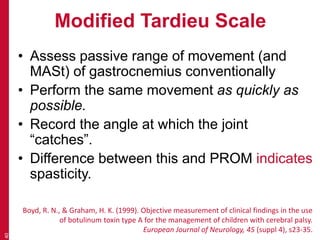
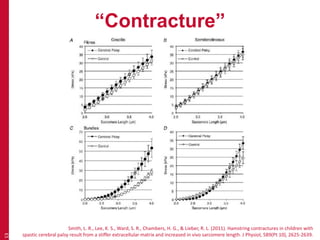
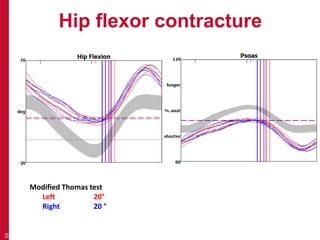
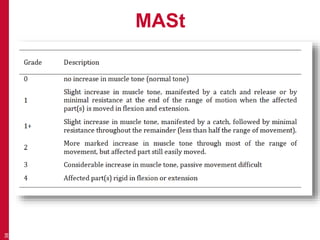
This document discusses contractures and spasticity in individuals with neuromuscular impairments. It defines contracture as a shortening of the muscle belly through atrophy or loss of fascicles and increased muscle stiffness from an enlarged extracellular matrix. Spasticity is described as a velocity-dependent increase in muscle tone due to hyperreflexia of the stretch reflexes following an upper motor neuron lesion. The Modified Ashworth Scale and Modified Tardieu Scale are presented as clinical measures of tone and spasticity, respectively, with the latter assessing the angle at which a joint catches during a rapid stretch.
![Pandayan, 2005
“disordered sensori-motor control, resulting
from an upper motor neuron lesion,
presenting as intermittent or sustained
involuntary activation of muscle”
28
Pandyan, A. D., Gregoric, M., Barnes, M. P., Wood, D., Van Wijck, F., Burridge, J., . . .
Johnson, G. R. (2005). Spasticity: clinical perceptions, neurological realities and
meaningful measurement. [Review]. Disabil Rehabil, 27(1-2), 2-6.](https://image.slidesharecdn.com/recognisingfeaturescontractureandspasticity-140516103111-phpapp02/85/Recognising-features-contracture-and-spasticity-28-320.jpg)
![NIH Taskforce on Childhood
Motor Disorders
Tone
[resistance to] “passive stretch while the patient
is attempting to maintain a relaxed state of
muscle activity ”
32
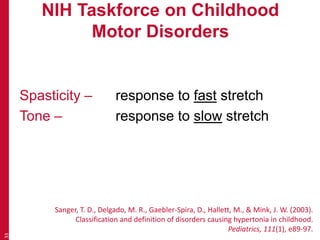
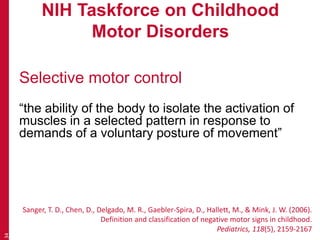
Sanger, T. D., Delgado, M. R., Gaebler-Spira, D., Hallett, M., & Mink, J. W. (2003).
Classification and definition of disorders causing hypertonia in childhood.
Pediatrics, 111(1), e89-97.](https://image.slidesharecdn.com/recognisingfeaturescontractureandspasticity-140516103111-phpapp02/85/Recognising-features-contracture-and-spasticity-32-320.jpg)
![Spasticity
Tardieu (1954)
• Complex
• Impractical
• In French!
39
Tardieu, G., Shentoub, S., & Delarue, R. (1954).
[Research on a technic for measurement of spasticity].
Rev Neurol (Paris), 91(2), 143-144.](https://image.slidesharecdn.com/recognisingfeaturescontractureandspasticity-140516103111-phpapp02/85/Recognising-features-contracture-and-spasticity-39-320.jpg)