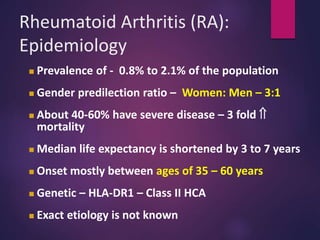
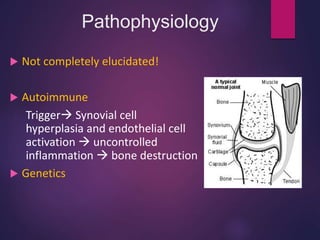
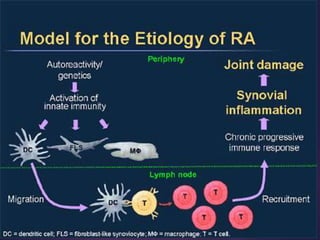
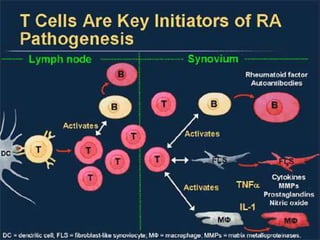
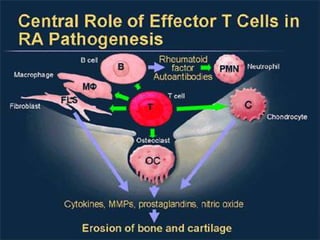
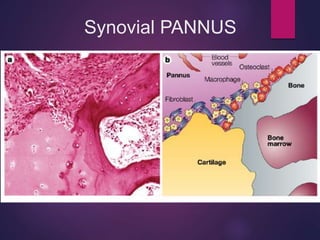
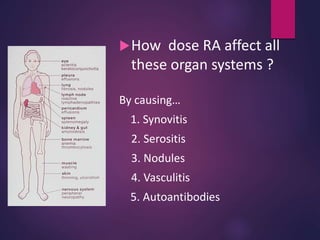
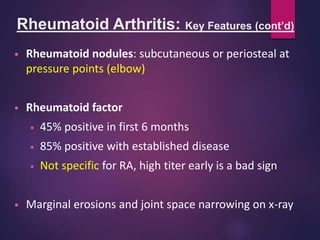
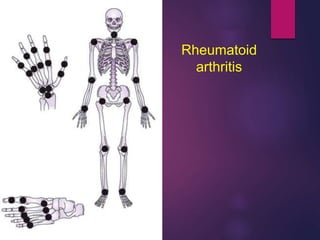
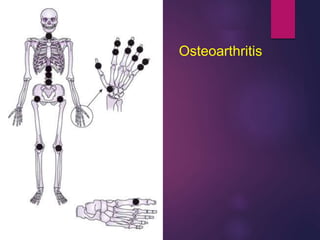
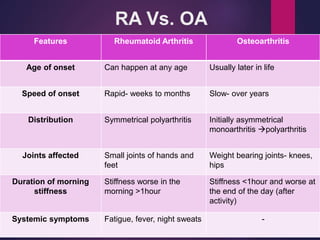
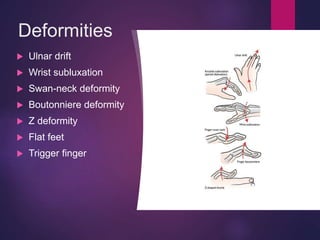
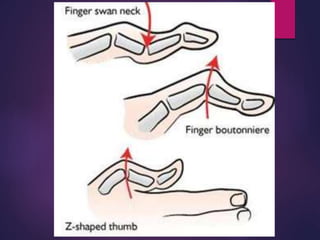
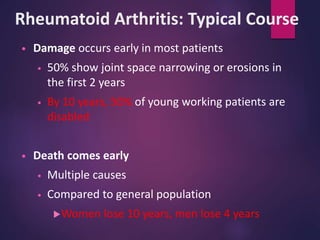
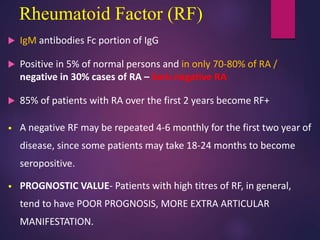
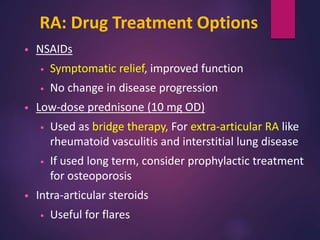
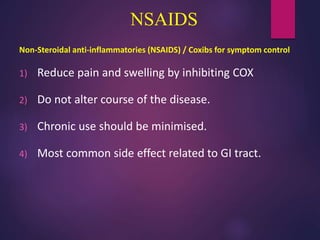
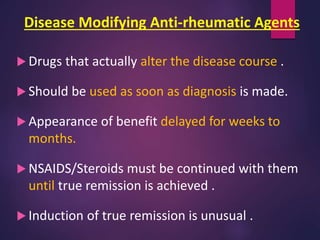
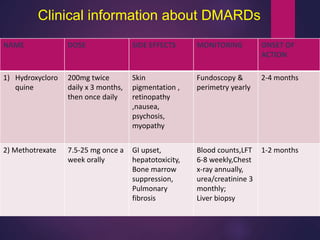
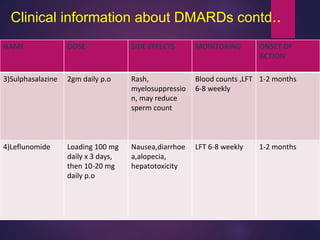
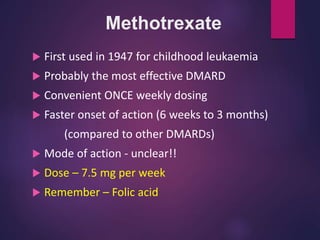
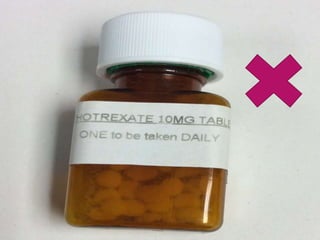
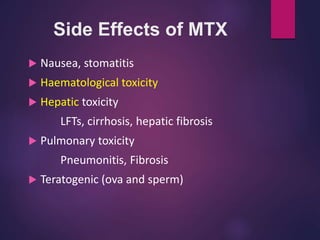
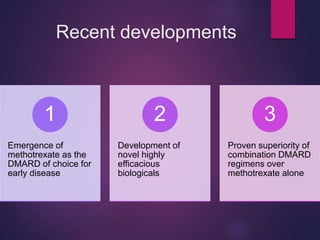
Rheumatoid arthritis is a chronic inflammatory disease that affects about 0.8-2.1% of the population. It is characterized by symmetric inflammation of joints that can lead to joint damage over time. While the exact cause is unknown, genetics and autoimmunity are thought to play a role. Treatment involves medications like NSAIDs for symptom relief and DMARDs like methotrexate to slow disease progression. Left untreated, rheumatoid arthritis can cause pain, deformities, and loss of function in joints as well as increase the risk of other health issues.