This document provides information on retinal detachment including:
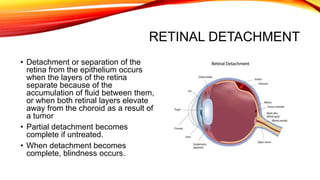
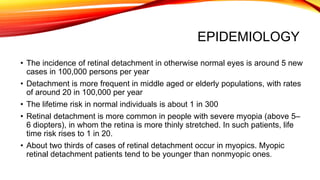
1. It describes the three main types of retinal detachment - rhegmatogenous, tractional, and exudative - and their causes.
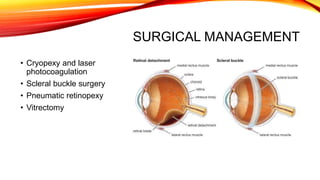
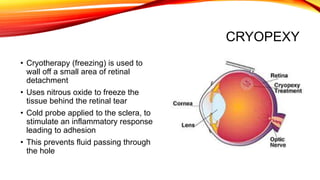
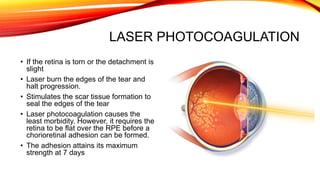
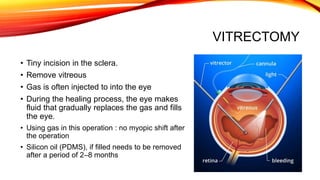
2. Risk factors, clinical manifestations, diagnosis, and surgical management options like cryopexy, laser photocoagulation, scleral buckling, pneumatic retinopexy, and vitrectomy are summarized.
3. Post-operative care involves positioning, monitoring for complications, restricting activities that raise intraocular pressure, and reporting any new visual issues or pain immediately.