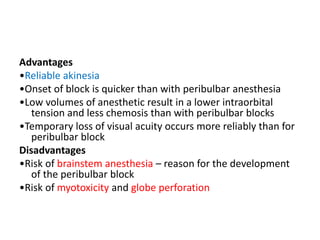
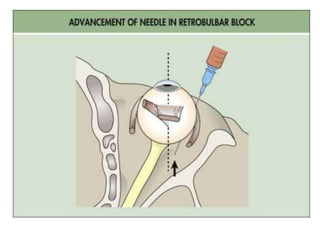
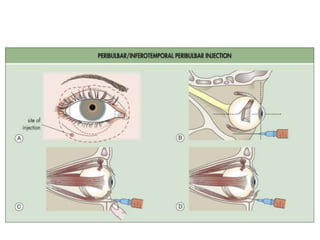
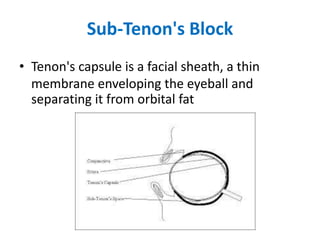
Local and topical anesthesia are now the norm for cataract surgery, with only 2% of patients requiring general anesthesia. Topical anesthesia involves applying local anesthetic eye drops. Retrobulbar and peribulbar blocks involve injecting local anesthetic behind or around the eye muscle cone. Sub-Tenon's block involves injecting local anesthetic into the space beneath the outer protective layer of the eye. While topical and local blocks provide anesthesia, general anesthesia allows for a quiet, immobile patient but is more expensive and risky.