Tongue
Floor of mouth
Buccal mucosa
Gingiva
RISK FACTORS:
Tobacco chewing/smoking
2. Alcohol consumption
3. Sun exposure (lips)
4. HPV infection
5. Plummer-Vinson syndrome
6. Oral submucous fibrosis
7. Leukoplakia/erythroplakia
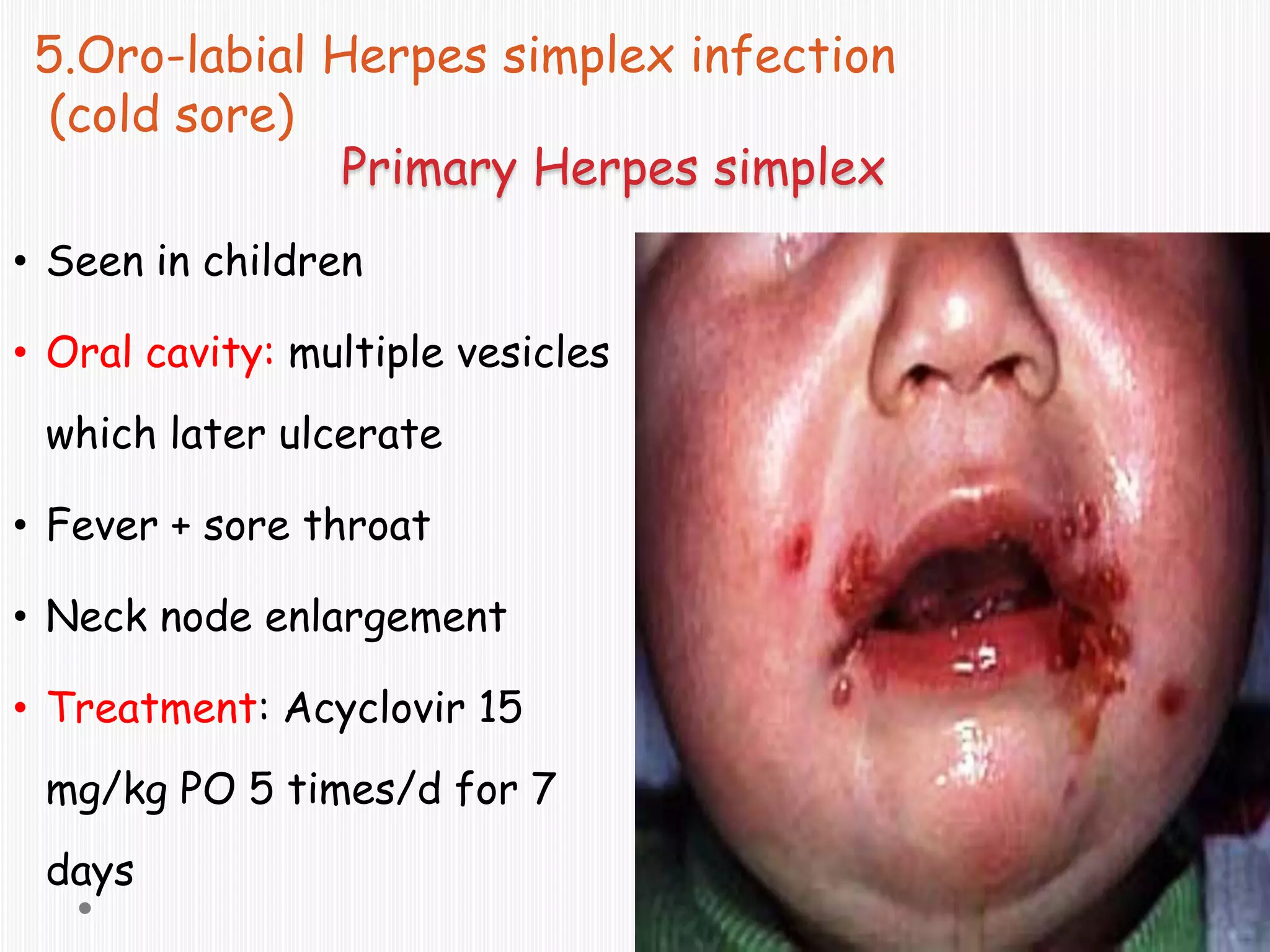
This document discusses common oral conditions including aphthous ulcers, oral candidiasis, Vincent's infection, oral herpes, leukoplakia, erythroplakia, and oral cancer. It describes the anatomy of the oral cavity, signs and symptoms, causes