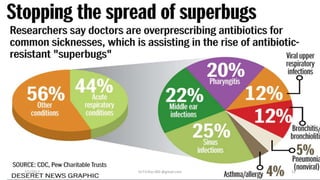
The document discusses the importance and components of antibiotic stewardship programs. It notes that antimicrobial resistance is increasing as development of new antibiotics is slowing. An antibiotic stewardship program aims to optimize antibiotic use, prevent resistance, and improve outcomes. Key components include monitoring antibiotic use, providing education to prescribers, and implementing guidelines and interventions to ensure appropriate antibiotic selection, dosage, and duration. The goals are to improve patient safety, reduce costs, and slow the development of drug-resistant bacteria.
















![Point-of-care interventions can include:
• appropriate use of guidance,
• ➤ indication for antibiotic,
• ➤ choice of agent,
• ➤ route [IV vs. oral] of administration of treatment,
• ➤ timeliness of treatment,
• ➤ likelihood of on-going infection or not,
• ➤ use of investigation,
• ➤ interpretation of microbiology with a view tode-escalation or stopping
therapy,
• ➤ duration of therapy.
7/5/2017 Dr.T.V.Rao MD @gmail.com 19](https://image.slidesharecdn.com/antibioticstewardshipprogram-170705112205/85/Antibiotic-stewardship-program-19-320.jpg)
![Data collection for quality
improvement
• Antimicrobial stewardship is part of many patient safety
programs. To measure the performance of these programs, data is
primarily used for 3 purposes [Solberg et al., 1997]:
• l Accountability (e.g. targets)
• l Improvement
• l Research.
• A range of such measures for antimicrobial stewardship programs
have been proposed. They can be summarized as four types
structural, process, outcomes and balancing (are the changes
causing new problems?)
7/5/2017 Dr.T.V.Rao MD @gmail.com 20](https://image.slidesharecdn.com/antibioticstewardshipprogram-170705112205/85/Antibiotic-stewardship-program-20-320.jpg)