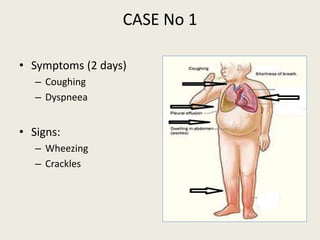
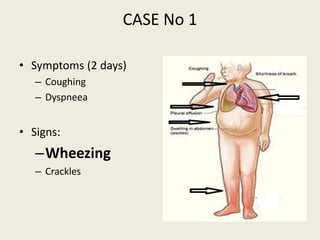
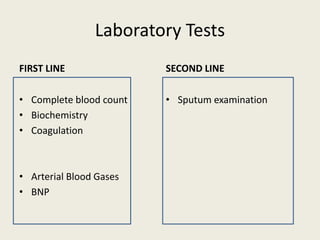
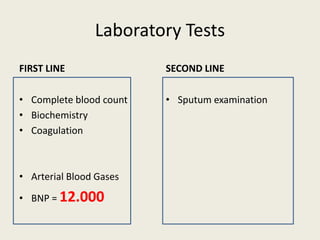
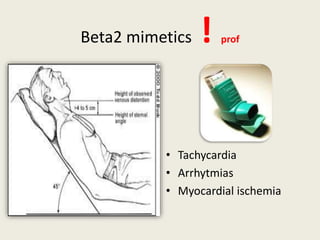
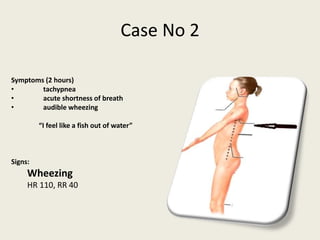
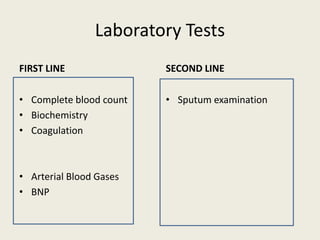
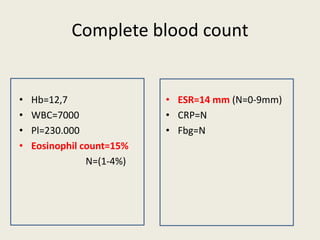
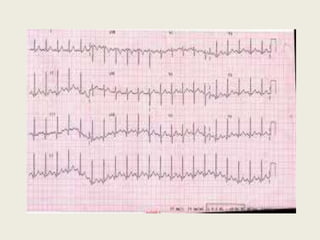
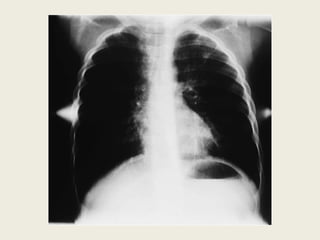
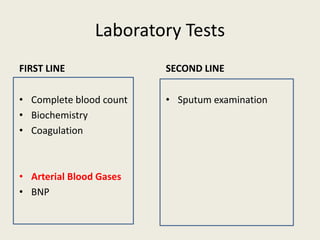
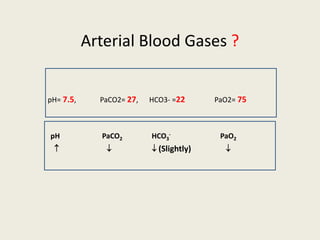
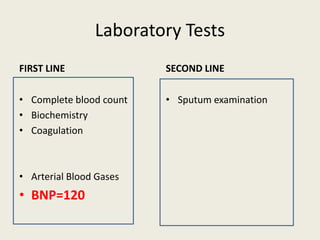
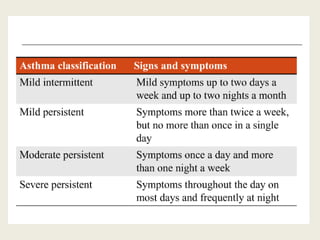
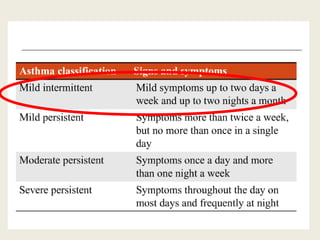
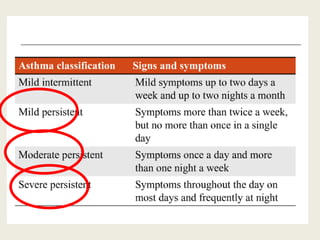
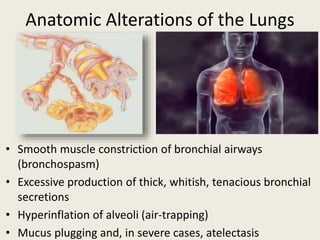
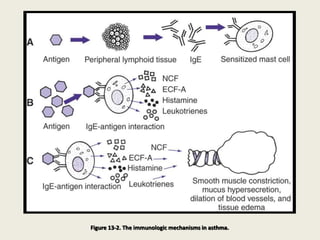
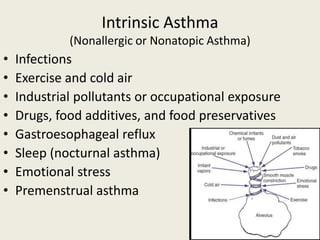
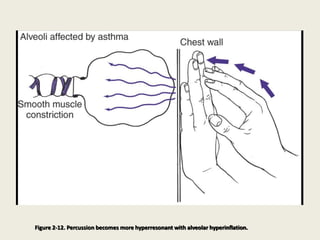
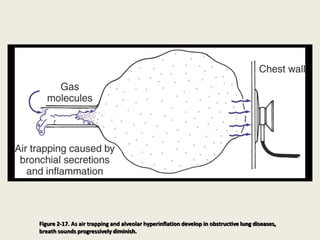
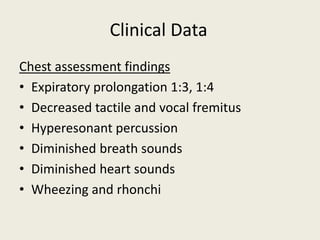
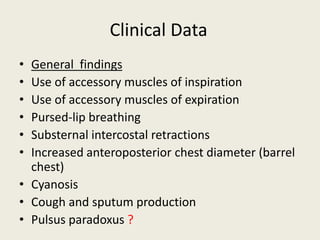
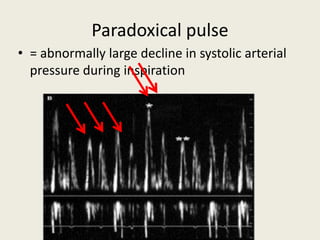
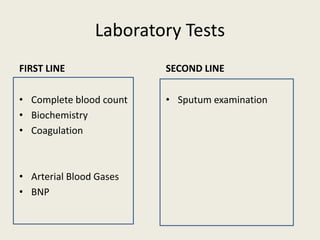
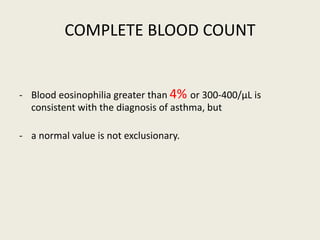
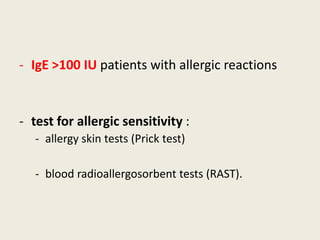
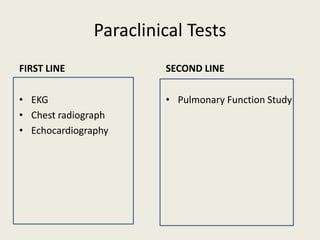
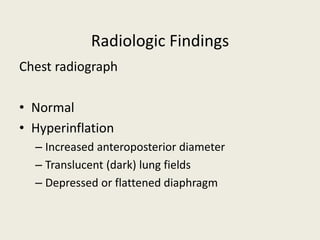
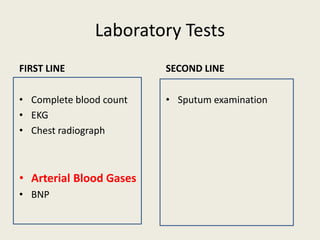
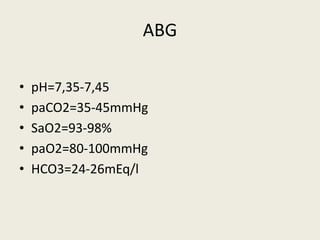
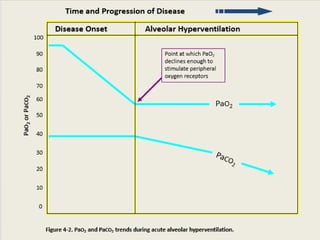
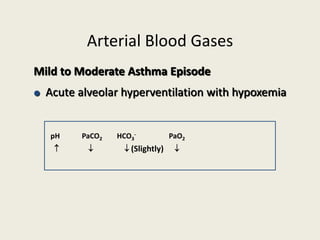
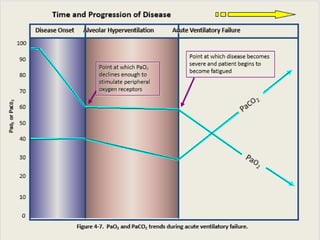
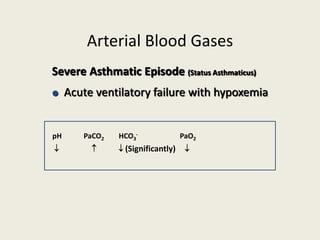
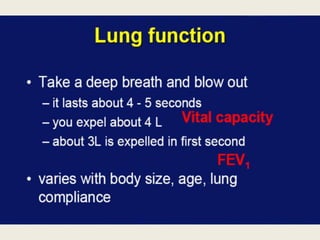
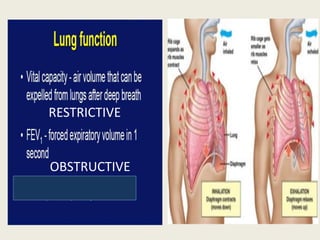
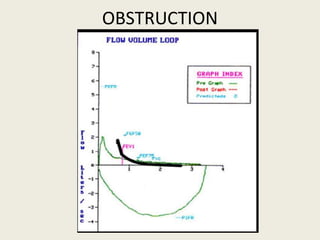
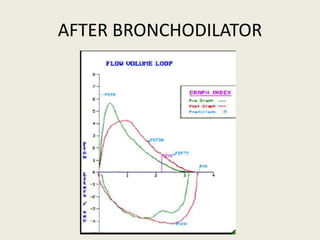
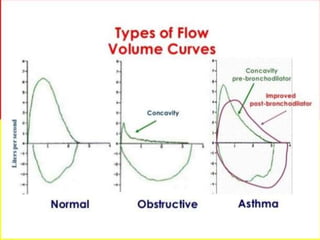
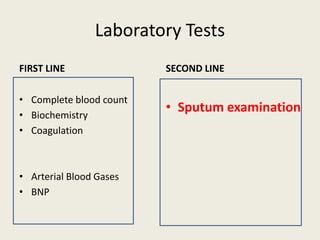
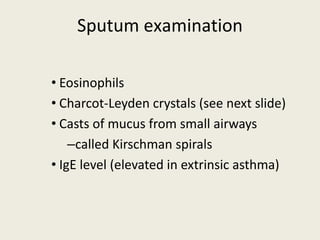
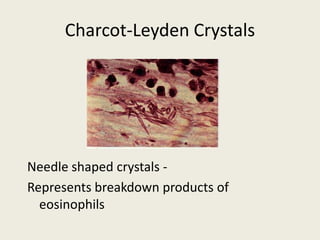
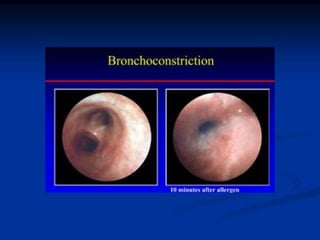
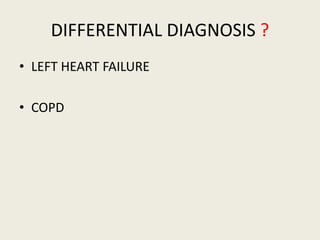
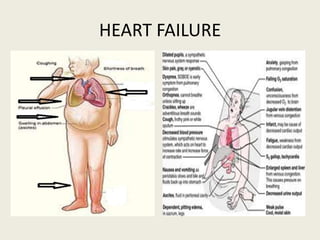
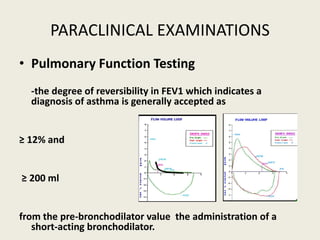
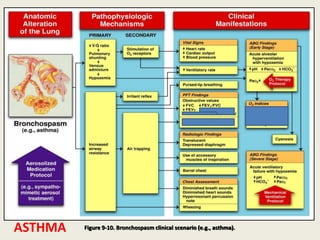
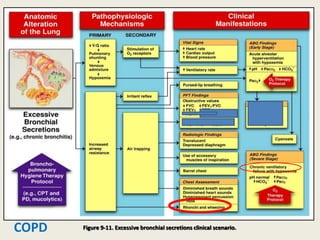
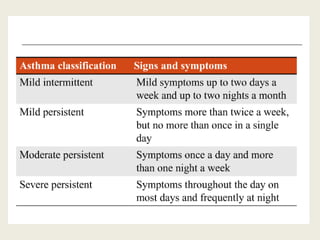
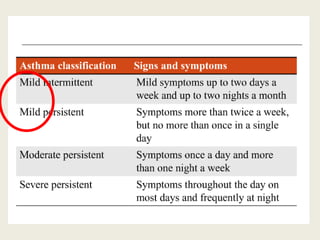
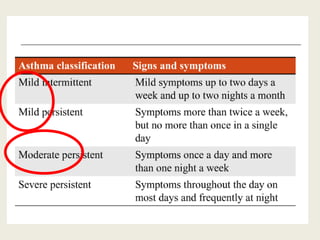
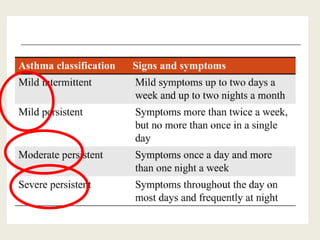
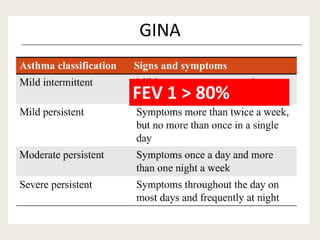
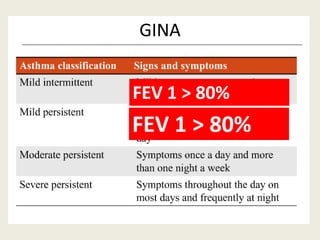
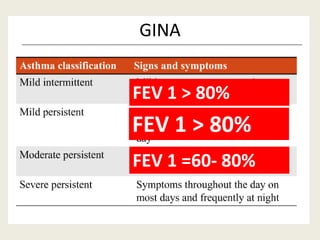
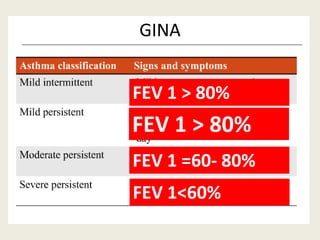
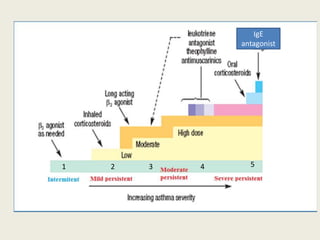
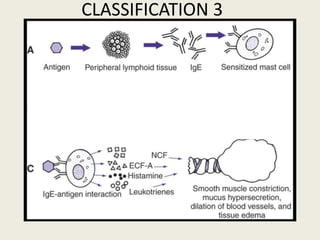
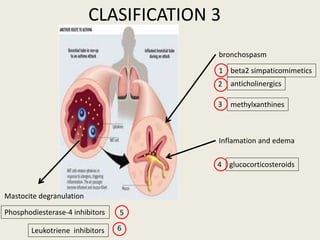
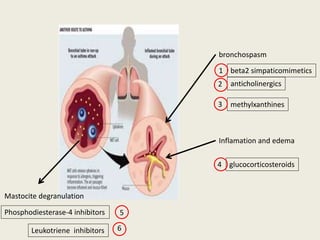
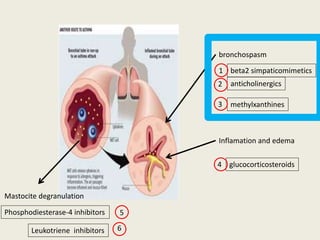
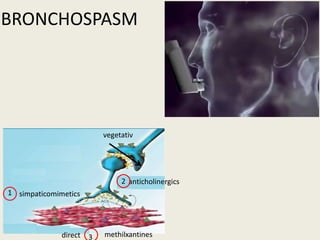
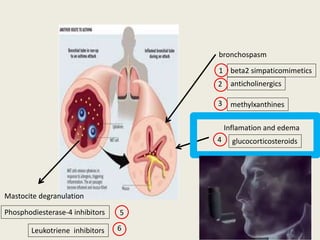
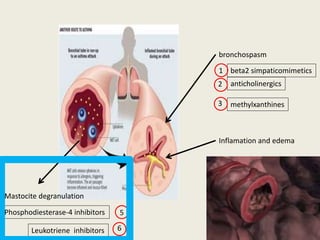
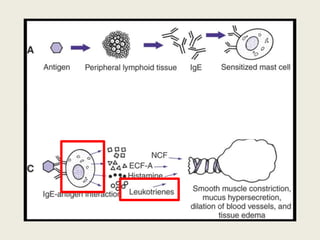
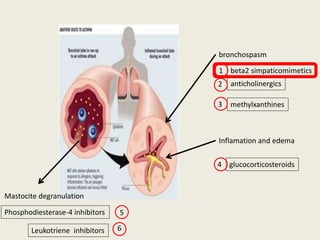
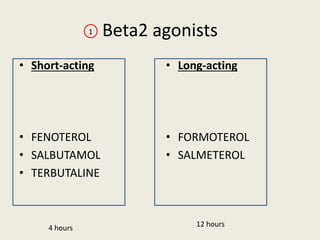
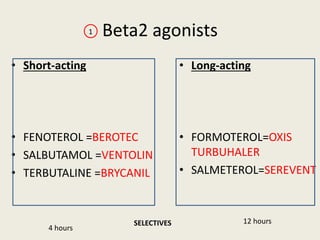
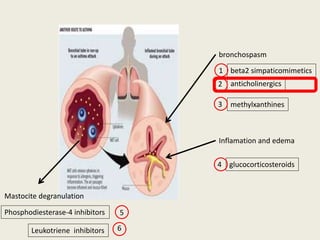
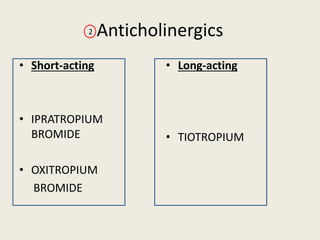
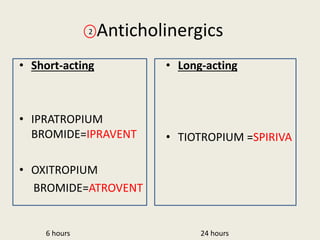
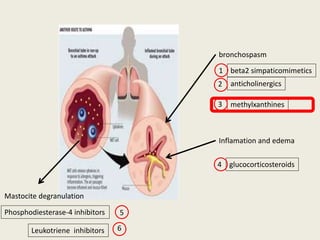
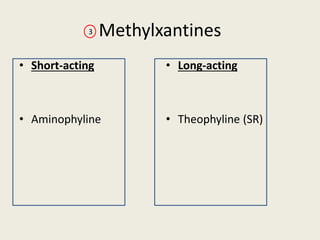
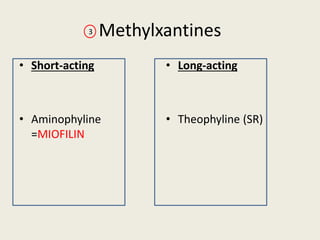
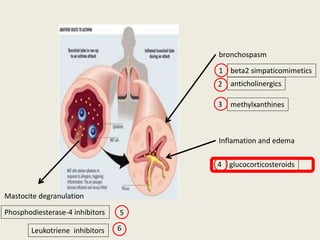
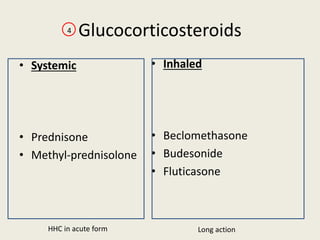
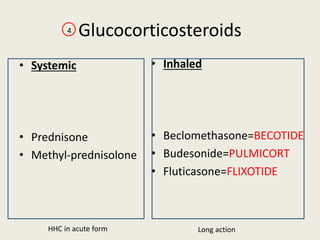
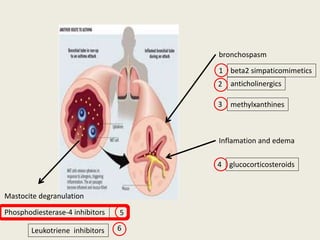
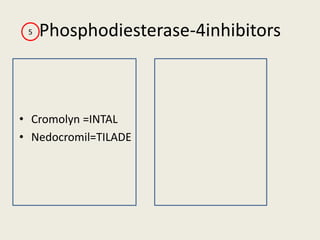
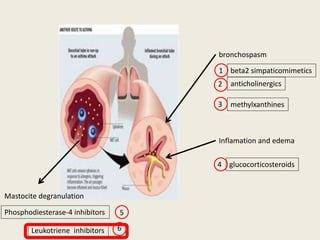
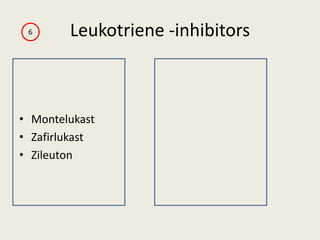
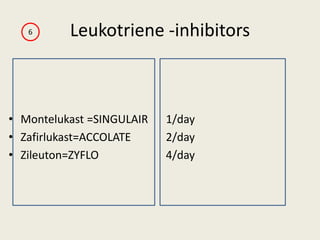
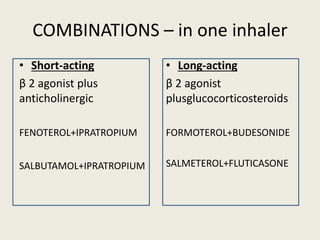
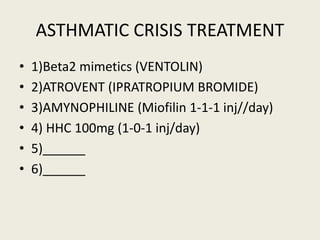
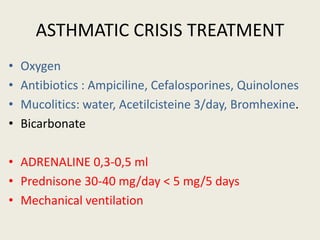
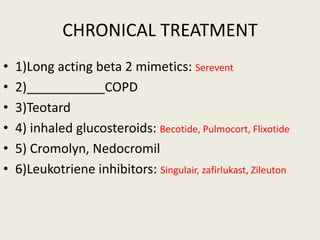
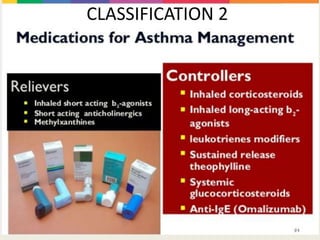
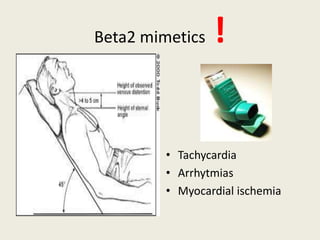
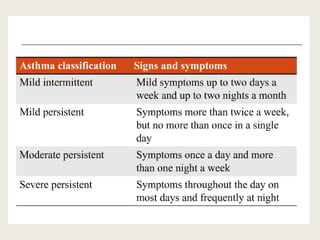
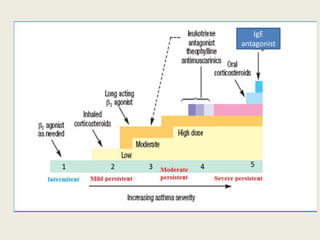
This document summarizes information about two asthma case studies. For case one, it describes a 66-year-old man who stopped his blood pressure medication and presented with coughing, dyspnea, wheezing and crackles. Tests showed elevated BNP and arterial blood gases indicative of mild to moderate asthma. For case two, it describes a 16-year-old girl with a history of asthma who presented with shortness of breath, wheezing and tachycardia. Laboratory tests showed elevated eosinophils. Both cases were diagnosed with acute exacerbation of asthma. The document then provides further details on the definition, causes, symptoms, examinations, tests and treatment of asthma.