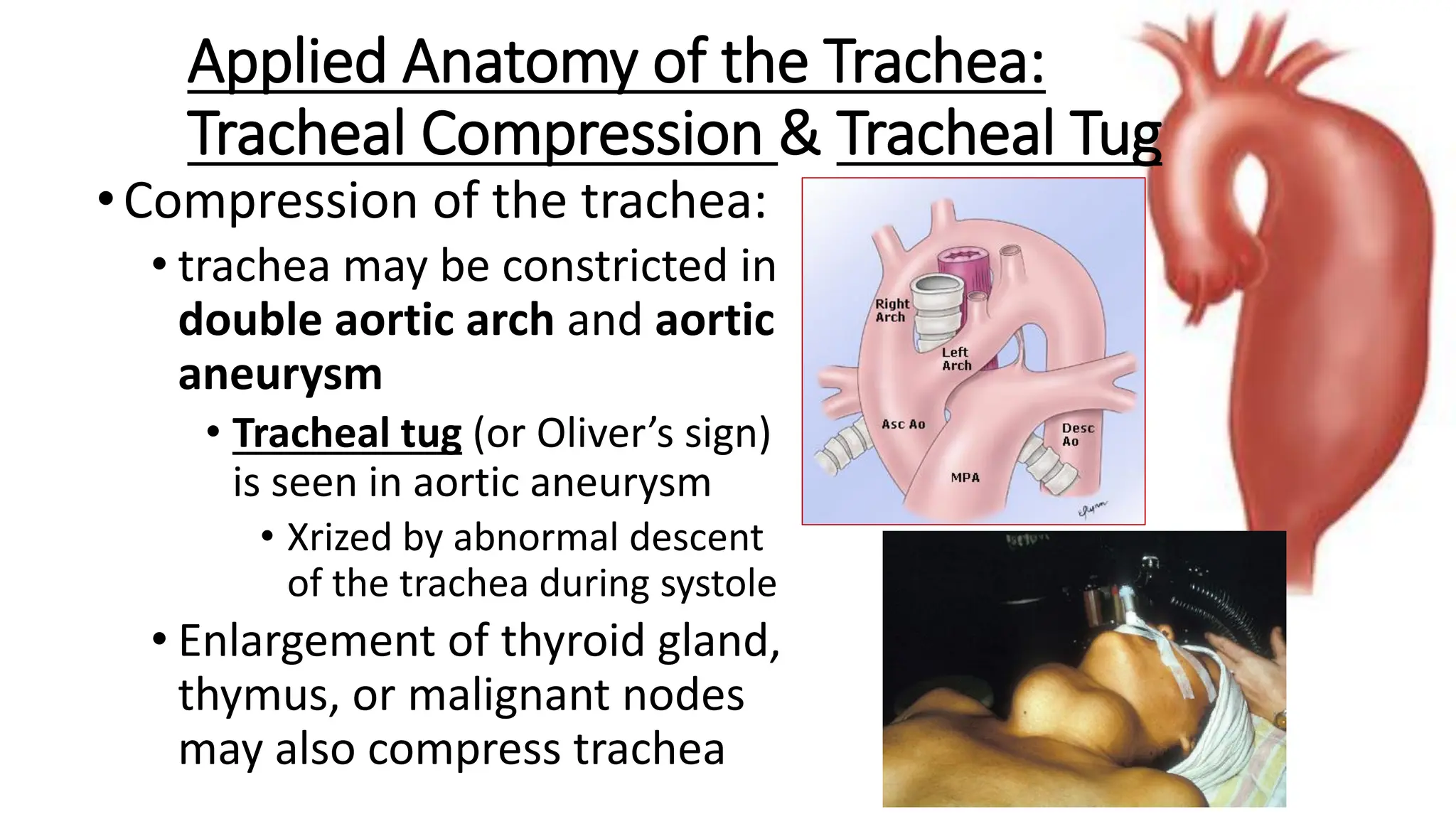
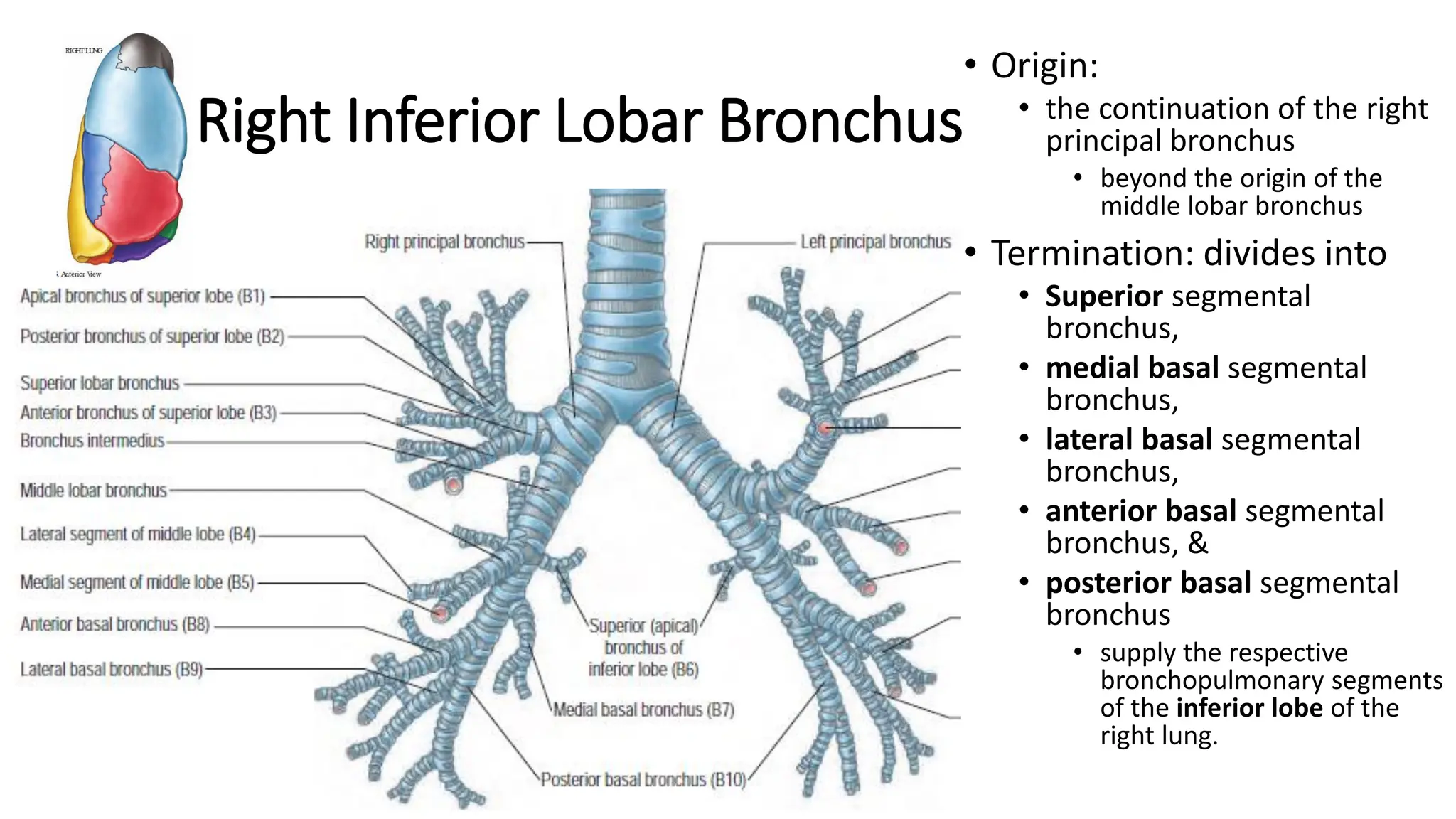
The trachea is a cartilaginous tube that connects the larynx to the bronchi. It has 16-20 C-shaped cartilage rings. The right principal bronchus is shorter, wider, and more vertical than the left. The left principal bronchus is narrower, longer, and more horizontal. It lies closer to the aorta and esophagus. Secondary bronchi arise from the principal bronchi and supply the lobes. The right lung has 3 lobar bronchi while the left has 2. The right superior lobar bronchus is the only one that enters above the pulmonary artery.