’S TUMOR)
- 71. It has smooth surface, round border with soft, cystic consistency. This tumour affects only parotid gland.
- 72. Histology This tumor is made up of two histologic components: epithelial and lymphoid tissue. As the name would indicate, the lesion is essentially an adenoma exhibiting cyst formation, with papillary projections into the cystic spaces and a lymphoid matrix showing germinal centers
- 73. Partial superficial parotidectomy. TREATMENT
- 74. ADENOID CYSTIC CARCINOMA (CYLINDROMA) Adenoid cystic carcinoma is a malignant neoplasm arising from the glandular epithelium of either major or minor salivary glands. It has profound tendency to invade into the perineural lymphatic spaces. Freq. occurs at the age of 50 to 70 years. more prevalent among females. most common sites for development in minor glands are the palate and tongue, In the major gland , it is the most Common submandibular salivary gland CLINICAL FEATURES
- 75. The lesion often produces a relatively slow enlarging growth, with frequent surface ulcerations. It frequently invade the facial nerve sheath, lingual and the hypoglossal nerves. Pain is very common feature in this tumor and severe neurological signs like anesthesia, paresthesia or palsy frequently develop.
- 76. Adenoid cystic carcinoma is composed of myoepithelial cells and ductal cells which have a varied arrangement. Histologically, adenoid cystic carcinomas have three subtypes: A. Cribriform pattern (classic). B. Tubular pattern. C. Solid pattern (basaloid). Cribriform pattern (classic). The cribriform pattern shows basaloid epithelial cell nests that form multiple cylindrical cyst like patterns resembling a Swiss cheese or honey comb pattern, which is the most classic and best recognized pattern HISTOPATHOLOGY
- 77. Tubular pattern. The tubular pattern reveals tubular structures that are lined by stratified cuboidal epithelium. Solid pattern (basaloid). The solid pattern shows solid groups of cuboidal cells with little tendency towards duct or cyst formation.
- 78. By wide surgical excision. Post surgical radiotherapy is effective since the tumor cells are radiosensitive. Short-term prognosis is good but long-term prognosis is grave. TREATMENT
- 79. MUCOEPIDERMOID TUMOR Mucoepidermoid tumor is an unusual type of malignant salivary gland neoplasm with varying degree of aggressiveness. The tumors arise from the excretory duct cells of the salivary gland It predominantly affects parotid and minor salivary glands, it also frequently affects the jawbone. Clinically, the tumor presents slow growing, painless swelling that often has a cystic feeling.
- 80. Some lesions cause fast enlarging swelling, with pain, ulceration, paresthesia and hemorrhage, etc. Nodular mass on the left posterior lateral hard palate.
- 81. mucoepidermoid tumor consists of three distinct types of cells: (A) large pale mucous secreting cells. (B) epidermoid cells. (C) intermediate type of cells. Mucoepidermoid carcinomas are graded as a)low-grade. b)intermediate-grade. c)high-grade. HISTOLOGICALLY
- 82. Low-grade tumors show well formed glandular structures and prominent mucin filled cystic spaces, minimal cellular atypia and a high proportion of mucous cells (Low grade a and b) Large cystic spaces with mucous secretion lined by mucous and epidermoid cells and intermediate cells (a, 400 μ m; b, 200 μ m)
- 83. Intermediate-grade tumors have solid areas of epidermoid cells or squamous cells with intermediate basaloid cells. Cyst formation is seen but is less prominent than that observed in low-grade tumors. All cell types are present, but intermediate cells predominate. (Intermediate grade c and d) c - Well circumscribed lesion with fewer cystic spaces and more solid areas d - Intermediate grade, predominantly clear, and epidermoid cells (c, 4 mm; d, 200 μ m).
- 84. High-grade tumors consist of cells present as solid nests and cords of intermediate basaloid cells and epidermoid cells. Prominent nuclear pleomorphism and mitotic activity is noted. Cystic component is usually very less (<20%). Necrosis and perineural invasion may be present. High grade e and f) Solid tumors with the squamoid elements exhibiting anaplasia: Nuclear hyperchromatism, prominent nucleoli, and pleomorphism. Very rare mucous cells seen (e, 50 μ m; f, 70 μ m)
- 85. The treatment of mucoepidermoid carcinoma is predicated by the location, histopathologic grade, and clinical stage of the tumor. Early-stage tumors of the parotid often can be treated by subtotal parotidectomy with preservation of the facial nerve Advanced tumors may necessitate total removal of the parotid gland, with sacrifice of the facial nerve. For lowgrade neoplasms, only a modest margin of surrounding normal tissue may need to be removed. TREATMENT
- 86. High-grade or large tumors warrant wider resection, Neck dissection is indicated for patients with clinical evidence of metastatic disease . Postoperative radiation therapy also may be used for more aggressive tumors.
- 87. CONCLUSION Knowledge of anatomy and physiology of salivary glands is essential to distinctly identify various associated conditions and salivary gland pathologies. Precise anatomical knowledge is also essential to plan out our treatment strategies and alter the patient’s lifestyle for the better.
- 88. References: Clinical Periodontology By Carranza, 13th Edition. ESSENTIALS OF ORAL HISTOLOGY AND EMBRYOLOGY A Clinical Approach 3rd EDITION. Fundamentals of Oral Histology and Physiology. Orban's Oral Histology & Embryology (14th Edition). Shafers Textbook of Oral Pathology by Arya Rajendran, Shivapatha Sundaram 7th Edition. Salivary Glands Development, Adaptations and Disease. Essentials of Oral Pathology Swapan Kumar Purkait. Junqueira's Basic Histology Text and Atlas, 14th Edition.
- 89. Salivary Gland Tumours Monographs in Clinical Cytology by Jerzy Klijanienko, Philippe Vielh. Salivary Gland Disorders by Eugene N. Myers , Robert L. Salivary Gland Diseases Surgical and Medical Management Robert L. Witt, M.D. Glandular Epithelium Hanan Jafar. Netter’s Essential Histology. Part 1 by Ovalle Willam K., Nahirney Patrick C. Oral Anatomy, Histology and Embryology 5th Edition B. K. B. Berkovitz.
- 90. Alexander T Kessler and Alok A Bhatt:Review of the Major and Minor Salivary Glands, Part 1: Anatomy, Infectious, and Inflammatory Processes J Clin Imaging Sci. 2018; 8: 47. Salivary Diagnostics David T. Wong. Victor Shing Howe To, Jimmy Yu Wai Chan, Raymond K. Y. Tsang, and William I. Wei.Review of Salivary Gland Neoplasms: 2012,872982,6. A.S. Tucker. / Seminars in Cell & Developmental Biology 18 (2007) 237–244.
