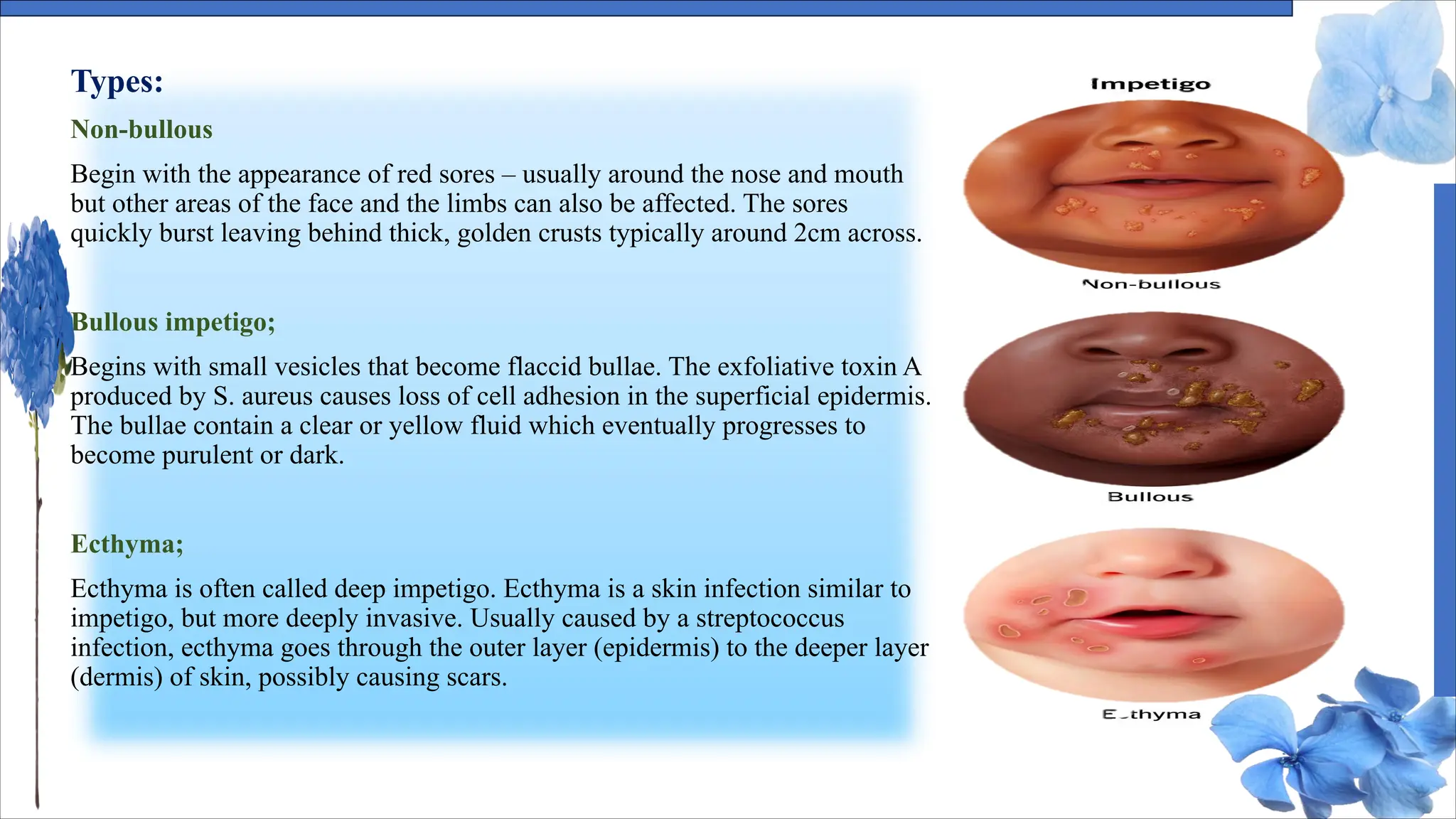
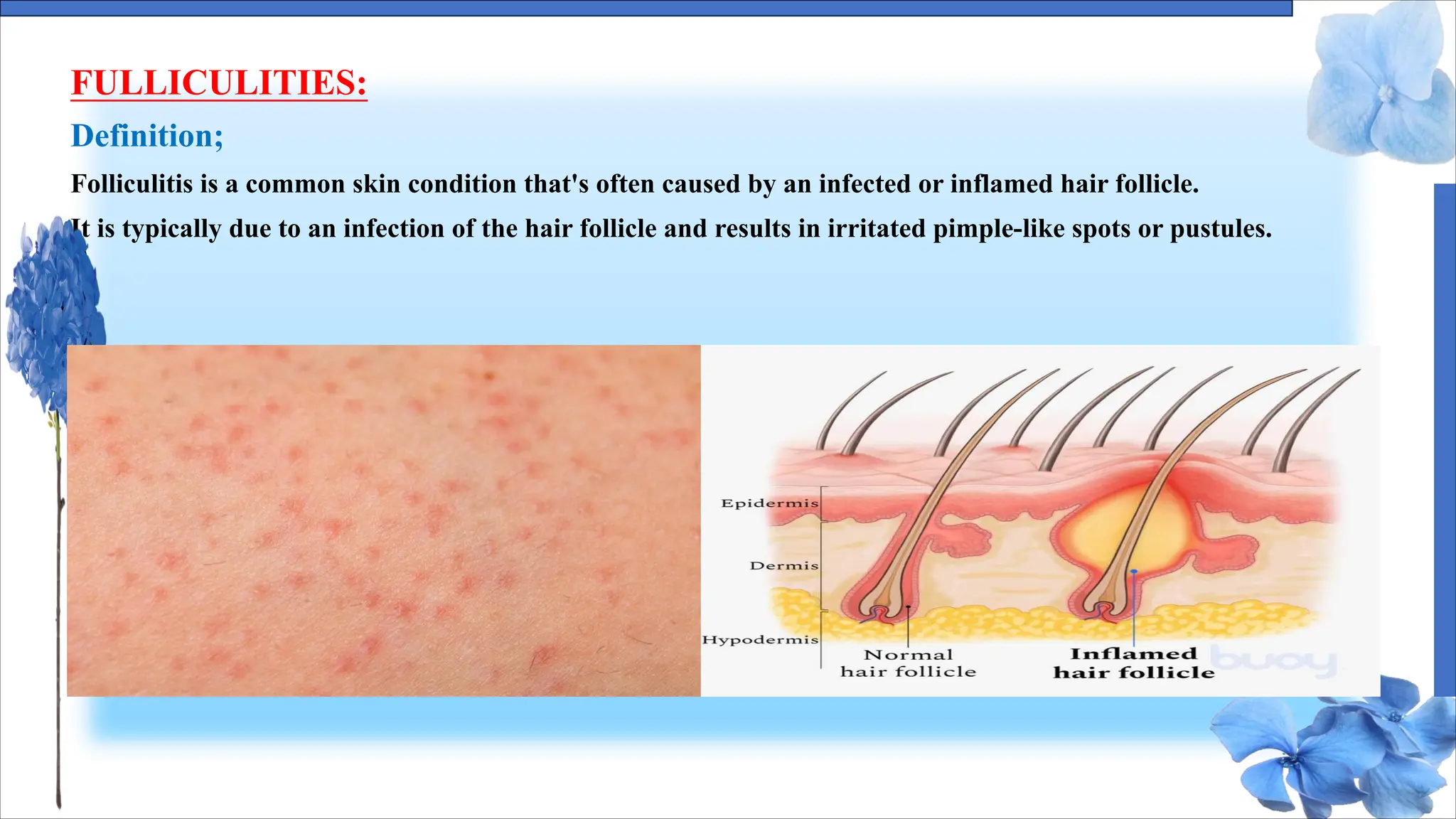
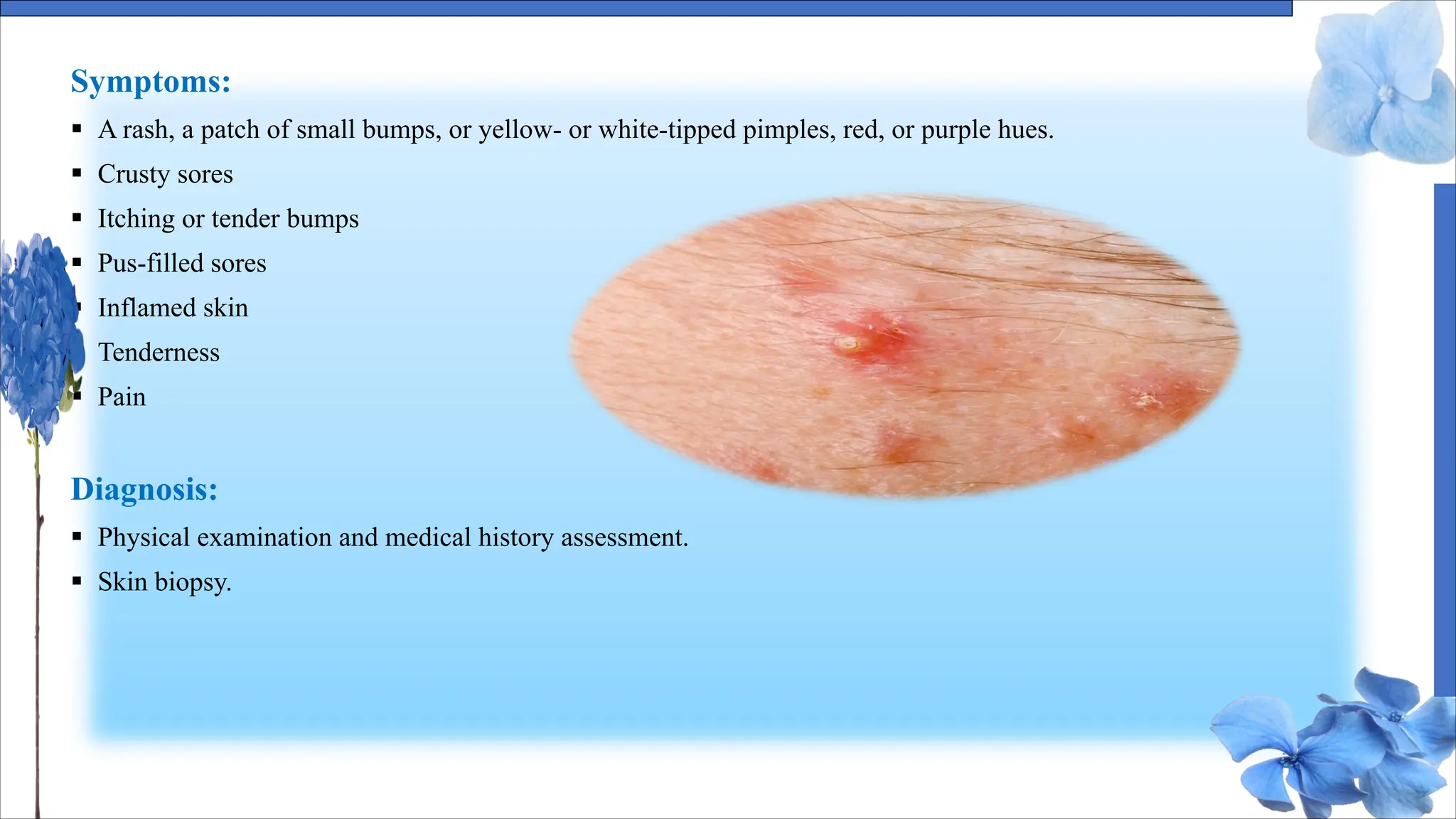
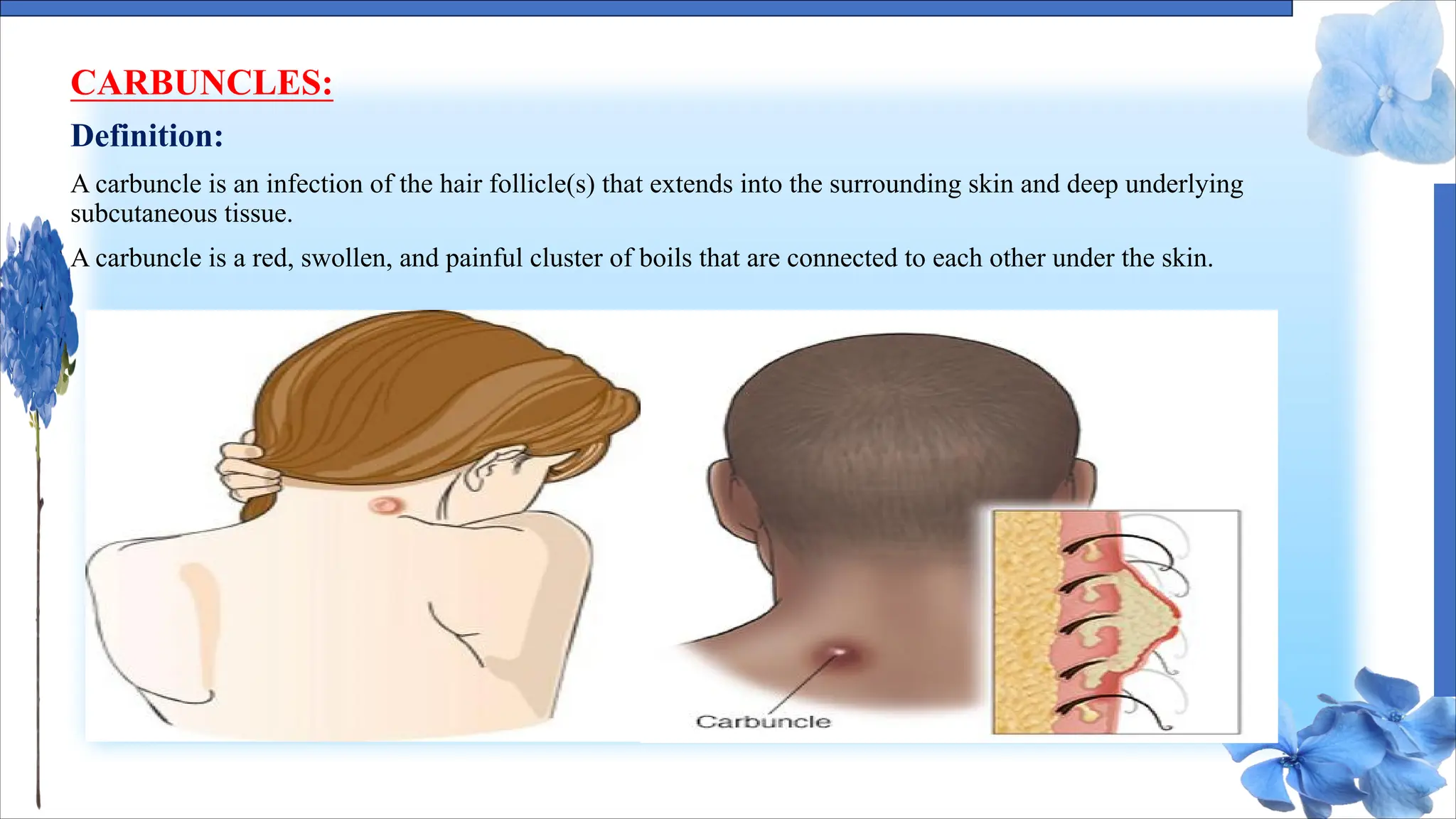
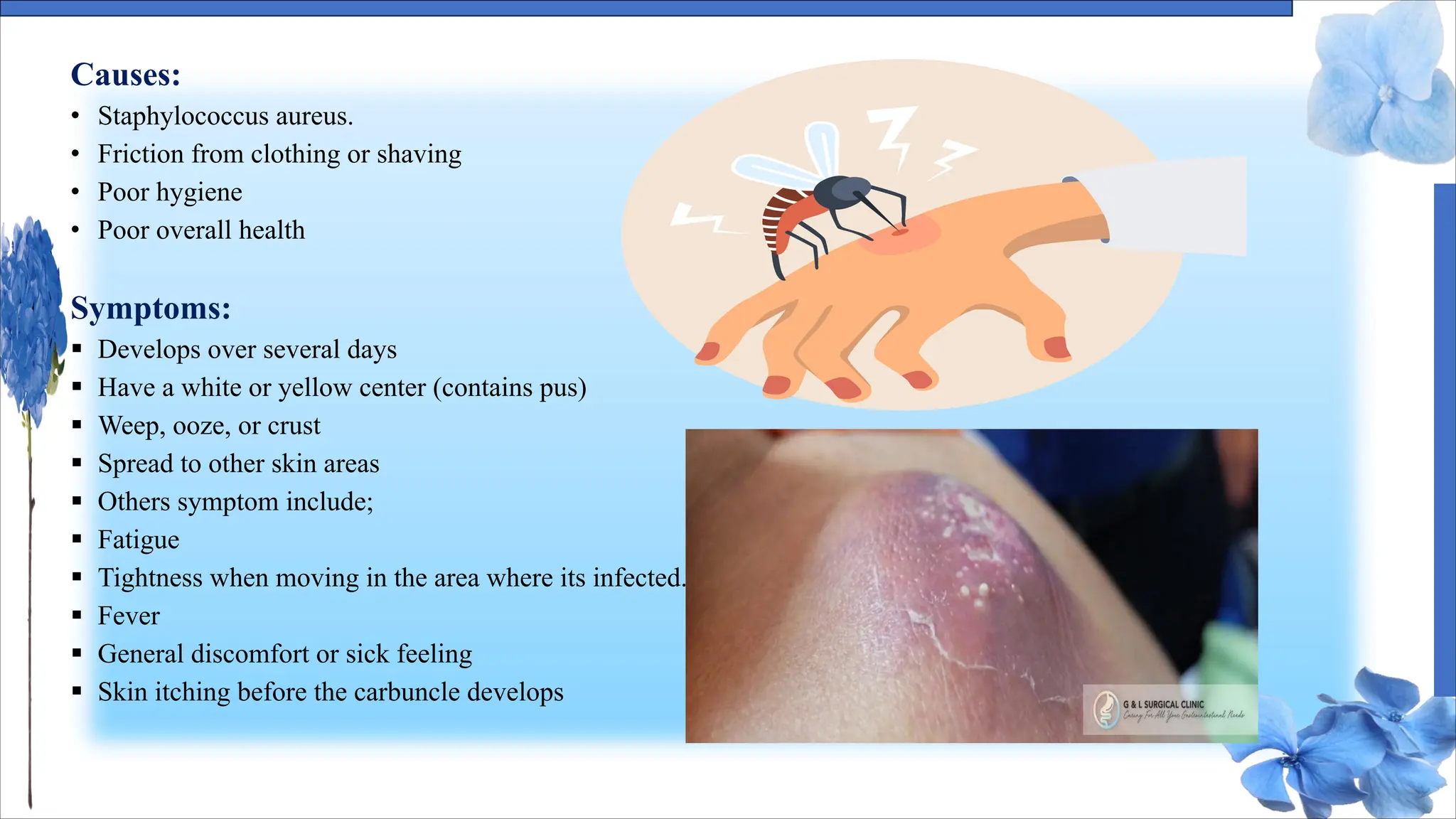
The document discusses various skin conditions including pyoderma, impetigo, folliculitis, furuncles, and carbuncles, detailing their definitions, causes, symptoms, diagnosis, and management strategies. Pyoderma gangrenosum causes painful ulcers, while impetigo is a contagious infection characterized by sores. Other conditions such as folliculitis and furuncles are associated with infected hair follicles, with specific treatments ranging from antibiotics to lifestyle changes.