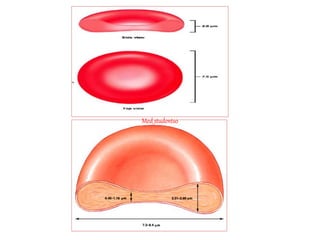
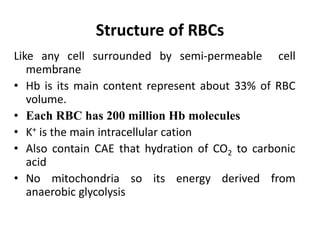
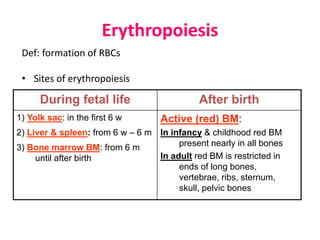
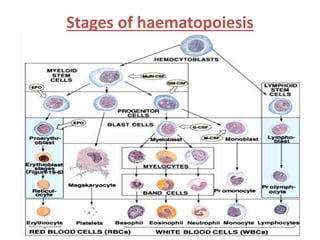
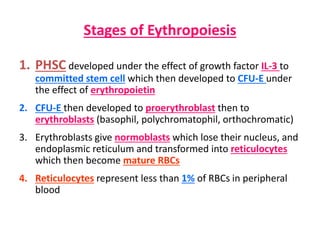
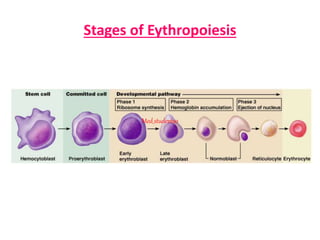
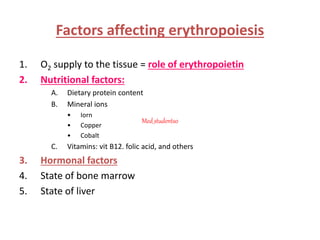
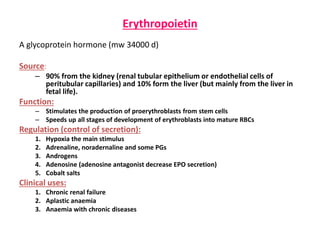
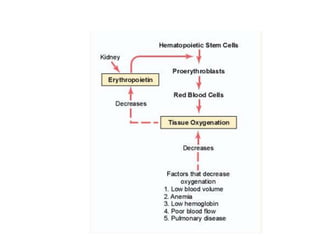
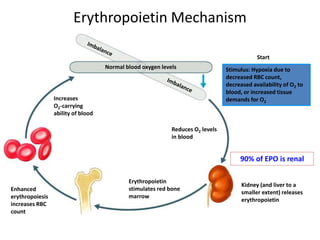
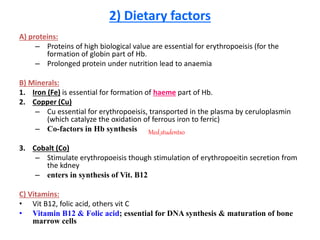
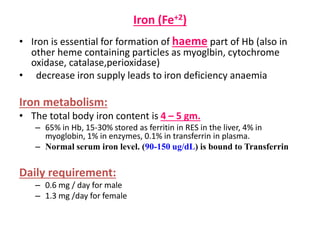
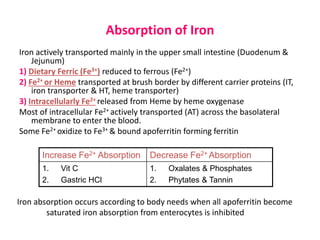
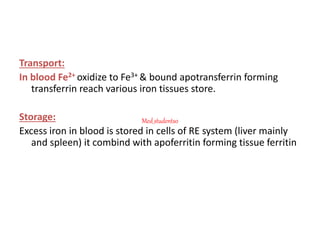
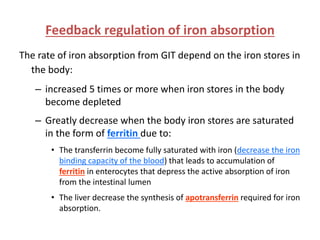
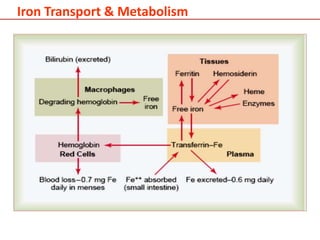
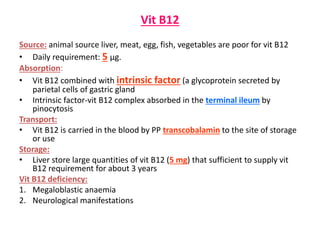
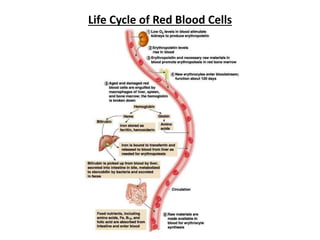
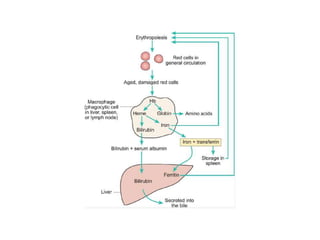
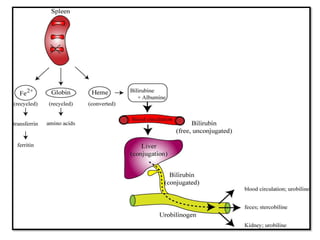
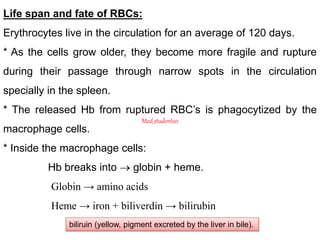
The document provides an overview of red blood cells (RBCs), detailing their structure, formation processes (erythropoiesis), lifespan, and factors affecting their production. It emphasizes the role of erythropoietin, nutrition, and hormonal influences in RBC development, as well as iron and vitamin requirements for their maturation. Additionally, it outlines the life cycle of RBCs and their breakdown process in the body.