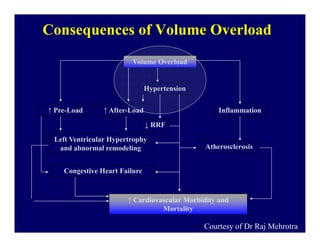
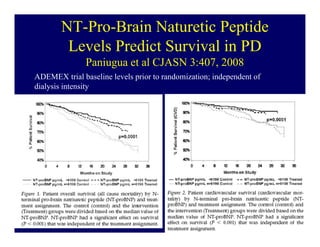
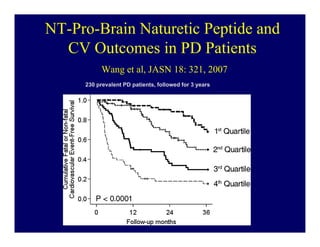
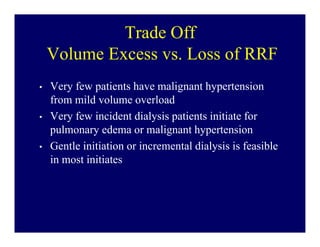
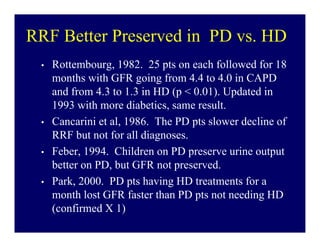
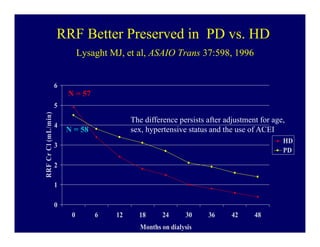
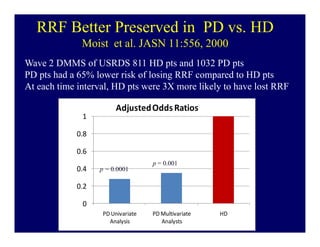
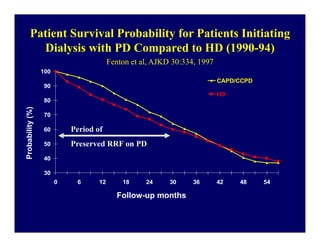
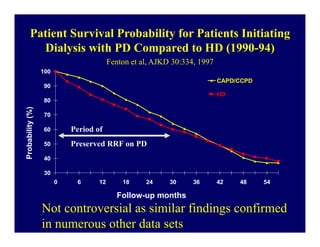
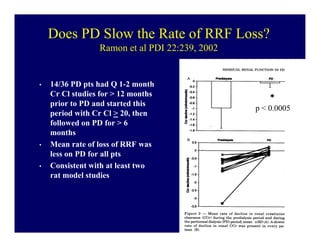
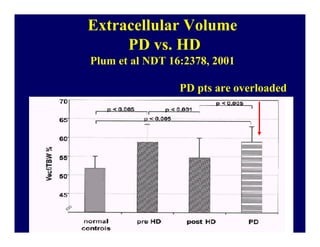
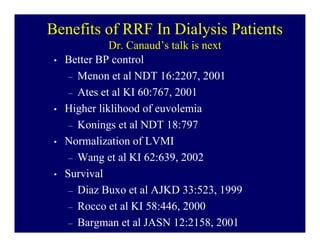
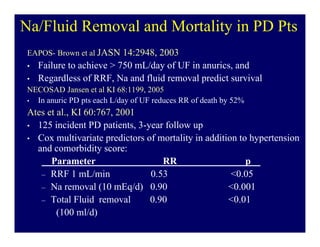
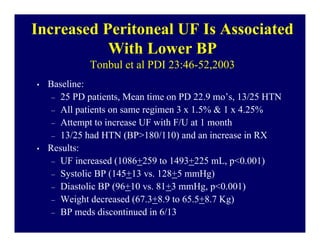
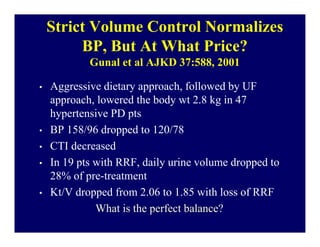
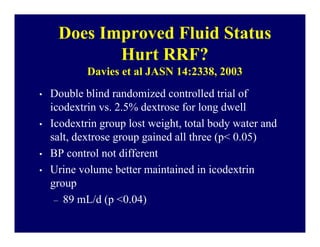
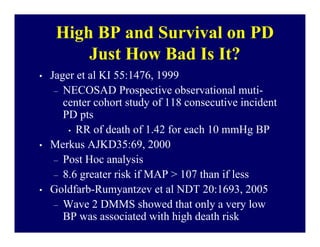
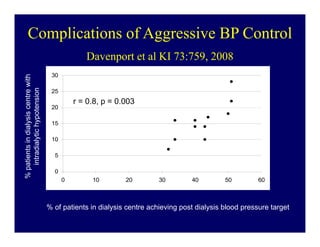
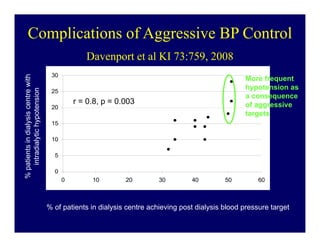
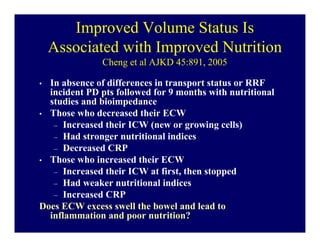
This document summarizes a program on residual renal function (RRF). The first presentation is by Thomas Golper on whether volume overloaded dialysis patients should be aggressively ultrafiltered to dry weight even if it causes RRF to decline. The second presentation is by Bernard Canaud on how RRF improves patient outcomes. The third presentation is by Isaac Teitelbaum on how to preserve RRF in dialysis patients. The program aims to discuss the tradeoffs between managing volume status and preserving RRF in dialysis care.