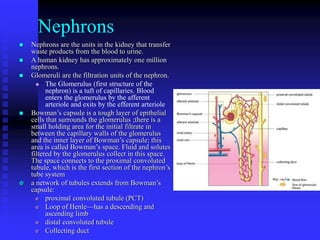
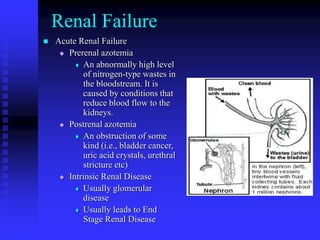
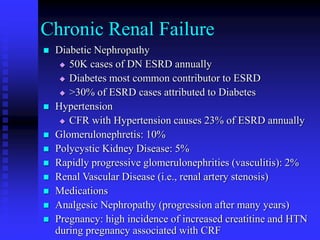
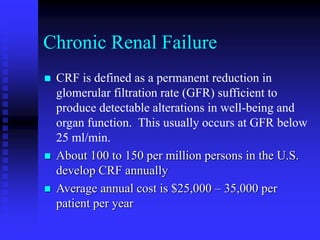
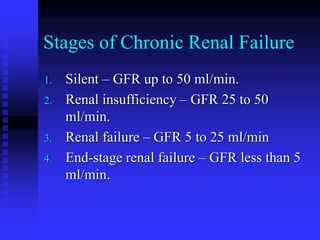
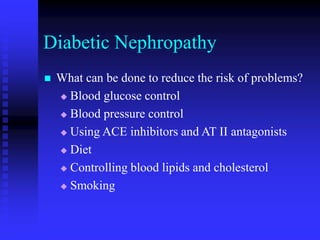
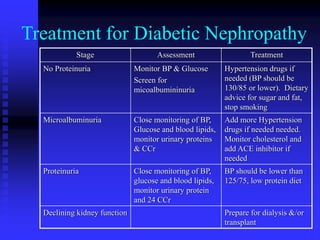
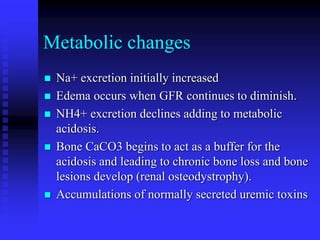
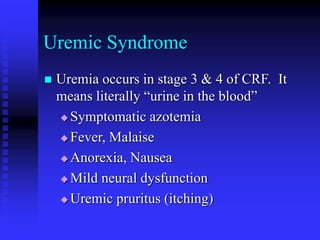
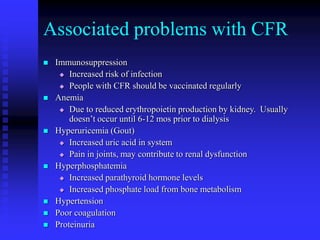
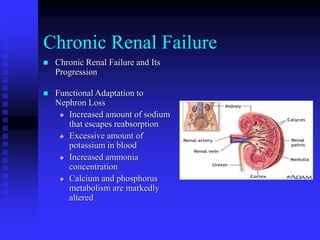
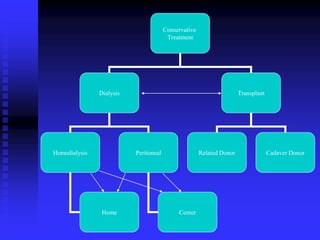
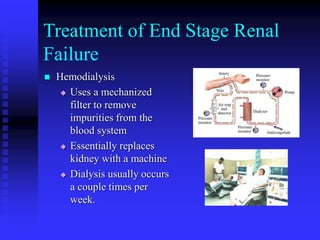
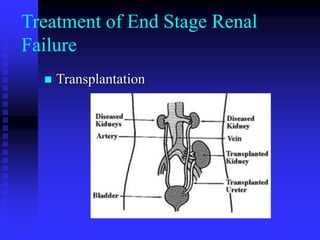
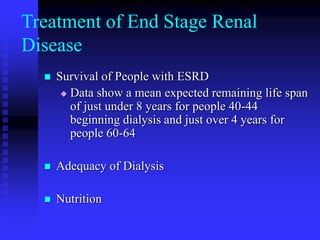
The document discusses chronic renal failure, including its causes, stages, symptoms, and treatment options. It defines chronic renal failure as permanent kidney dysfunction resulting in detectable health issues. Common causes include diabetes, hypertension, and glomerulonephritis. Treatment may involve managing symptoms conservatively or through dialysis and transplantation to replace kidney function. The goals of treatment are to delay disease progression, manage complications, and improve quality of life.