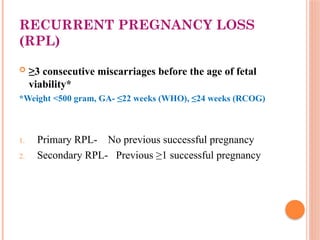
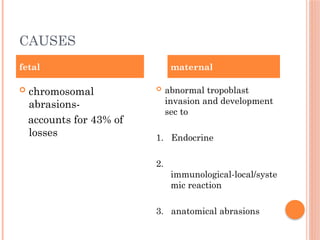
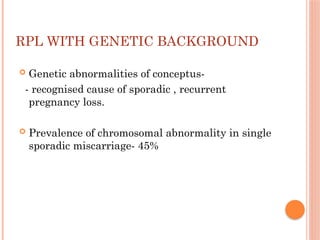
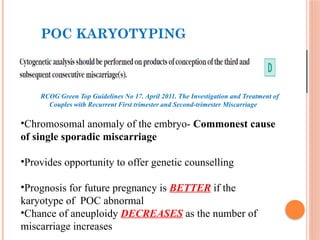
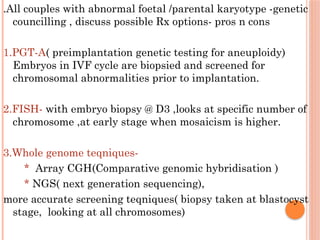
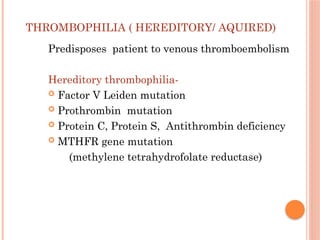
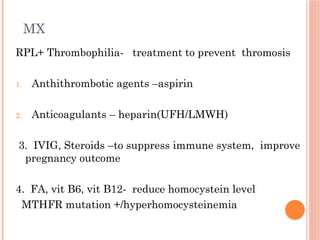
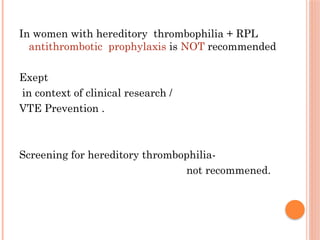
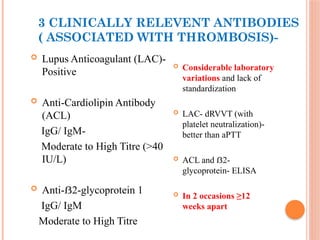
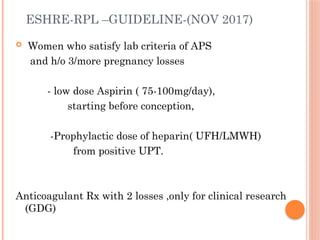
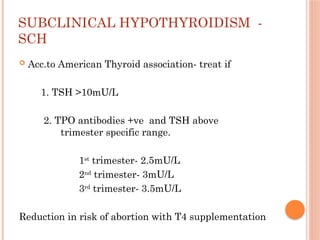
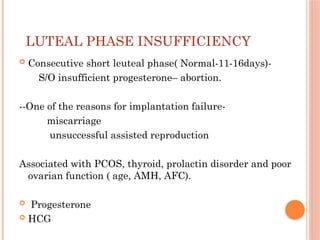
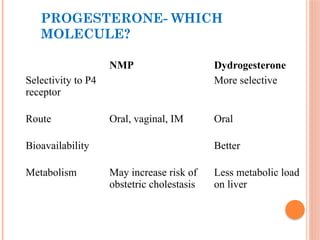
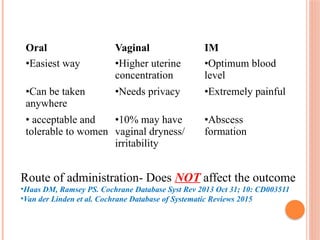
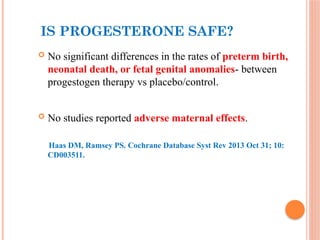
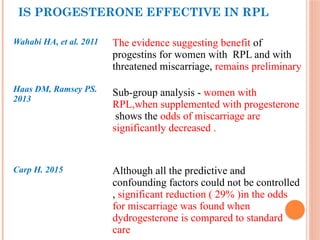
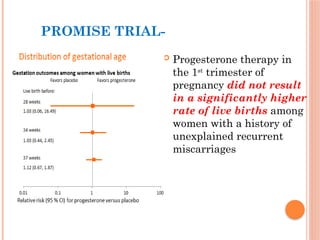
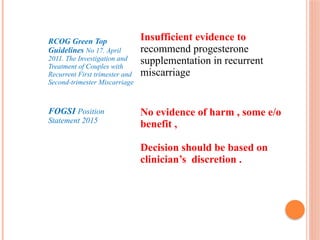
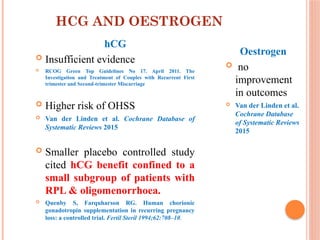
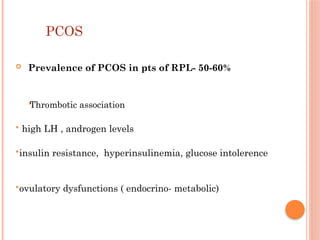
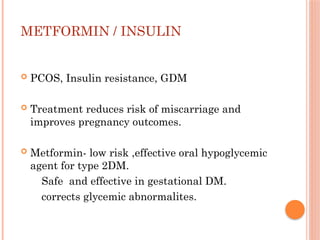
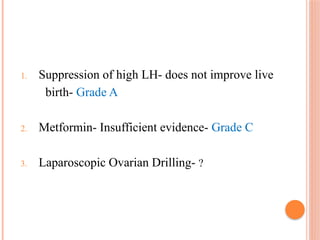
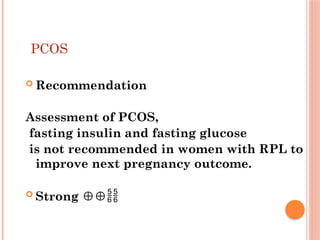
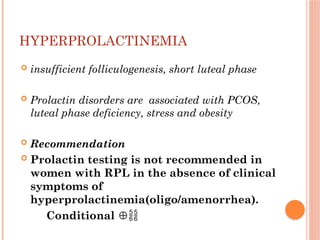
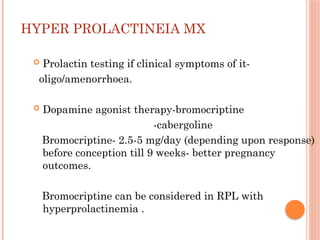
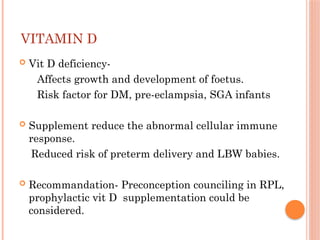
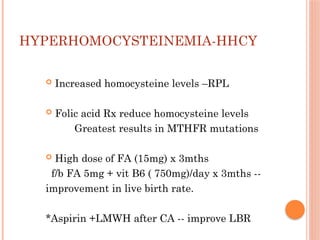
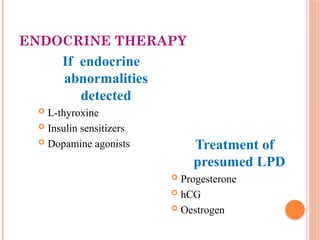
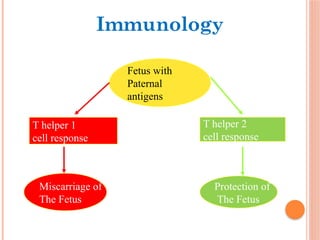
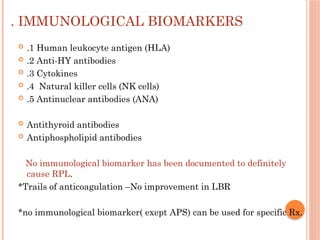
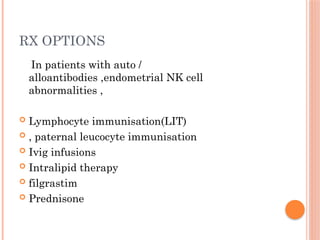
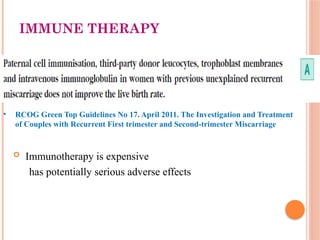
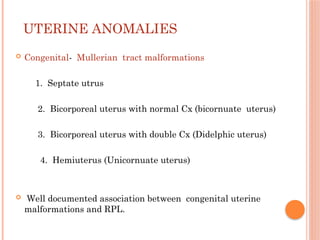
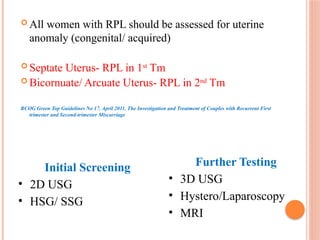
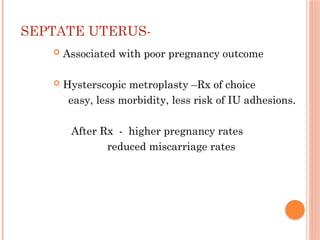
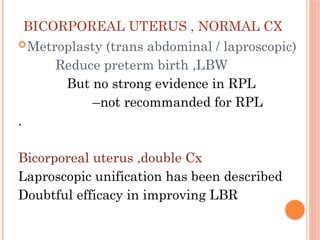
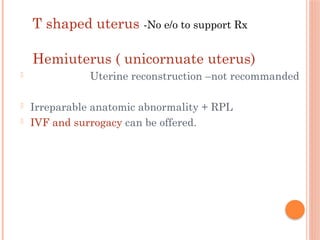
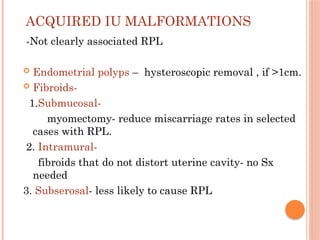
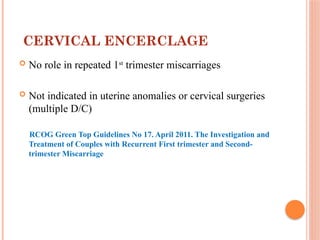
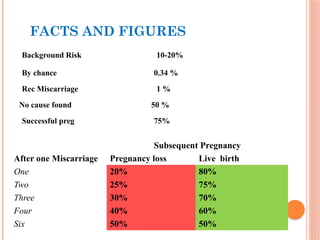
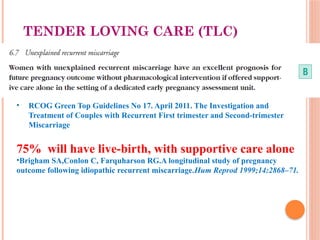
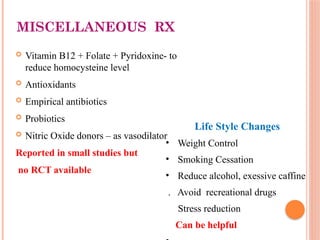
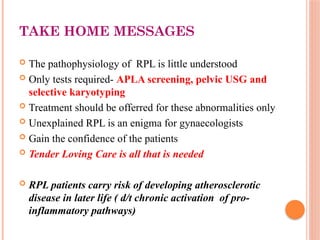
The document addresses the complex management of recurrent pregnancy loss (RPL), defining types of RPL, potential causes, and treatment recommendations for affected couples. It emphasizes the importance of genetic counseling, investigation of underlying conditions like thrombophilia, and the role of hormonal treatments such as progesterone, while discussing various therapeutic approaches. In addition, it highlights the significance of assessing uterine anomalies and the impact of maternal age on miscarriage rates.