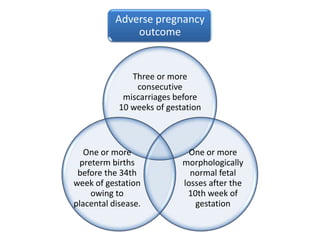
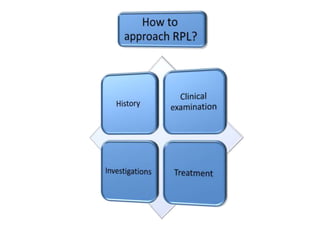
1) Recurrent miscarriage, defined as the loss of three or more consecutive pregnancies, affects 1% of couples trying to conceive.
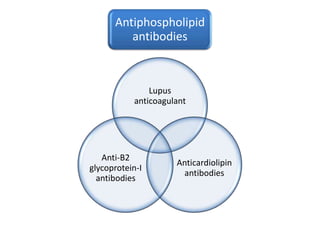
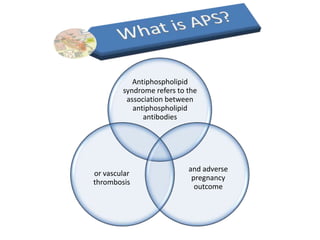
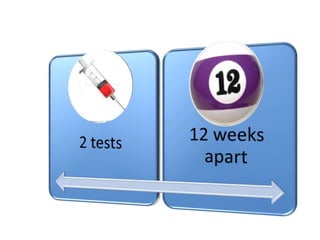
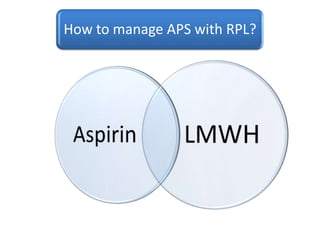
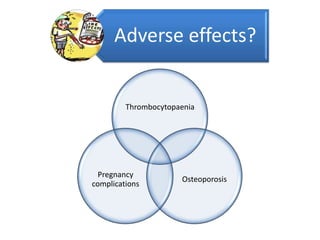
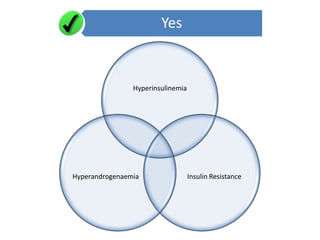
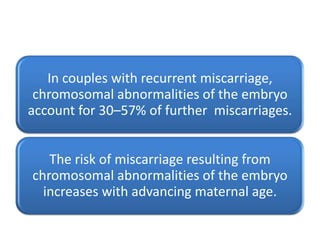
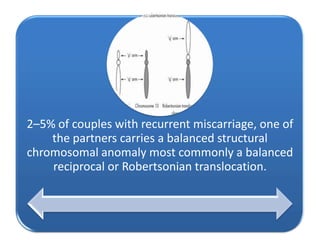
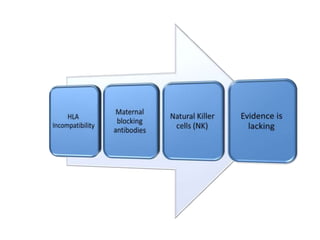
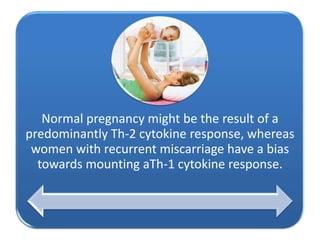
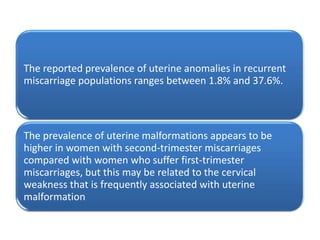
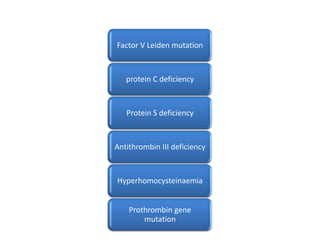
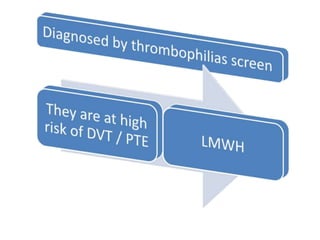
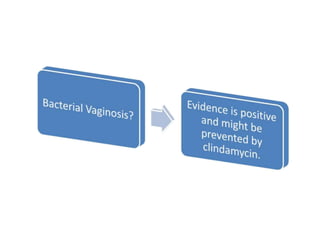
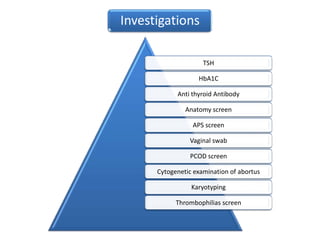
2) Risk factors for recurrent pregnancy loss (RPL) include antiphospholipid syndrome, genetic factors, anatomical factors, endocrine factors, immune factors, infective agents, inherited thrombophilic defects, smoking, caffeine, alcohol, lupus anticoagulant, and anti-cardiolipin antibodies.
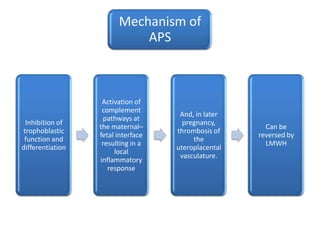
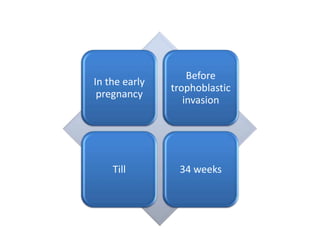
3) Antiphospholipid antibodies are present in 15% of women with RPL, compared to less than 2% of women with a normal obstetric history, and live birth rates without treatment can be as low as 10%