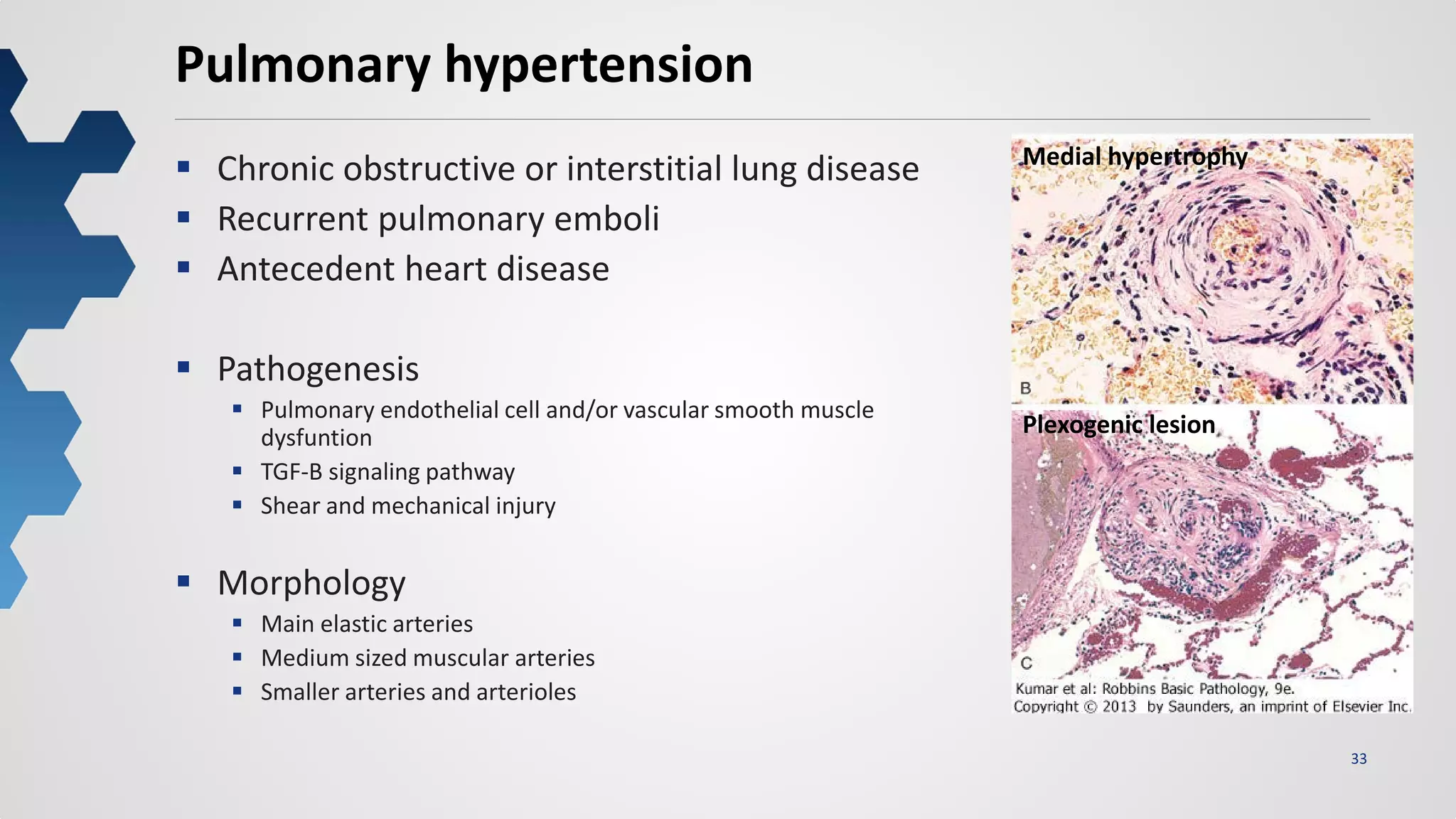
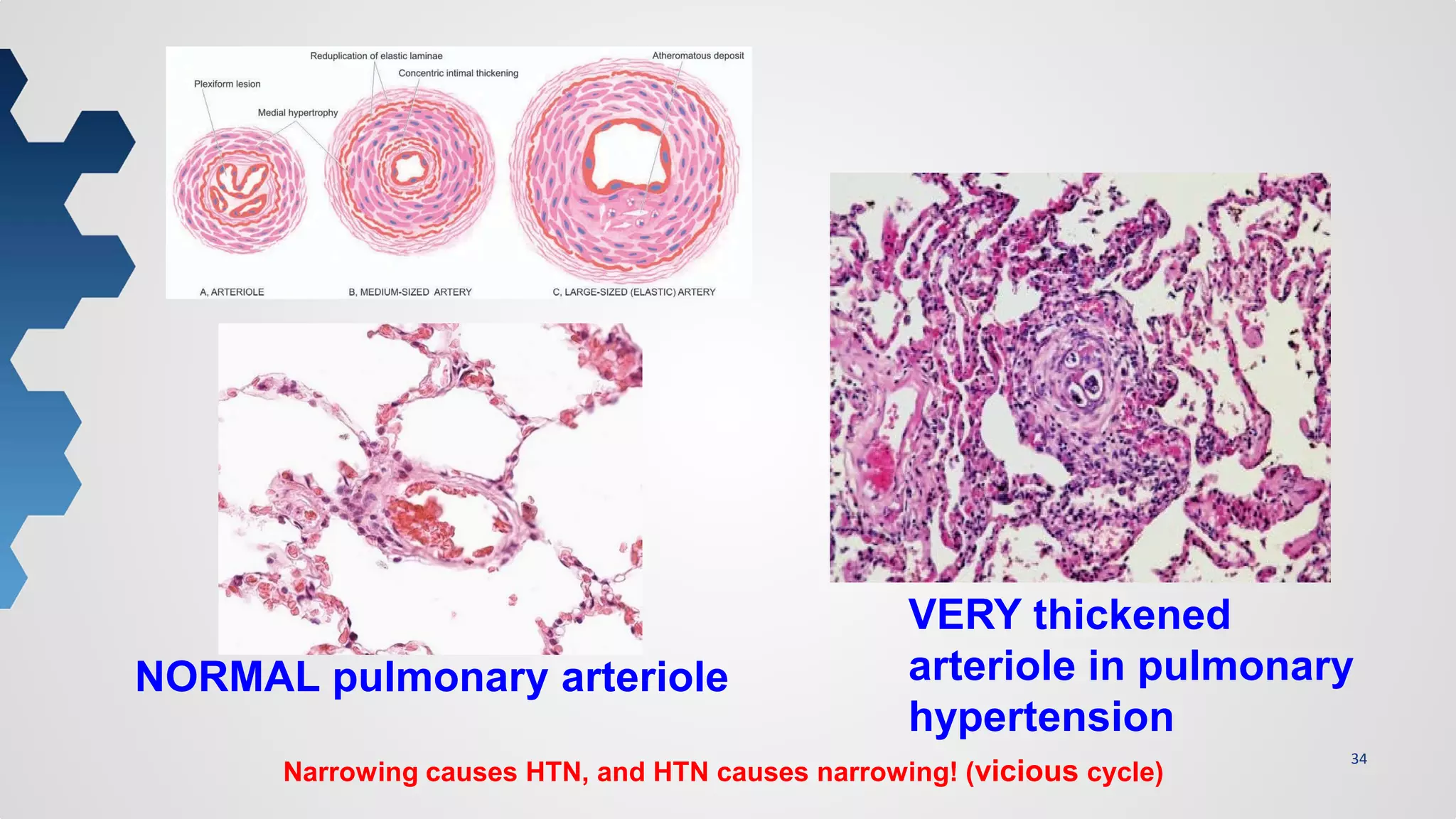
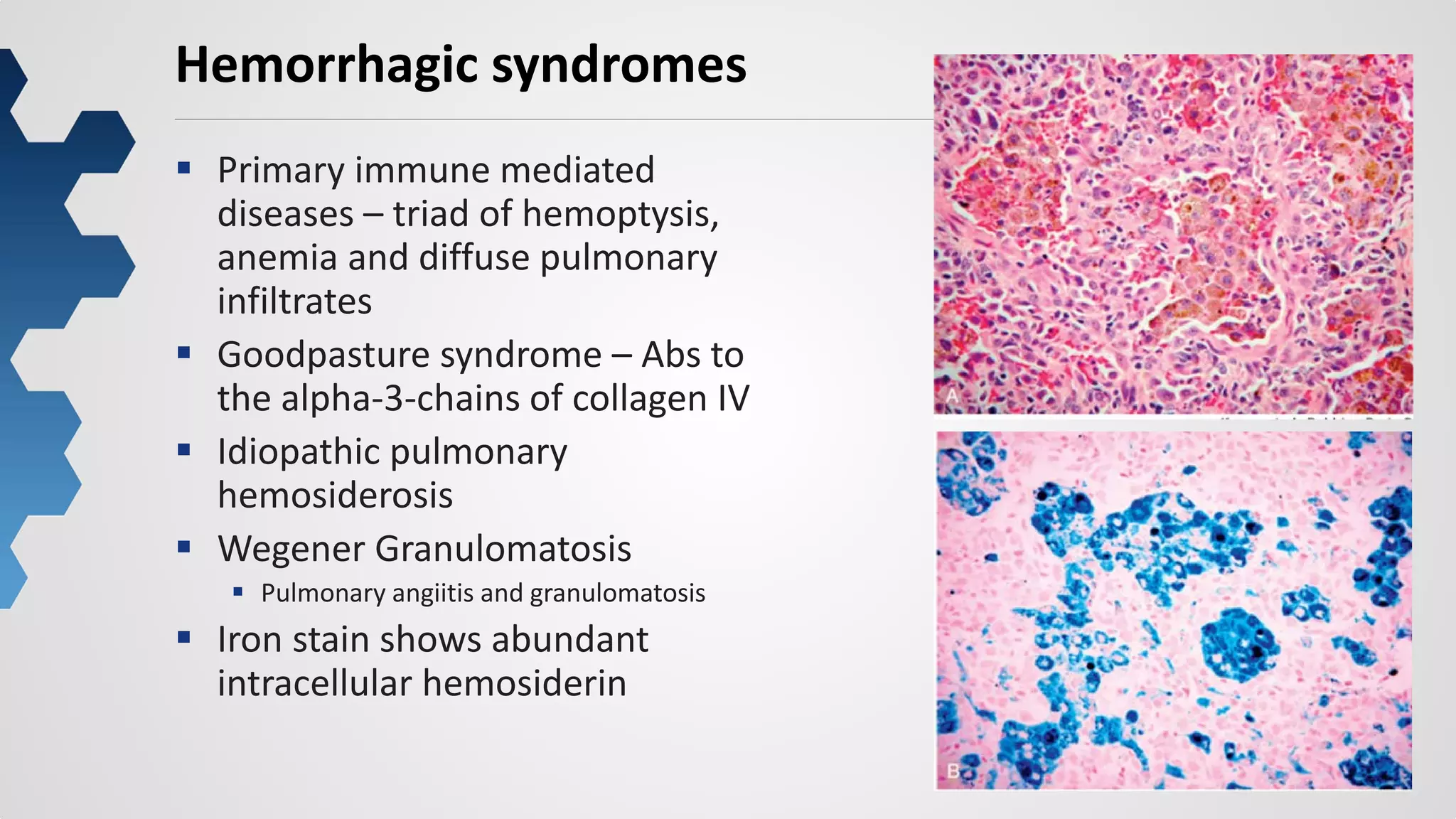
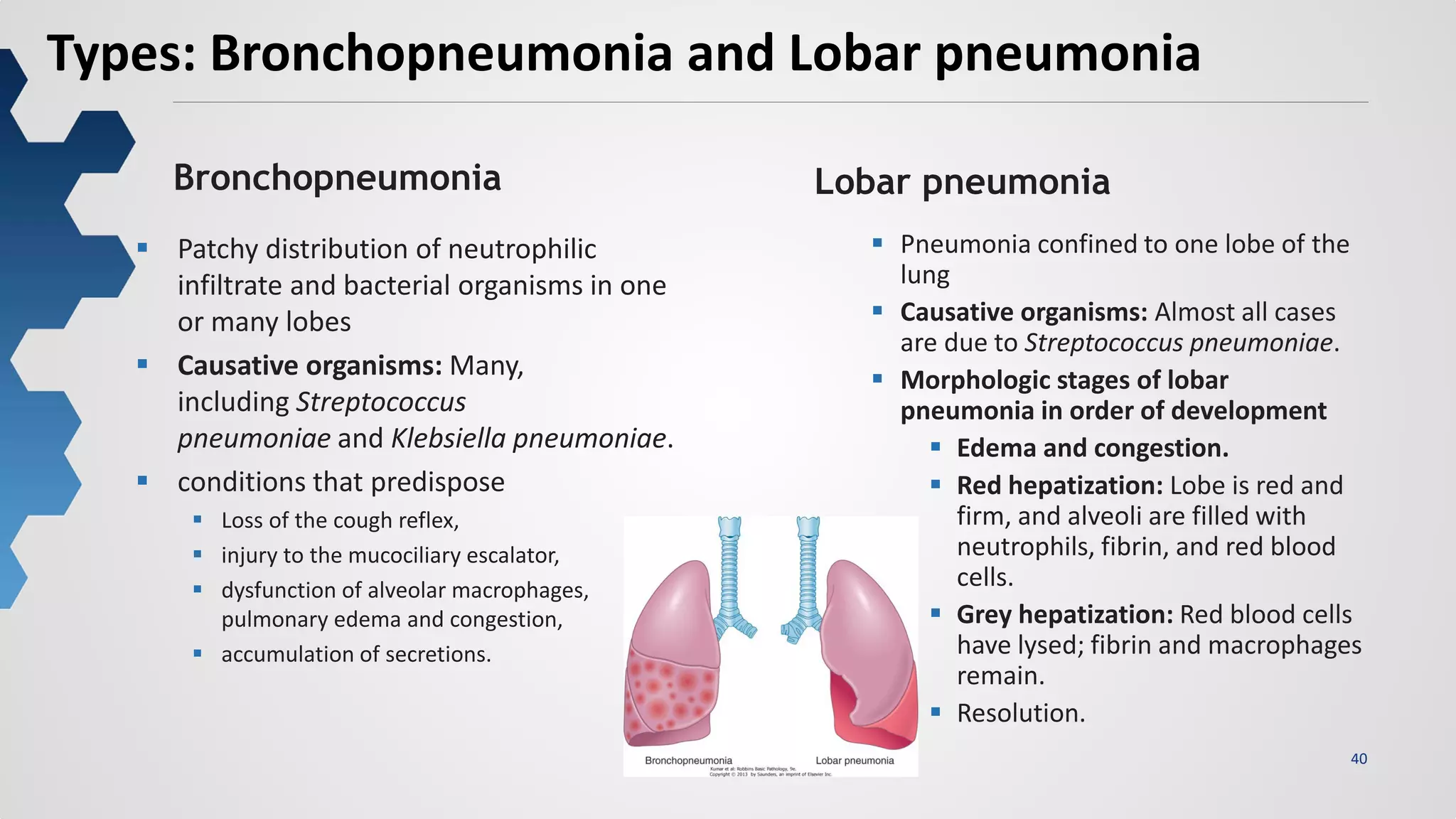
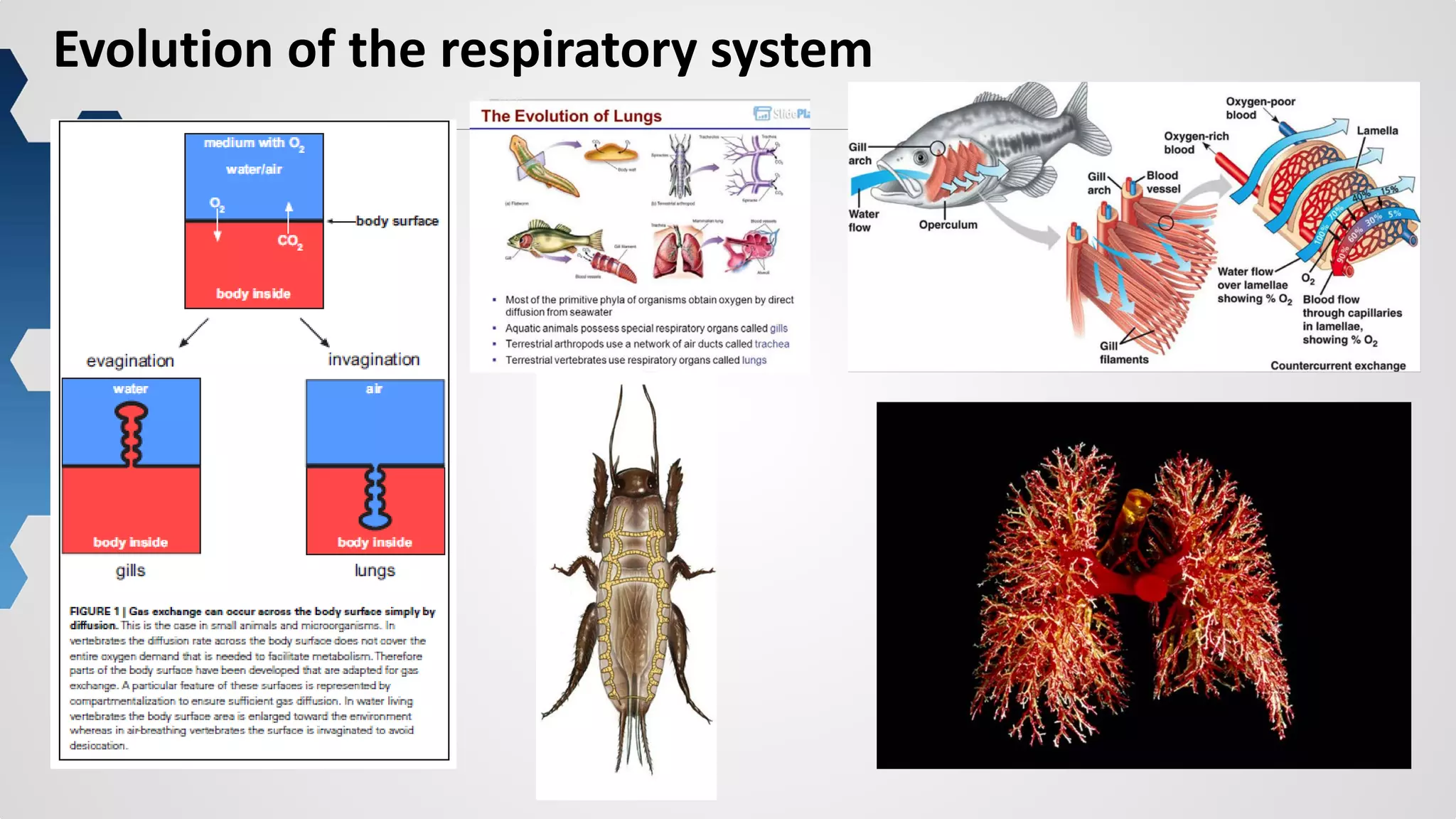
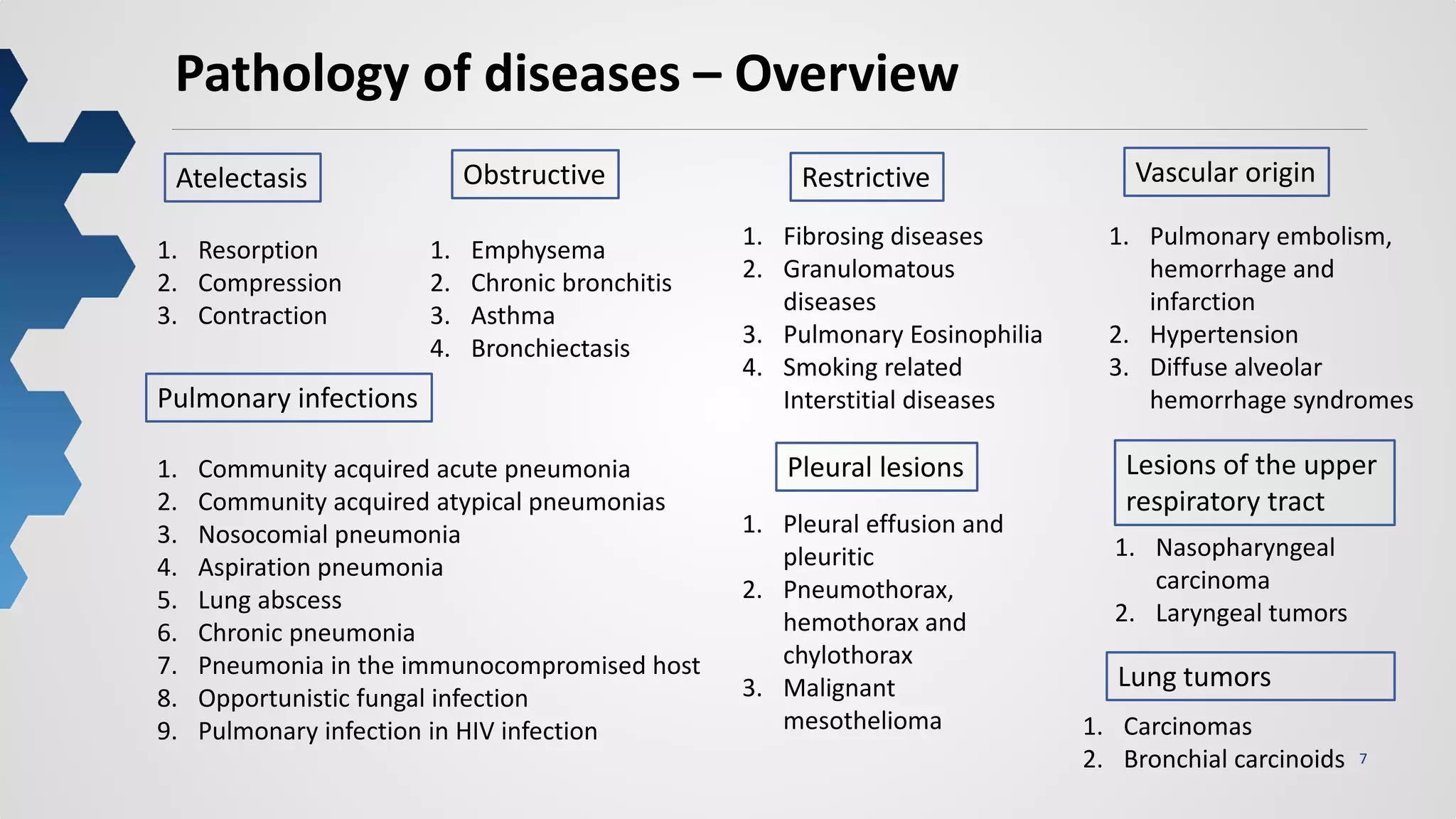
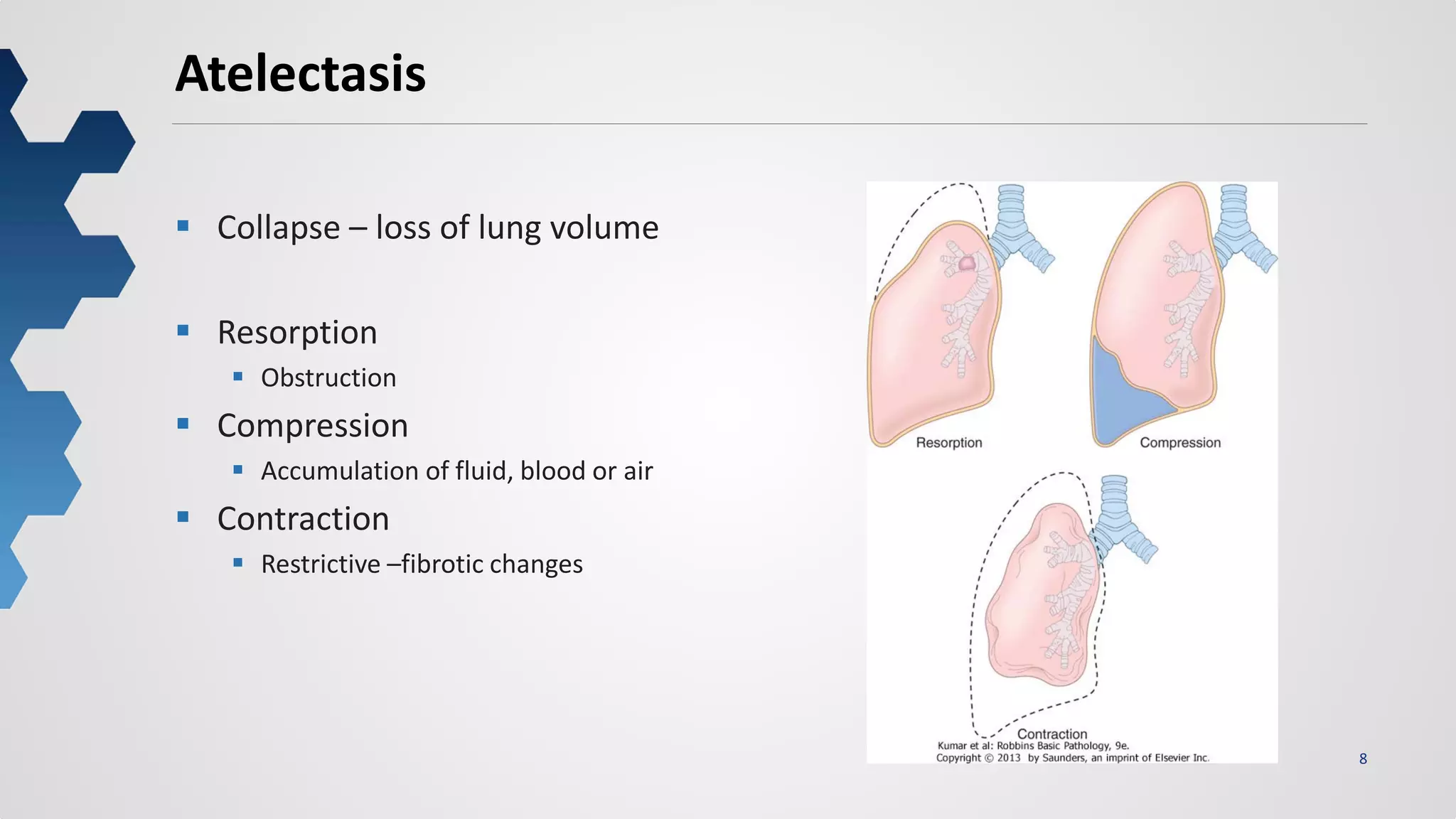
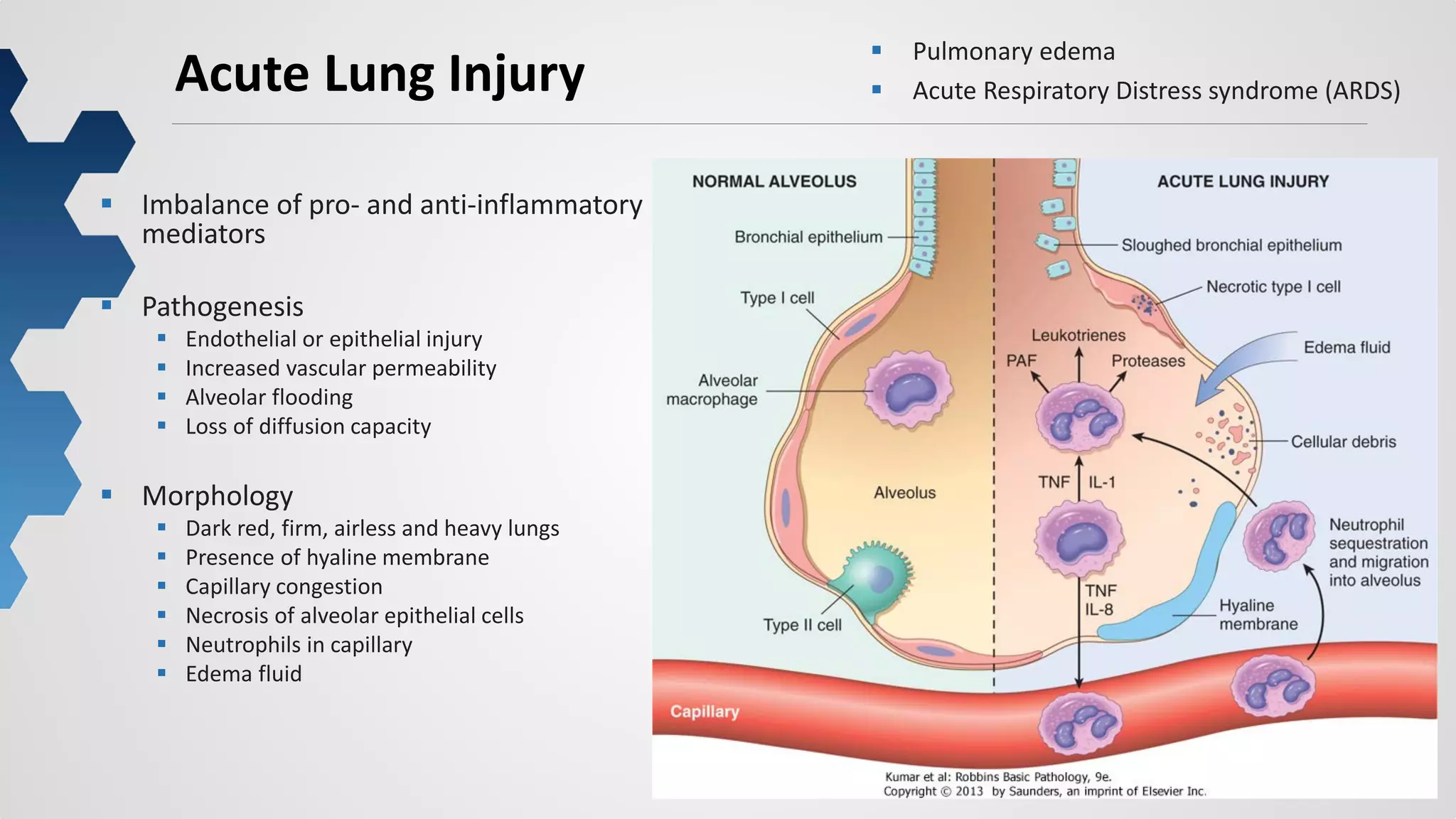
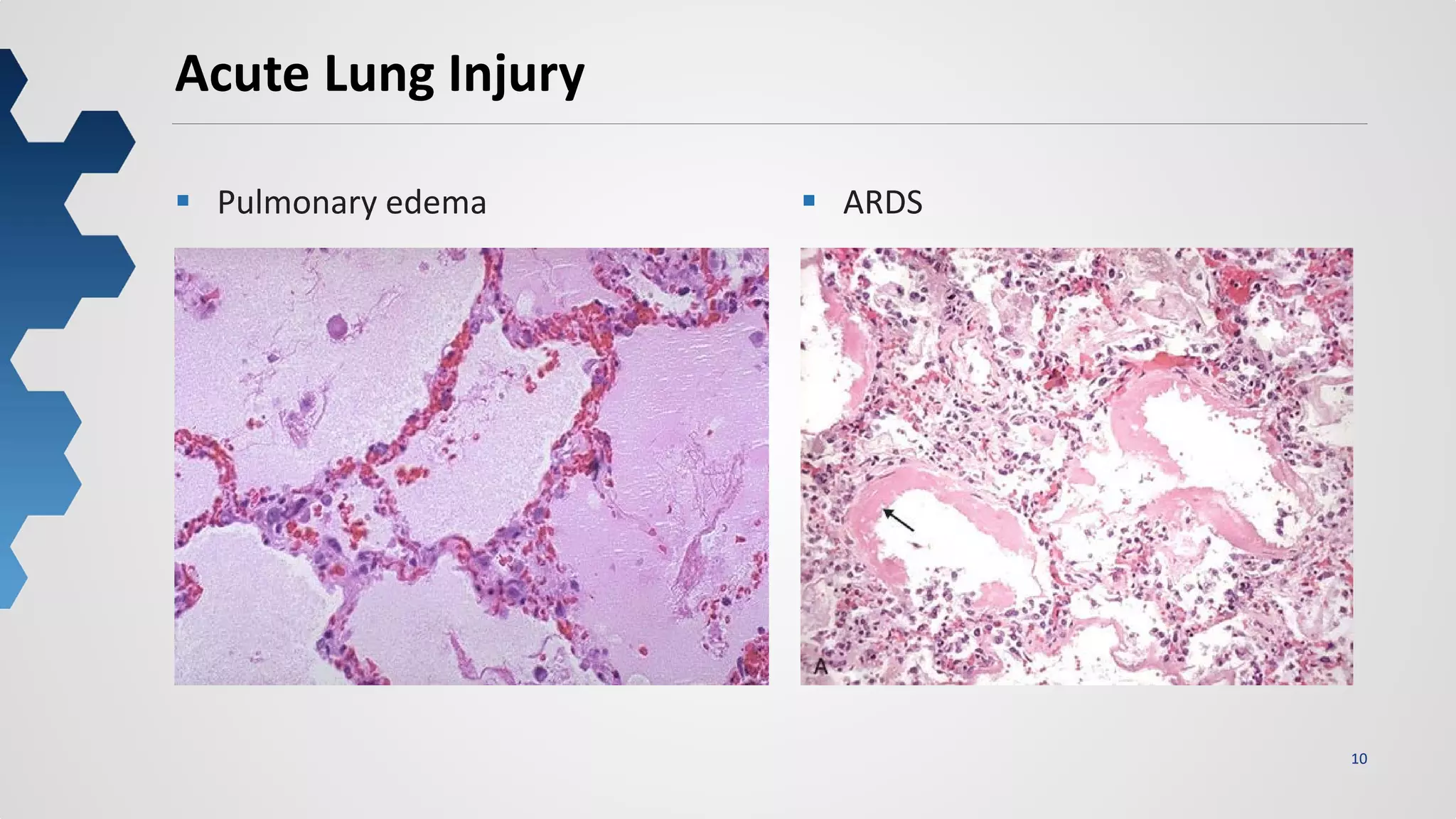
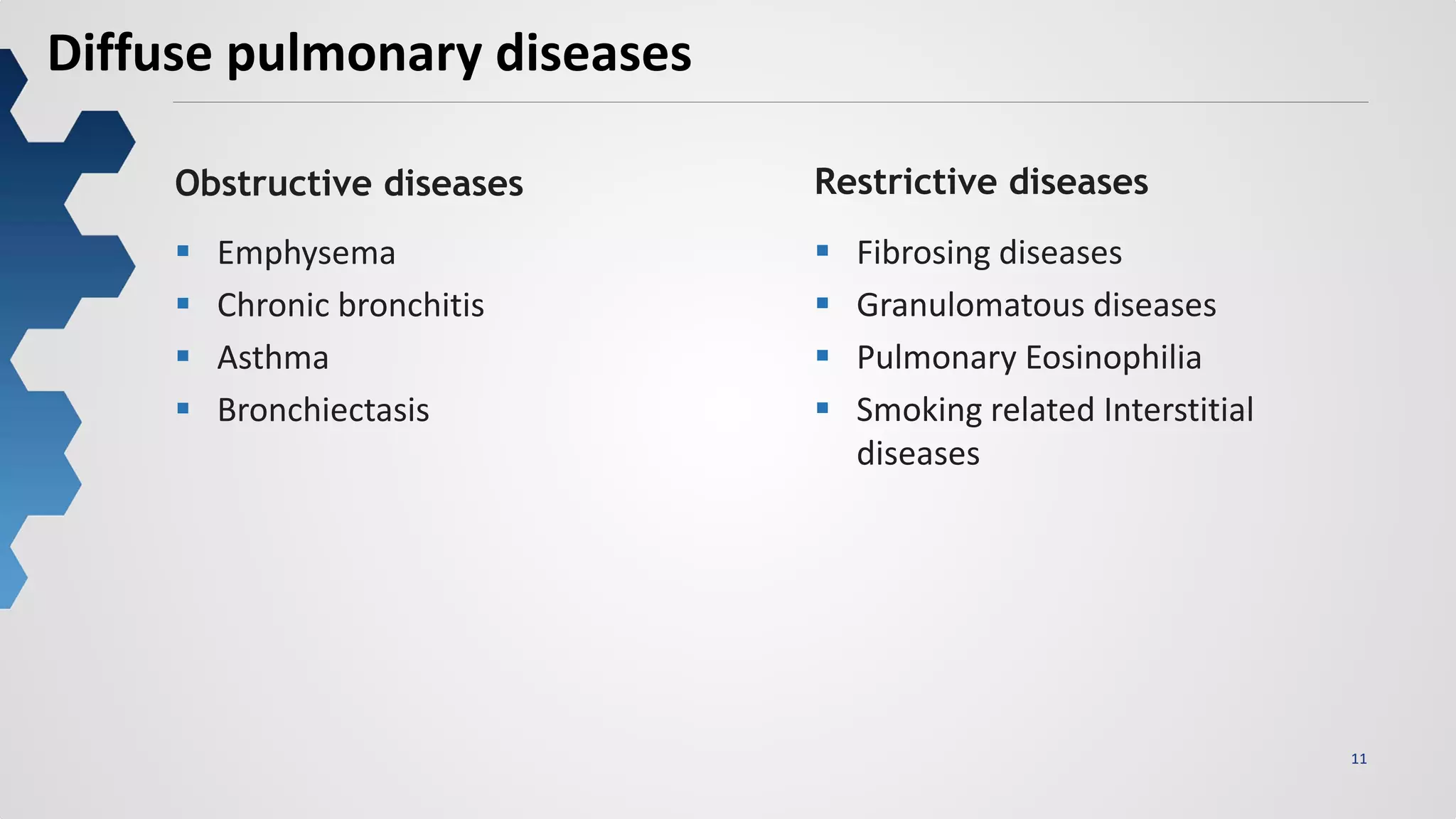
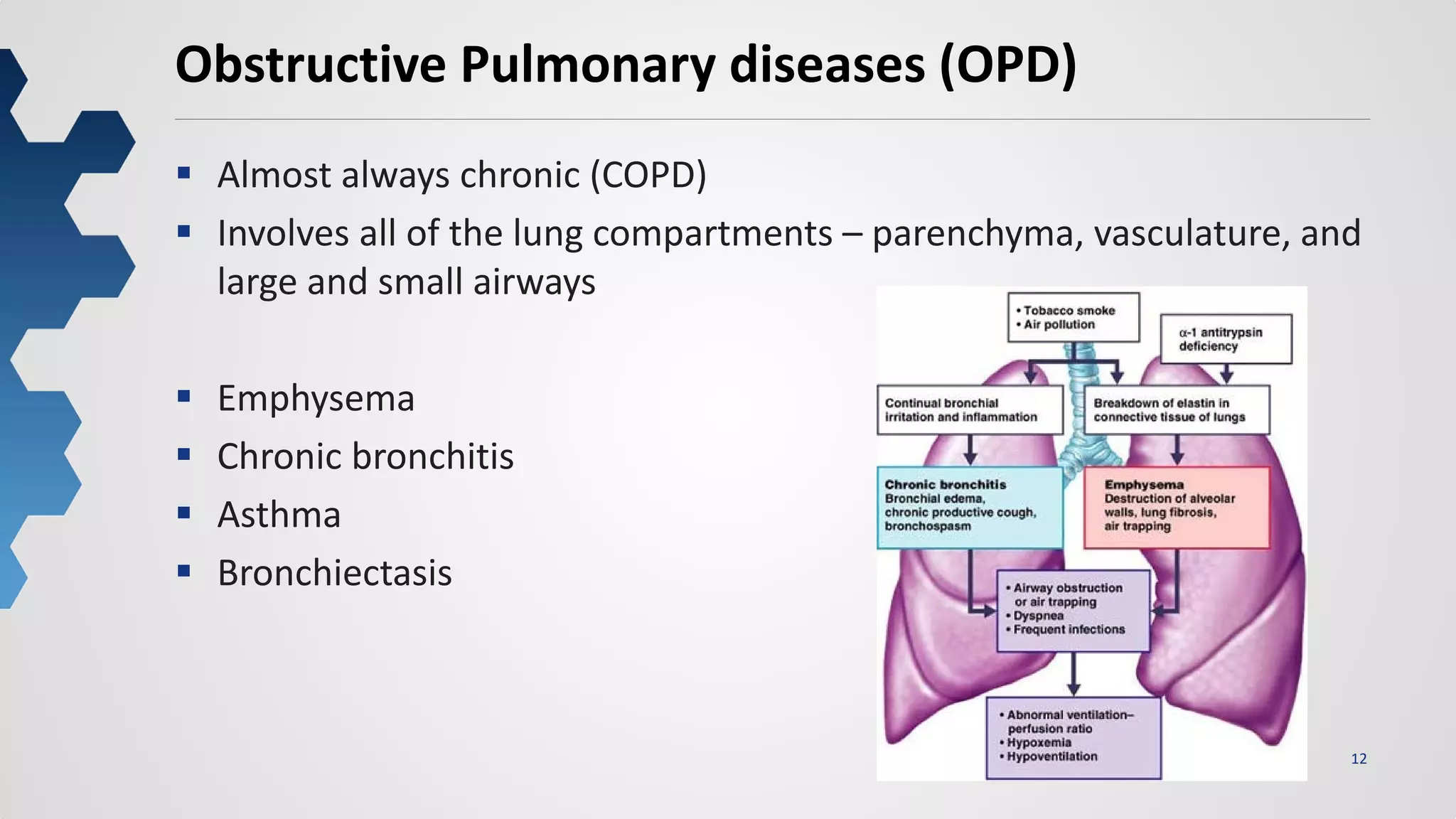
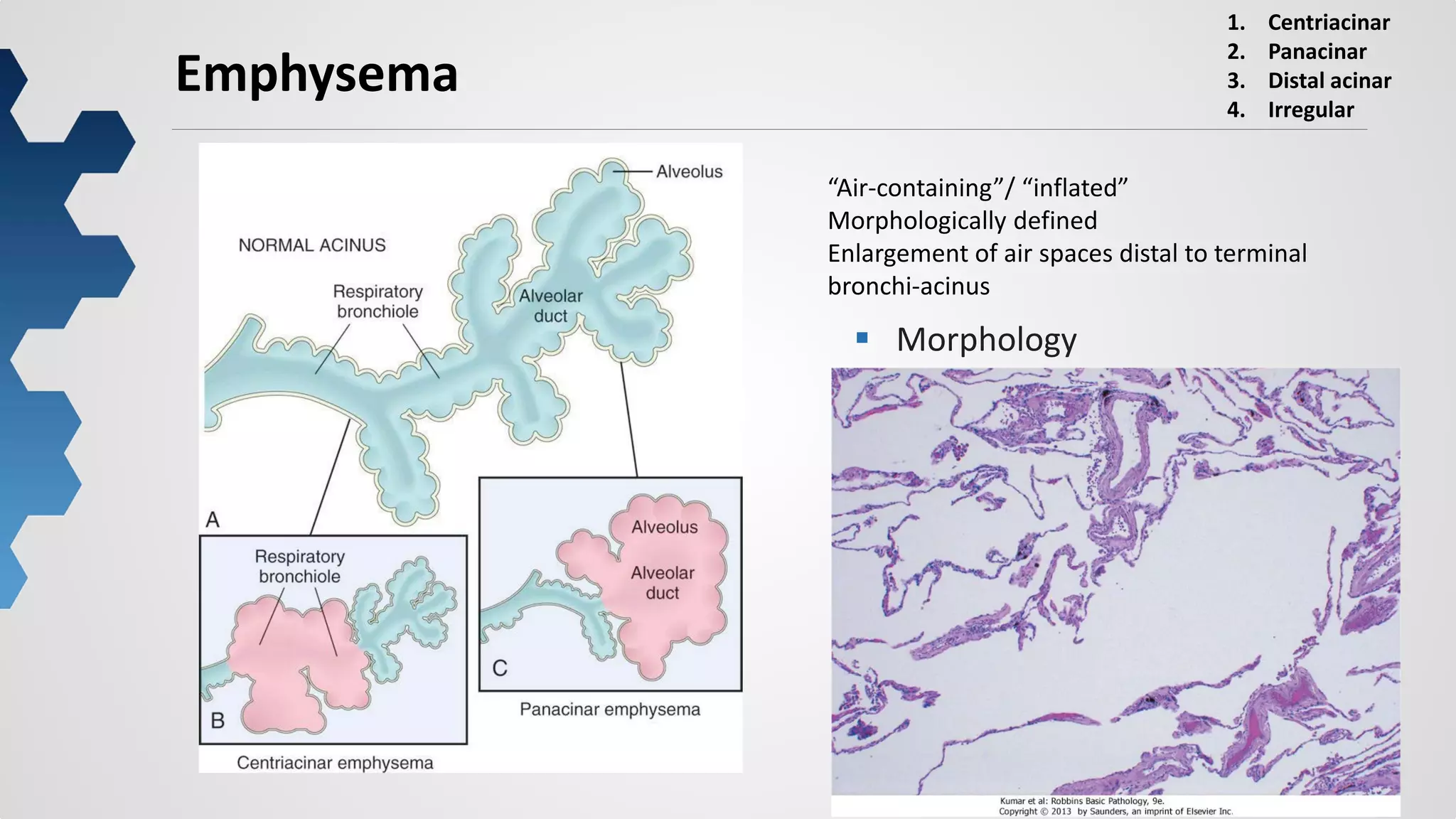
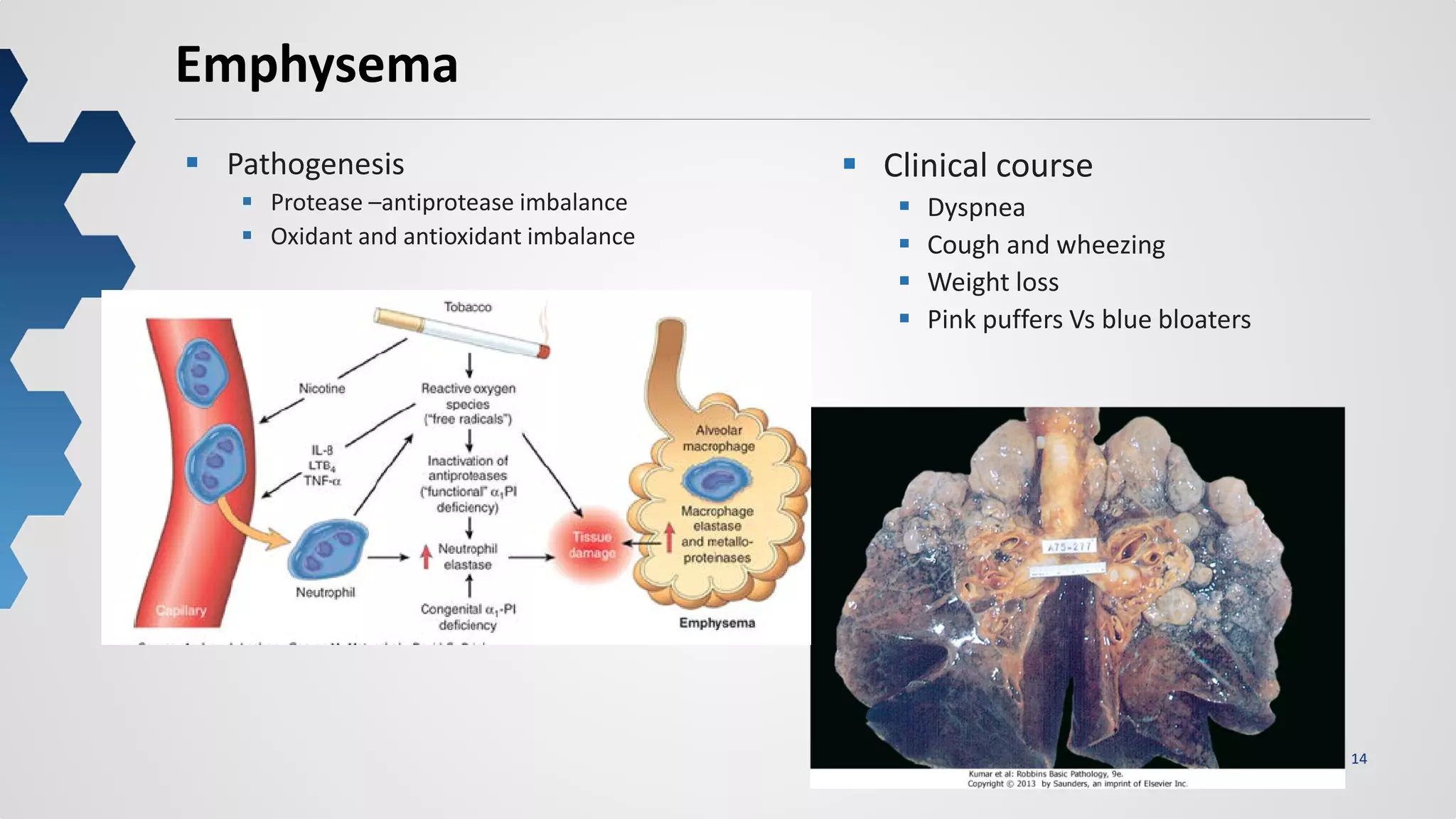
This document provides an overview of the anatomy, histology, and pathology of the respiratory system. It begins with the normal anatomy and histology of the lungs and trachea. It then discusses various pathological conditions including atelectasis, acute lung injury, diffuse pulmonary diseases such as obstructive diseases like emphysema and restrictive diseases like idiopathic pulmonary fibrosis. It also covers pulmonary infections, tumors, and diseases of vascular origin. For each condition, it provides details on pathogenesis, morphology, and clinical presentation.
![32
Pulmonary embolism (PE)
Blood clot(s) migrate from the systemic
circulation to the pulmonary vasculature.
Deep veins of the lower and upper extremities (deep venous
thrombosis [DVT]
Morphology
Size of the embolic mass
General state of circulation
Saddle embolus – pulmonary arteries
Stasis Immobility
Bed rest
Anesthesia
Congestive heart failure/cor pulmonale
Prior venous thrombosis
Hypercoagulability Malignancy
Anticardiolipin antibody
Nephrotic syndrome
Essential thrombocytosis
Estrogen therapy
Heparin-induced thrombocytopenia
Inflammatory bowel disease
Paroxysmal nocturnal hemoglobinuria
Disseminated intravascular coagulation
Protein C and S deficiencies
Antithrombin III deficiency
Vessel wall injury Trauma
Surgery
Large saddle embolus
from the femoral vein-
impacted in the main left
and right pulmonary
arteries](https://image.slidesharecdn.com/lecturethelungspreethisurendranss-180228082219/75/Lecture-the-lungs-preethi_surendran_ss-32-2048.jpg)