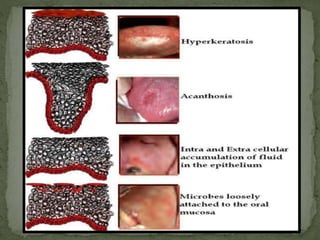
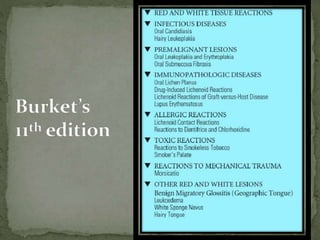
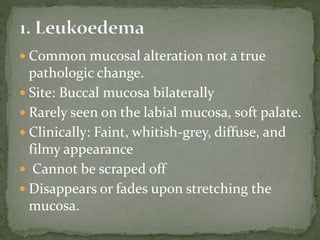
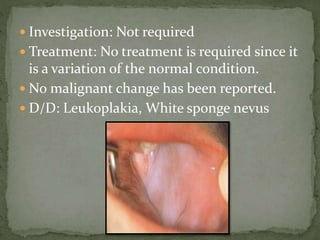
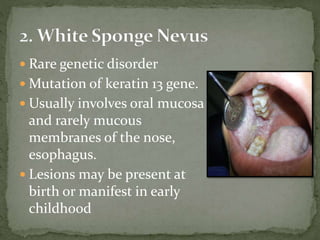
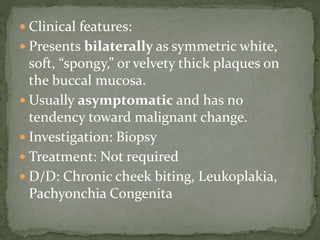
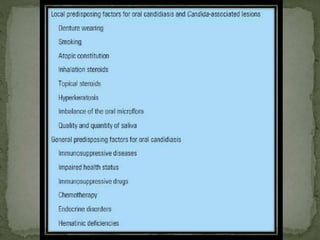
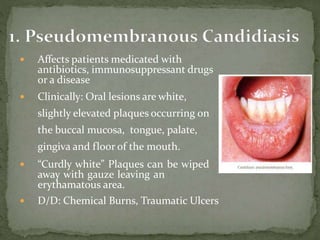
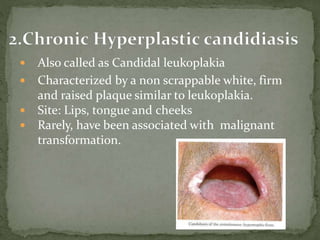
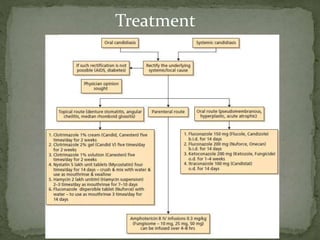
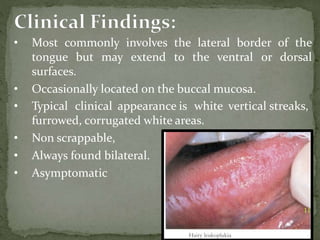
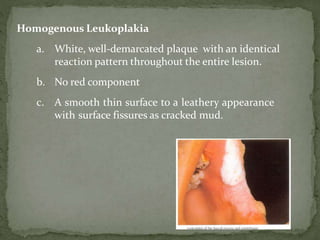
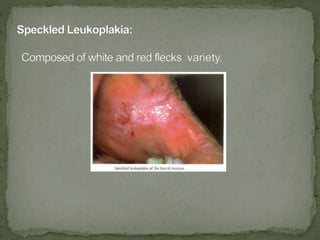
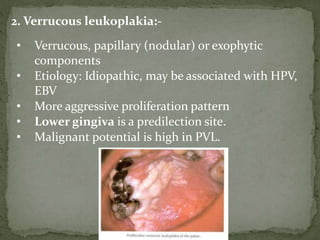
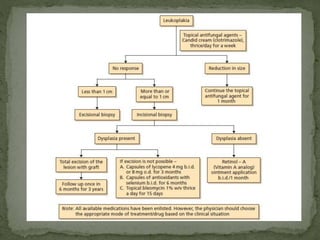
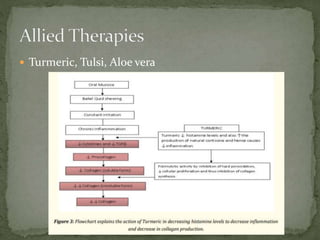
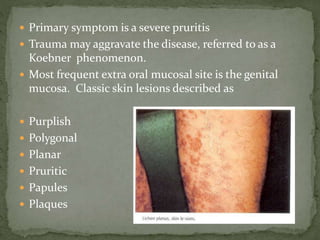
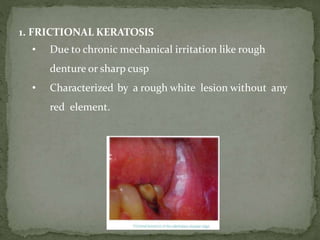
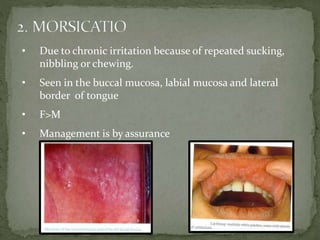
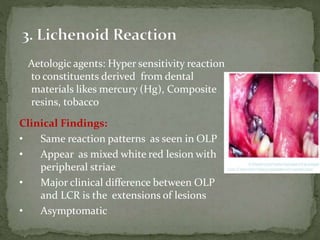
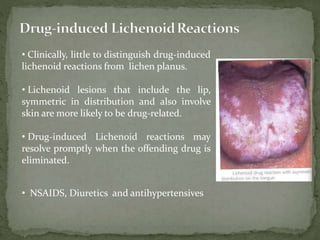
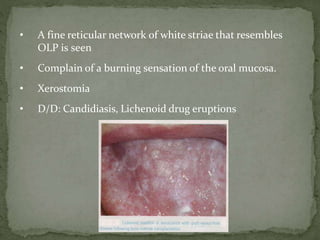
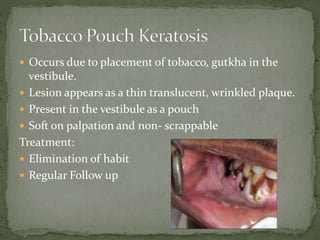
The document discusses the clinical presentation and management of oral mucosal lesions. It begins by explaining that the mucosa may appear white due to factors like blood vessel concentration, keratinization, and melanin levels. It then covers common white lesions like leukoedema and white sponge nevus. The document also discusses premalignant and malignant conditions, infectious diseases, allergic reactions and mechanical trauma that can cause white lesions. Treatment options are provided for many of the conditions.